
Pelvic Floor Physiotherapy
DID YOU KNOW?
1 in 4 women are incontinent.
1 in 9 men are incontinent.
1 in 6 children under the age of 17 struggle with incontinence.
Only 1 in 12 people seek out treatment because they are embarrassed to talk about it, or don’t know that help is available.

Incontinence is just one of many Pelvic Floor conditions that can be treated by a trained Pelvic Floor Physiotherapist at Triangle Physiotherapy. We provide a comfortable & positive environment to encourage patients to successfully complete a pelvic health physiotherapy program. Our state-of-the-art facilities have private rooms for pelvic health treatments to put patients at ease when addressing a sensitive issue such as this.
Your pelvic health physiotherapist offers you valuable advice and an individually tailored treatment program to help treat your pelvic problems. Some of the pelvic issues we treat at our clinic are:
WOMEN'S PELVIC HEALTH
MEN'S PELVIC HEALTH
KID'S PELVIC HEALTH
TRANS AND GENDER-DIVERSE PELVIC HEALTH
WOMEN’S HEALTH
 Vaginismus
Vaginismus
Vaginismus is a condition where the muscles surrounding the vaginal opening involuntarily contract, leading to
sensations of discomfort, burning, and pain, and making it difficult or impossible to insert objects like tampons,
fingers, or a penis. The severity of symptoms can vary, ranging from mild discomfort to complete closure of the vaginal
opening, which may feel like a physical barrier. This condition can occur at any point in a person's life and is
frequently associated with ongoing sexual problems.
Vaginismus is categorized into two main types:
1. primary vaginismus and secondary vaginismus. Primary vaginismus is a lifelong condition that manifests from the first attempt at vaginal insertion, causing symptoms such as discomfort, burning, or pain with the use of tampons, fingers, or a penis.
2. In contrast, secondary vaginismus is a condition that appears later in life after a period of successful and painless vaginal penetration with objects such as tampons, fingers, or a penis.
Treatment for vaginismus may include:
1. Education regarding the cause of your symptoms and what you can do to help yourself
. Sympathetic downregulation training
3. Manual therapy to release tight structures
4. Dilator therapy
5. Possible referral to a sex therapist if appropriate to address underlying psychosocial causes Dyspareunia
Dyspareunia
Dyspareunia, a condition commonly referred to as painful intercourse, is a widespread pelvic health issue that can significantly affect an individual's life. It encompasses the discomfort experienced before, during, or after sexual penetration and can impact both men and women.
Although dyspareunia can stem from various causes, it is often associated with factors like pregnancy, childbirth, genitourinary or abdominal surgery, trauma, hormonal imbalances, stress, anxiety, and excessive tension in the pelvic floor muscles.
However, people suffering from painful intercourse need not despair, as Pelvic Health Physiotherapy can offer assistance, regardless of the source of the pain.
Treatment for dyspareunia may include pain management strategies, sympathetic down-regulation, manual therapy and exercises. Dysmenorrhea
Dysmenorrhea
Dysmenorrhea is a medical condition characterized by pain experienced before or during menstrual periods. The symptoms
of dysmenorrhea can begin immediately after ovulation (mid-cycle) and continue until the end of menstruation. A typical
menstrual cycle begins on the first day of bleeding and ends on the first day of the following bleeding. On average, a
menstrual cycle can last anywhere between 28 to 35 days.Treatment:
Visiting a physiotherapist may alleviate the symptoms of dysmenorrhea. During the assessment, the physiotherapist will evaluate the muscles and connective tissues in your abdomen, pelvic girdle, and pelvic floor. Additionally, they can instruct you on how to unwind these muscles, utilize deep breathing, and other techniques to help you manage stress more effectively. Endometriosis
Endometriosis
Endometriosis is a medical condition in which the tissue that typically lines the uterus (known as endometrial tissue) starts to develop outside of the uterus. This condition affects around 10% of women who are in their reproductive years, including teenagers.
