Undergoing any type of surgery can be a daunting experience, especially when you are dealing with pain or discomfort in the lead-up to the procedure. For many patients, managing pain before surgery can be as crucial as the surgery itself, both in terms of improving the surgical outcome and enhancing recovery. Physiotherapy is an essential part of this pre-surgical care, providing strategies to manage pain, improve mobility, and prepare the body for the challenges of surgery and rehabilitation. The highly trained physiotherapists at Triangle Physiotherapy can advise you on strategies on managing pain before surgery and how it can help you feel stronger, more comfortable, and better equipped for recovery.
What is Pre-Surgical Physiotherapy?
Pre-surgical physiotherapy, often referred to as “prehabilitation,” is the practice of preparing the body before surgery through a series of targeted exercises, education, and therapies. The goal is to improve physical fitness, increase mobility, and reduce pain prior to undergoing surgery. By strengthening muscles, improving joint mobility, and reducing stress on affected areas, prehabilitation can make the body more resilient during the recovery process and even reduce the risk of complications after surgery.

The Importance of Managing Pain Before Surgery
Chronic pain, whether from conditions like arthritis, injuries, or musculoskeletal disorders, can be overwhelming and can negatively affect the body’s ability to heal post-surgery. Pre-surgical pain management is not just about addressing discomfort; it’s about setting the stage for a smoother recovery. Here’s why it’s essential to manage pain before surgery:
- Reducing the Impact of Surgery on the Body
Chronic pain can weaken muscles and joints, affecting overall mobility. If these issues are not addressed before surgery, they can impede recovery, increase stress on the surgical site, and lengthen the rehabilitation process. By managing pain pre-operatively, you can make the body more capable of handling the stresses of surgery. - Improved Post-Surgical Outcomes
Research has shown that patients who engage in pre-surgical physiotherapy tend to have better outcomes following surgery. They often experience reduced pain post-operation, faster healing, and a quicker return to normal activities. - Preventing Muscle Atrophy and Stiffness
When dealing with long-term pain, it’s common to limit movement in order to avoid discomfort. This inactivity can lead to muscle atrophy (weakening) and joint stiffness. Physiotherapy helps maintain and even improve strength and flexibility before surgery, ensuring the body is in the best possible condition for a smooth recovery.
How Physiotherapy Can Help Manage Pain Before Surgery
Physiotherapists are experts in movement and pain management, and they can develop tailored treatment plans that address the specific needs of each individual. Here’s how physiotherapy can help manage pain before surgery:
- Pain Relief Techniques
Physiotherapists use a variety of manual therapy techniques to reduce pain and improve joint function. These may include:- Massage therapy to relax muscles and reduce tension.
- Joint mobilizations to increase range of motion and alleviate stiffness.
- Myofascial release to address tightness and discomfort in the soft tissues.
- These techniques can help reduce the intensity of pain, making it easier to engage in exercises and movements that promote healing.
- Strengthening Exercises
Weak muscles can contribute to pain and difficulty moving. Physiotherapists can develop a customized exercise program to strengthen muscles around the affected joints, improving stability and reducing the strain on pain-prone areas. Strengthening key muscle groups ensures that the body is well-prepared for the demands of surgery and recovery. - Mobility and Flexibility Training
Stiffness in the joints and muscles can exacerbate pain and hinder movement. Physiotherapists incorporate stretching and flexibility exercises into pre-surgical programs to improve range of motion. Whether it’s the hips, knees, or shoulders, increasing flexibility can reduce discomfort and prevent further limitations, allowing for better post-surgical rehabilitation. - Postural Correction
Poor posture can put additional strain on joints and muscles, exacerbating pre-existing pain. Physiotherapists assess your posture and provide education on how to align your body correctly during daily activities. Proper posture can prevent unnecessary pressure on joints and muscles, reducing pain and discomfort before surgery. - Education and Pain Management Strategies
Physiotherapists teach patients how to manage pain more effectively through techniques like breathing exercises, mindfulness, and relaxation strategies. Additionally, they may provide advice on managing pain at home, such as the use of heat or cold therapy and ergonomic adjustments in daily activities.
