What is the Pelvic Floor?
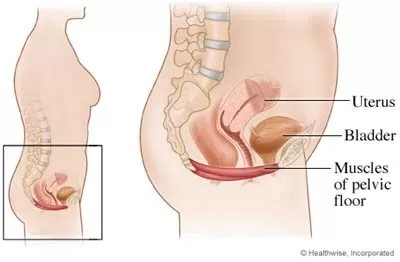
The pelvic floor is a set of muscles that spread across the bottom of the pelvic cavity like a hammock. The pelvic floor has three openings that run through it, the urethra, the vagina, and the rectum. The functions of the pelvic floor include:
- Supporting the pelvic organs, specifically the uterus, the bladder, and the rectum
- To help provide sphincter control for the bladder and bowel
- Withstanding increases in pressure that occur in the abdomen such as coughing, sneezing, laughing, straining, and lifting
- To enhance the sexual response
What causes pelvic floor dysfunction?
The pelvic floor becomes dysfunctional in many women when there is an imbalance in the joints, muscles, and connective tissue integrity.
- Weak pelvic floor muscles: contributing to stress incontinence, urge incontinence, and pelvic organ prolapse.
- Tight pelvic floor muscles: contributing to Urinary and Fecal Urgency, Urge Incontinence, Chronic Pelvic Pain, Dyspareunia, Vaginismus, Vulvodynia, Pudendal Neuralgia, Interstitial Cystitis and Chronic Prostatits.
One of the most commonly seen conditions by pelvic physiotherapists is stress incontinence in women.

What is Stress Urinary Incontinence?
Stress urinary incontinence is the involuntary release of urine during laughter, coughing, lifting of objects or any movement that increases pressure on your bladder. When the bladder is full, the muscles in the wall of your bladder contract forcing urine through the urethra and out of your body. Sphincter muscles and pelvic floor muscles keep the urethra closed to avoid leakage of urine. These muscles relax at the same time the bladder contracts in order to allow urine to exit your body.
Causes of stress incontinence:
Hormonal changes:
During the week before your menstrual cycle, estrogen levels fall, causing symptoms of stress urinary incontinence to worsen. Additionally, as a woman goes through menopause, estrogen levels also fall causing the pelvic floor muscles to weaken.
Pregnancy:
If you are pregnant, you may experience stress urinary incontinence due to hormonal changes and the enlarging size of the uterus. During pregnancy, estrogen levels are lower, leading to less muscular strength in the sphincter and pelvic floor muscles. Additionally, as the fetus grows extra weight is placed on your bladder.
Childbirth:
Vaginal delivery can damage your pelvic floor muscles making urine leakage more likely. The supporting tissues of your bladder can also be damaged during vaginal delivery causing a cystocele, or prolapse of your bladder, symptoms of which include urinary incontinence. You may not know you have suffered damage to your pelvic floor until after you have gone through menopause, when the pelvic floor muscles are further weakened due to a fall in estrogen levels.
Hysterectomy and other surgery:
The bladder and uterus are very close together and have common supporting ligaments and muscles. Surgery to, or removal of your uterus as in a hysterectomy, risks damage to the supporting structures of your bladder. If these supporting structures are damaged, a cystocele is likely to occur. Symptoms of a cystocele include urinary incontinence.
Illnesses:
When you are ill and suffering from severe coughing, the pelvic floor muscles may fatigue and allow temporary stress incontinence due to an increase in abdominal pressure experienced while coughing.
Obesity:
Obesity can increase the abdominal pressure on the bladder leading to urinary incontinence.
Neurological damage:
Any neurological disorder such as multiple sclerosis, Parkinson’s disease or stroke can cause urinary incontinence by interfering with the nerve signals that control your bladder. Additionally, if the nerves that supply your bladder or pelvic floor muscles are damaged, urinary incontinence may also result
How is Stress Urinary Incontinence treated?
Treatments of stress urinary incontinence are individual based. The following should be considered:
Pelvic floor muscle strengthening:
Strengthening the supporting muscles of your bladder is very effective inhelping stress urinary incontinence.
Bladder training
Bladder training involves learning to delay the urge to urinate. You areinstructed to breathe deeply, relax, and distract yourself with another activitywhen you feel the urge. The initial goal is to delay urination by increments and eventually once every2 to 4 hours.
Pessary
Pessaries can help when a cystocele or prolapsed bladder is the cause forurinary incontinence. A pessary is a device of various shapes and sizes that isplaced in the vagina to support the bladder and keep it in place.
Surgery
For severe cystoceles, or bladder prolapses, surgery is needed in order tocorrect the position of the bladder and help with urinary incontinence.
Important Tips
- Avoid constipation. Repeated straining can have a very damaging effect on the pelvic floor muscles.
- It’s important for women to be active. Regular exercise and recreational sporting activities play a key role in keeping women fit and healthy well into old age
- Drink plenty of water
- Learn to tighten your pelvic floor muscles before you cough, sneeze or lift heavy items.
To get your pelvic health assessed, schedule a consultation with a pelvic floor physiotherapist at Triangle Physiotherapy and Rehabilitation!
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.