Typical indications of endometriosis comprise menstrual pain, though discomfort may arise at other points during the menstrual cycle like ovulation, as well as pain during bowel movements and sexual intercourse. Other symptoms include bloating in the abdominal region, heavy menstrual bleeding, and fatigue.
Individuals who experience pelvic pain, with or without endometriosis, may receive multidisciplinary treatment, which involves consulting a counselor, physiotherapist, and dietician. This approach enables them to address various factors that contribute to their condition. The treatment may encompass pain education, cognitive-behavioral therapy, mindfulness techniques, pelvic physiotherapy, and dietary modifications to alleviate sensitivity.
There is a growing interest in Canada to develop more programs that cater to pelvic pain patients and offer them the necessary assistance. Pelvic Organ Prolapse
Pelvic Organ Prolapse
Pelvic organ prolapse is characterized by the movement of the pelvic organs (including the bladder, urethra, uterus, vagina, rectum, or small intestine) toward or through the vaginal or anal opening. This condition is subjective, as the degree of prolapse may not always align with the symptoms experienced. Some women may not experience any symptoms at all. Treatment is typically based on the level of discomfort caused by the symptoms, rather than the degree of prolapse. It is worth noting that pelvic organ prolapse is not a disease, but rather a functional issue.
The management of pelvic organ prolapse can significantly reduce, alleviate, or control the symptoms associated with the condition. Physiotherapists address several strategies to manage pelvic organ prolapse, including inner core training, pelvic floor strengthening, postural correction, constipation/toileting education, symptom management education, exercise prescription, and pessary education and fitting. If physiotherapy treatment does not produce satisfactory results, corrective surgery may be considered as a last resort, although most experts recommend reserving surgery as a final option. Urinary Incontinence
Urinary Incontinence
The inability to maintain control urine leakage as a result of a stress event i.e. laughing (Stress Incontinence), or a
sudden need to immediately urinate (Urge Incontinence). 50% of women will at some point in their life experience some
form of UI. This can severely impede an individual’s social and physical activities.Common Misconceptions:
· It is normal to have urinary leakage after childbirth
· It is normal to have urinary leakage as you age
· There is nothing you can do about urinary leakage
· Kegels will solve all incontinence issues
Risk Factors:
Female -
· Obesity
· Post menopause (hormone changes) - Over 40 (1 in 3)
· Pregnancy and Childbirth
· Multiparous: having had more than one child
· Obstetric trauma (forceps, suction, tearing)
· Gynecological or Urinary surgery
· Chronic Illness
· Medication
· Smoking
· Chronic straining
· Radical Prostatectomy for men
· Prostate enlargement
The muscles that comprise the pelvic floor are vital in maintaining urinary continence. They act as a sphincter, and provide support and stability. While a weak pelvic floor could be a cause for UI, it is not always the answer. Individuals at the other end of the spectrum with a hypertonic pelvic floor can also experience UI. Therefore, a thorough assessment by a pelvic floor physical therapist is needed to determine the root cause of your UI and create a personalized treatment plan. Interstitial Cystitis
Interstitial Cystitis
Interstitial cystitis (IC)/painful bladder syndrome (PBS) is a chronic bladder health issue. It is a feeling of pain and pressure in the bladder area. Along with this pain are lower urinary tract symptoms which have lasted for more than 6 weeks, without having an infection or other clear causes.
Symptoms range from mild to severe. For some patients, the symptoms may come and go, and for others, they don't go away. IC/BPS is not an infection, but it may feel like a bladder infection. Women with IC/BPS may feel pain when having sex. Some people with IC/BPS may have other health issues such as irritable bowel syndrome, fibromyalgia, and other pain syndromes.Symptoms:
· Bladder pain
· Pain/burning with urination
· Increased urinary urgency
· Increased urinary frequency
· Vaginal/rectal/penile pain
· Pain with sex
There is an association of myofascial trigger points in patients with ICS as well as connective tissue dysfunction which can be helped by pelvic floor physiotherapy.
