Physiotherapy can be highly beneficial for individuals suffering from knee osteoarthritis (OA) by addressing pain, improving function, and enhancing the overall quality of life.
What is Knee Osteoarthritis (OA)?
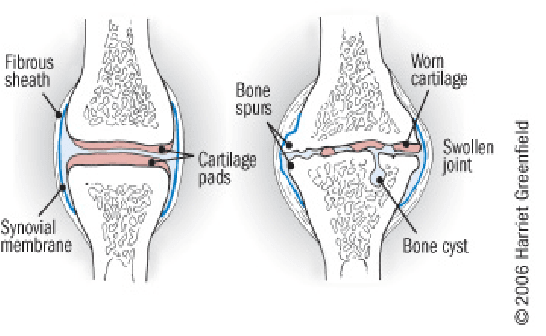
Knee OA is a degenerative joint disease that is typically a result of wear and tear and causes progressive loss of the articular cartilage of the joint.
What are the causes of Knee OA?
Knee osteoarthritis (OA) is a complex condition influenced by a variety of factors. Here are the primary causes and contributing factors:
1. Aging
- Natural Wear and Tear: As people age, the cartilage that cushions the knee joint gradually wears away, leading to OA.
- Decreased Ability to Heal: Older cartilage has a reduced ability to repair itself, making it more susceptible to damage.
2. Genetics
- Family History: Genetic predisposition can play a significant role. If OA runs in your family, you might be more likely to develop it.
- Genetic Mutations: Certain genetic mutations can affect cartilage production and maintenance.
3. Joint Injuries
- Previous Injuries: Injuries such as fractures, ligament tears, or meniscus damage can increase the risk of OA.
- Repetitive Stress Injuries: Repeated stress or overuse of the knee joint, often due to occupational or recreational activities, can lead to OA.
4. Obesity
- Increased Joint Load: Excess body weight puts additional stress on the knee joints, accelerating cartilage breakdown.
- Inflammation: Fat tissue produces inflammatory chemicals that can contribute to joint damage.
5. Mechanical Factors
- Joint Alignment: Abnormal joint alignment, such as bowlegs or knock-knees, can increase stress on certain parts of the knee.
- Muscle Weakness: Weak muscles around the knee, particularly the quadriceps, can lead to increased joint stress.
6. Gender
- Higher Risk in Women: Women, especially those over 50, are more likely to develop knee OA compared to men. Hormonal differences might contribute to this increased risk.
7. Metabolic and Systemic Factors
- Metabolic Syndrome: Conditions like diabetes and metabolic syndrome are associated with an increased risk of OA due to systemic inflammation and metabolic disturbances.
- Inflammatory Diseases: Conditions such as rheumatoid arthritis can predispose individuals to secondary OA.
8. Lifestyle Factors
- Physical Activity: Both excessive and insufficient physical activity can affect joint health. High-impact sports can lead to joint injuries, while sedentary lifestyles can weaken muscles and joints.
- Diet: Poor nutrition can affect joint health. For example, deficiencies in vitamins D and C can impair cartilage maintenance and repair.
9. Joint Biomechanics
- Meniscus Tears: Damage to the meniscus can disrupt joint mechanics and contribute to OA.
- Ligament Damage: Injuries to ligaments, such as the ACL, can destabilize the knee and lead to abnormal wear patterns.
10. Inflammation
- Low-Grade Inflammation: Chronic low-grade inflammation can contribute to the breakdown of cartilage and other joint tissues.
Understanding these causes and contributing factors can help in the prevention and management of knee osteoarthritis, emphasizing the importance of maintaining a healthy lifestyle, avoiding joint injuries, and seeking early intervention for symptoms.
What are the most common symptoms of Knee OA?
Knee osteoarthritis (OA) typically presents with a range of symptoms that can vary in intensity from mild to severe. The most common symptoms include:
1. Pain
- Activity-Related Pain: Pain that worsens with activity or weight-bearing and improves with rest.
- Persistent Pain: Chronic pain that may be present even at rest or during the night in more advanced stages.
2. Stiffness
- Morning Stiffness: Stiffness in the knee that is usually worse in the morning or after periods of inactivity and typically lasts less than 30 minutes.
- Post-Activity Stiffness: Stiffness that occurs after prolonged sitting or resting.
3. Swelling
- Joint Swelling: Swelling around the knee joint due to inflammation or increased production of joint fluid.
- Effusion: Accumulation of excess fluid within the knee joint, leading to noticeable swelling.
4. Reduced Range of Motion
- Limited Flexibility: Difficulty bending or straightening the knee fully.
- Loss of Motion: Progressive decrease in the knee’s range of motion over time.
5. Grinding Sensation (Crepitus)
- Audible Cracking or Popping: A sensation of grinding, cracking, or popping sounds when moving the knee, often due to roughened cartilage surfaces.
6. Weakness or Instability
- Feeling of Giving Way: A sensation that the knee might buckle or give out, often due to muscle weakness or joint instability.
- Muscle Weakness: Weakness in the muscles surrounding the knee, particularly the quadriceps.
7. Deformity
- Joint Deformities: Changes in the shape of the knee joint, such as bowlegged (varus) or knock-kneed (valgus) appearance, due to uneven wear and joint damage.
8. Tenderness
- Joint Tenderness: Tenderness or pain when pressing on or around the knee joint.
9. Functional Impairment
- Difficulty with Activities: Challenges with everyday activities such as walking, climbing stairs, sitting, or standing due to pain and stiffness.
- Reduced Mobility: Decreased ability to perform normal daily activities and exercise.
10. Fatigue
- General Fatigue: Feeling of tiredness and reduced energy levels, often due to chronic pain and sleep disturbances.
These symptoms can significantly impact an individual’s quality of life and ability to perform daily activities. Early recognition and management of knee OA symptoms can help slow disease progression and improve function and comfort.
What are the treatment options for Knee OA?
The number 1 treatment option is conservative management (ie. Patient education, therapeutic exercise, activity modification, weight loss, bracing), surgery should be considered after a conservative approach (talk to your orthopaedic specialist for more information).
Physiotherapy can help by providing you with education about osteoarthritis, tailor an exercise program that is suitable for you, help you consider the best options for activity modifications, provide you with education on bracing, address psychosocial factors such as fear-avoidance, promote patient autonomy and get you back to doing the things you love to do!
Manual therapy- joint mobilization to help with stiffness. Muscle energy technique to help stretch surrounding muscles.
Modalities – heat/ice for pain relief, TENs/IFC for pain relief and inflammation control. Ultrasound for pain relief.
Exercises – help with improving mobility, ROM, strength, balance, aerobic capacity, promoting physical function, reducing knee pain and inflammation.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy can be a highly effective treatment for managing knee osteoarthritis by improving mobility, reducing pain, and enhancing overall function. Whether you are looking for physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are experienced physiotherapists ready to help you manage osteoarthritis and improve your quality of life.