Your physiotherapist will conduct a thorough external and internal evaluation to determine the tone of your muscles as well as the presence or absence of trigger points.Treatment may include:
· Myofascial release
· Trigger point release
· Therapeutic exercise
· Desensitization of the central nervous system
· Bladder retraining
You may also be referred to our naturopathic doctor who will assess your diet and provide nutritional counseling to eliminate irritants. Diastasis Recti
Diastasis Recti
A Rectus Diastasis is a separation in the 6-pack muscle, the rectus abdominis.
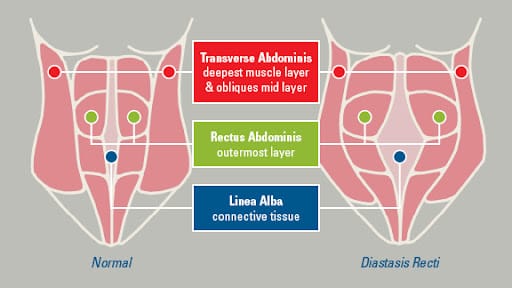
How does it occur?
It most often occurs during pregnancy. Sometimes it will spontaneously correct following birth, but it does not always. It can also occur with overstretch of abdominal musculature.Why is it a problem?
There is no pain with this condition. However, the abdominal wall and the core will become weak. Your abdominals work with your pelvic floor, so a separation of your rectus abdominis muscles can make your pelvic floor less efficient and may result in prolapse and incontinence. Your abdominals also work with your lower back musculature, therefore it can lead to lower back pain.How do I know if I have a Rectus Diastasis?
If you lift your head while lying on your back and the center of your belly protrudes out, you may have a rectus diastasis.
It is measured by the number of fingers you can fit between the muscle when lying on your back and lifting your head. Normal is 1/2 a finger above and below the belly button, and one finger at the belly button.How can rectus diastasis be treated?
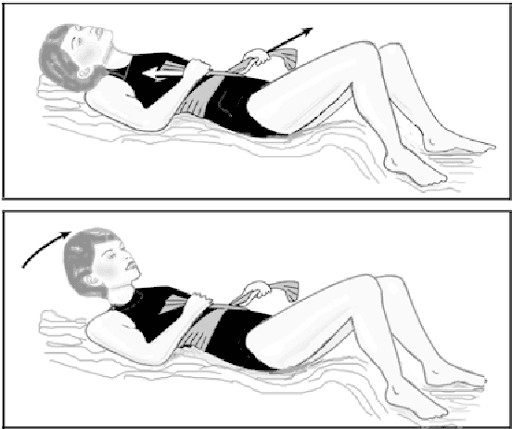
If the abdominal separation is greater than 4 fingers, an abdominal binder is recommended. Our pelvic physiotherapists are also able to help you reduce or eliminate the separation.What type of exercise is recommended to resolve rectus diastasis?
Lie on your back with your knees bent. Place a sheet around your waist, crossed as if tying a knot and pull snug. Raise your head only, chin towards your chest. Hold for a count of 5, exhaling during the count. Lower your head as you loosen your grip on the sheet. Repeat 10-20 times per session, 2 sessions per day. It should be corrected within several weeks. If it does not correct within this time, please see a physiotherapist who specializes in pelvic health.
Contact us if you think you have diastasis recti and would like to book an appointment with one of our experienced pelvic physiotherapists.
 RECTAL AND BOWEL CONDITIONS
RECTAL AND BOWEL CONDITIONS
Constipation is a common gastrointestinal (GI) disorder that causes difficulty with passing stool or reduces the frequency of having a bowel movement. It can be caused by different factors such as dehydration, diet e.g. not enough fibre, or a sedentary lifestyle. However, there are other possible underlying muscular reasons for constipation.
The pelvic floor can be a common culprit for constipation. The pelvic floor is a group of muscles that support the pelvic organs such as the uterus, bladder and rectum. These muscles are important in daily function, which includes bladder and bowel control. They can be either tight or weak which can lead to a variety of issues, one of them being constipation.
Treatment for constipation can include a number of lifestyle modifications such as increased fibre and water intake, and regular exercise. However, consulting with a pelvic physiotherapist can improve outcomes, by creating an exercise program specific to your pelvic floor dysfunction. The need for lengthening versus strengthening of the pelvic floor is determined through internal examination. Another option is seeing a naturopath for ways to adjust your diet accordingly. Quite often, both treatments go hand in hand. PESSARY FITTINGS
PESSARY FITTINGS
A pessary is a small device made of silicone or plastic that is inserted into the vagina to support the pelvic organs.
It can be used to treat pelvic organ prolapse, urinary incontinence, and other pelvic floor disorders. Pessaries come in
different shapes and sizes, and your OB/GYN or pelvic physiotherapist can help you find the one that's right for you.PROGRAM HIGHLIGHTS:
. Extensive 1-hour Initial Assessment
. Detailed history intake of patient’s pelvic issues
. Brief internal and external examination
. Individualized treatment sessions, 30 – 45 minutes in duration
. Recommended 4 – 8 treatments typically 1x/week* (varies from patient to patient)
.Outcomes vary and rely on treatment compliance and active patient participation LABOUR AND DELIVERY - BUMP-IT-UP
LABOUR AND DELIVERY - BUMP-IT-UP
Pelvic physiotherapy can be a valuable tool for preparing for your labour and delivery. It can help to improve the strength and mobility of the muscles and joints in the pelvic area. This can make it easier for the baby to descend through the birth canal during delivery.
Pelvic physiotherapy can help to alleviate common pregnancy-related symptoms such as back pain, incontinence, and pelvic pain. A combination of manual therapy techniques with soft tissue and joint mobilization along with mobility work can be used to alleviate pain in the pelvic area. The physiotherapist can also work on alignment and posture to help prevent injury and reduce discomfort.
Leading up to labour, a pelvic physiotherapist can provide you with a variety of tools to help with pain relief and positioning to improve your experience during labour. One of the common techniques taught to birthing parents at 32 weeks, is the perineal massage to reduce the chance of tearing during delivery. In addition, you would also be taught positions to help reduce discomfort during contractions as well as pushing techniques.
After delivery, a physiotherapist can help restore strength and mobility along with providing education on suitable abdominal and pelvic floor exercises based on weaknesses and tone. Any side effects from delivery such as perineal tearing can also be treated post-partum. PEDIATRIC PELVIC HEALTH
PEDIATRIC PELVIC HEALTH
Pediatric pelvic physiotherapy is a form of physical therapy that focuses on the pelvic region of children and adolescents. This type of therapy helps to improve the function of the muscles, bones, and joints in the pelvic area, which can be impacted by a variety of conditions including constipation, urinary incontinence, and developmental delays. The goal of pediatric pelvic physiotherapy is to improve the child's quality of life by reducing pain, increasing mobility and flexibility, and helping them achieve greater independence in their daily activities.
The pelvic health physiotherapist will use a combination of manual therapy techniques, exercise, and education to achieve these goals. Manual therapy techniques may include soft tissue mobilization, joint mobilization, and manual stretching. Exercises may include strengthening and stretching of the pelvic muscles, balance and coordination exercises, and education on proper posture and body mechanics.
The pelvic health physiotherapist will also educate the child and their parents on proper toileting habits, hydration, and dietary changes to help alleviate symptoms. Additionally, the pelvic health physiotherapist will work with the child's medical team to ensure a coordinated approach to their care.
Overall, pediatric pelvic physiotherapy is a safe and effective way to help children and adolescents with pelvic-related conditions improve their quality of life and reach their full potential.MEN'S HEALTH
 Post-Prostatectomy Incontinence
Post-Prostatectomy Incontinence
Prostate cancer is the most frequent form of cancer among men? In certain instances, a prostatectomy is the preferred method of treatment, which involves removing the prostate. The term "radical prostatectomy" refers to the removal of the entire prostate gland and its surrounding tissues. Although there are various surgical procedures to extract the prostate, they all produce comparable side effects.
During a radical prostatectomy, the prostate, ligaments, and part of the urethra are removed. The bladder neck (where the urethra joins the bladder) and the internal urethral sphincter (the primary sphincter muscle that aids in bladder continence) are changed. Therefore, the body's urinary continence mechanism changes, and frequently, the body has to relearn how to function effectively.
In particular, since the internal urethral sphincter, which plays a significant role in continence, is removed, the body must learn to use and depend on the remaining external urethral sphincter, as well as the rest of the pelvic floor muscles. Pelvic floor physiotherapy can significantly impact one's post-prostatectomy experience, particularly if it is done both before and after surgery. Post-prostatectomy Erectile dysfunction
Post-prostatectomy Erectile dysfunction
Erectile dysfunction (ED) following prostatectomy is a prevalent side effect. Almost all men experience ED immediately post-surgery, and around 50% may have prolonged or permanent ED.
Your physiotherapist will perform a similar assessment and treatment approach for ED as they would for incontinence. This involves evaluating the condition of your pelvic floor muscles and tissues, teaching you the correct way to activate and relax your muscles, and designing a customized exercise program that targets the muscles responsible for achieving and sustaining an erection. The initial focus of the treatment sessions will likely be on the first layer of the pelvic floor muscles since they are crucial to sexual function. Moreover, your physiotherapist may also discuss the use of available aids such as vacuum penile pumps, which can assist in attaining and maintaining an erection. Pelvic Pain
Pelvic Pain
Symptoms you experience may include:
1. Pain in the lower back, abdominal, and pelvic area, including the groin
2. penis, perineum, scrotum/testicles, or rectum
3. Pain with sitting, restricted clothing, or certain exercises
4. Dysuria (pain or burning with urination)
5. Increased urgency/frequency of urination
6. Urinary hesitancy (difficulty initiating urine stream)
7. Urinary intermittency (starting/stopping while urinating)
8. Urinary retention (incomplete urination)
9. Nocturia (frequent nighttime urination)
10. Pain or burning during or after ejaculation
11. Premature ejaculation
12. Erectile dysfunction, specifically pain or difficulty with gaining and maintaining erections along with weaker erectile strength
13. Decreased libido
Treatment:
To address male pelvic pain, a pelvic floor physical therapist will conduct an assessment and provide treatment. During the initial consultation, the therapist will inquire about the patient's medical history and symptoms, evaluate their bladder, bowel, and sexual function, and inquire about any previous medical consultations. In addition, the therapist will conduct a physical examination, evaluating the patient's posture, movement patterns, connective tissues, muscles, joints, and nerves. The therapist will then discuss the results of the examination with you and provide education on pelvic floor anatomy. Based on the assessment, the therapist will propose short-term and long-term treatment goals to alleviate symptoms and pain. In-person visits will usually consist of checking in with whether your symptoms have changed and performing manual therapy as well as myofascial trigger point release to address any connective tissue or musculature restrictions you may have. In addition, techniques to calm down your nervous system will also be taught to you. Trans And Gender-Diverse Pelvic Health
Trans And Gender-Diverse Pelvic Health
A pelvic health physiotherapist can help with preparation for and rehabilitation after transition-related surgeries and other pelvic health conditions that arise from gender-reassignment surgeries.
What are some of the conditions a pelvic health physiotherapist can help with?
1. Surgical Preparation
2. Pelvic Pain - Endometriosis / PCOS (Polycystic Ovary Syndrome)
3. Intimacy Pain - or difficulty with penetration
4. Pregnancy - and Postnatal care for Trans-parents
5. Bladder and Bowel Health
6. Side effects of binding - back pain, chest pain, poor posture, shoulder pain, numbness, and changes to the body’s natural movement patterns.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
FAQs
What does the typical treatment entail?
After a detailed questionnaire and physical examination of your pelvic area (External/Internal), your therapist will discuss the findings with you and plan a treatment program to best suit your needs. Some of the components of the treatment include dietary modifications, changes in voiding pattern, tips to tackle the urgency to empty your bladder. A home exercise program will be set up for you to work on. Your therapist may also suggest the use of different techniques to help you with your exercise program. These techniques may include:
- Manual (hands-on) techniques performed by therapist on the surface of the muscles in the pelvis, to help you locate and work your weak pelvic muscles correctly.
- Electrical Stimulation: Through a metallic probe that is placed about a finger length in your vagina a mild electric current is applied to help you localize and strengthen the pelvic muscles.
- Biofeedback: The same probe can also be used to read the activity of your pelvic floor muscles for display on the screen as you do your exercises. This will allow you to see how well you are performing your exercises. No electric current is felt during biofeedback.
If you have any questions about our Pelvic Floor Physiotherapy program, contact us via confidential email at pelvichealth@trianglephysiotherapy.com.
What is Pelvic Floor Physiotherapy? Is it the same kind of treatment I would receive if I had lower back pain?
Pelvic Floor Physiotherapists are specifically trained in diagnosing and treating conditions associated with the pelvic floor muscles. This usually refers to muscles involved in reproductive and digestive processes in the body. While these muscles are in close proximity to muscles commonly involved in lower back problems, and sometimes even overlap, physiotherapy treatment for the lower back involves significantly different techniques.
What are the most common misconceptions about Pelvic Floor Therapy?
There is a common misconception that only those dealing with incontinence issues and mothers who have recently delivered babies will benefit from Pelvic Floor Physiotherapy. While these two populations certainly are commonly seen by Pelvic Floor Physiotherapists, all of the conditions mentioned above will benefit from treatment.
Another common misconception is that it is only women who can benefit from Pelvic Floor Physiotherapy. This is purely a myth. As you can see from the list above, many conditions are applicable to both men and women.
What does a typical treatment session look like, and how often do I need treatment?
Your Physiotherapist will conduct a thorough subjective assessment of your condition. This will include your history of pain, known triggers for the pain, other relevant medical information, and many other things. Once the subjective portion is completed, your Physiotherapist will perform an internal exam of your applicable pelvic region to assess muscle tone and other objective findings. Once this is completed, your Physiotherapist will clearly communicate all of their findings to you and describe their proposed treatment plan.
There is no one recipe for the number of treatment sessions or the length of time required for full recovery. Some conditions may improve significantly in just a few sessions, while others that are more chronic may take longer to notice a difference. Whatever your prognosis, your Physiotherapist will clearly communicate expected timelines with you.
Will I have to undress?
In order to properly assess objective physical symptoms, your Physiotherapist will need to perform an internal exam of the appropriate pelvic region, which will require removal of clothing below the waist. However, all of our Physiotherapists are extremely professional and are in good standing with the College of Physiotherapists of Ontario, and will ensure that you are draped professionally and appropriately in a gown. Additionally, you will only undergo internal examination if and when necessary.
What is a pessary?
A pessary is a flexible device most often made of silicone, that is inserted vaginally to provide support to pelvic organs (Urethra, Bladder, Uterus, Rectum) that have descended into the vaginal space (prolapsed). It is a non-invasive solution to help women with a prolapse or urinary incontinence. The support from the pessary acts very much like a bra for the pelvic floor.
What are the benefits of a pessary?
- Non-invasive solution
- Conservative therapy
- Improves quality of life in non-surgical situations
- Comfortable, you will not feel the pessary when it fits properly
- Easily removed and reinserted, can be done independently or by health care practitioner like ObGyn or qualified pelvic physiotherapist.
Will my Pelvic Floor treatment be covered under my Extended Health Plan (EHP)?
Yes, Pelvic Floor Physiotherapy treatment will be covered under your EHP as this treatment is administered by a Registered Physiotherapist specialized in Pelvic Floor rehabilitation.