When Should You Seek Pre-Surgical Physiotherapy?
If you’re preparing for surgery and are experiencing pain, stiffness, or limited mobility, it’s a good idea to seek physiotherapy before your procedure. The sooner you begin prehabilitation, the better the results. Ideally, pre-surgical physiotherapy should begin a few weeks to months before the surgery date. However, even if you’re closer to your surgery, starting physiotherapy as soon as possible can still provide significant benefits.
Where can I find a Pre-Surgical Physiotherapy clinic in Oakville?
Triangle Physiotherapy has 8 locations in the GTA, with a physiotherapy clinic in Oakville, located at 2501 Prince Michael Drive, Oakville ON L6H7V6.
Book your prehabilitation appointment today to ensure you get the best outcomes from your surgery.
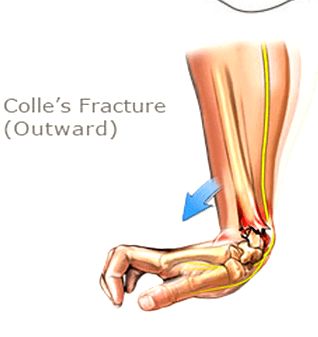
A Colles’ fracture, commonly referred to as a wrist fracture, typically occurs when a person falls onto an outstretched hand. This type of fracture primarily affects the distal radius, the bone located on the thumb side of the wrist. Colles’ fractures are prevalent among older adults, particularly those with osteoporosis, but they can occur at any age. Understanding the nature of this injury, along with effective recovery strategies and preventive measures, is crucial for regaining full functionality of the wrist and minimizing the risk of future injuries.
If you or someone you know has a Colle’s fracture, our physiotherapists at Triangle Physiotherapy can help.
Understanding Recovery
Recovery from a Colles’ fracture generally involves a combination of immobilization, rehabilitation, and lifestyle adjustments. After the fracture is diagnosed—often through X-rays—a healthcare provider may recommend a cast or splint to immobilize the wrist and allow for proper healing. The duration of immobilization can vary, typically lasting between six to eight weeks, depending on the severity of the fracture and the individual’s healing process. Once the cast is removed, the focus shifts to rehabilitation. Recovery times can vary widely, with many patients regaining full function in a few months, while others may take longer. Patience and adherence to a structured recovery plan are essential for optimal healing.
Neuromuscular Exercises post Colle’s Fracture
Neuromuscular exercises are designed to enhance the coordination and communication between the brain and muscles, which is especially important after a wrist injury. These exercises often focus on improving proprioception—the body’s ability to sense its position in space.
1. Wrist and Hand Movements: Start with simple wrist flexion and extension exercises, moving the wrist slowly through its range of motion.
2. Finger Coordination: Practice tapping each finger to the thumb, which helps improve dexterity and coordination.
Incorporating neuromuscular exercises into your recovery routine can significantly aid in regaining strength and functionality.
Mobility Incorporation post Colle’s Fracture
After the initial healing phase, it is crucial to incorporate mobility exercises to restore the full range of motion in the wrist. Gradual stretching and movement help reduce stiffness and enhance circulation.
1. Wrist Circles: Perform wrist circles in both directions to encourage mobility.
2. Tendon Gliding Exercises: These involve moving the fingers and wrist in various positions to promote flexibility and prevent stiffness.
Consistency in these mobility exercises can help ensure a smoother transition back to everyday activities.
Progressive Resistance Exercises
Once mobility is regained, progressive resistance exercises can be introduced to rebuild strength in the wrist and forearm. These exercises should start gently and gradually increase in intensity.
1. Wrist Flexion and Extension with Weights: Using light weights or resistance bands, perform controlled flexion and extension movements.
2. Grip Strengthening: Utilize grip trainers or stress balls to enhance grip strength, which is essential for overall hand function. By progressively increasing resistance, you can strengthen the wrist and surrounding muscles, reducing the likelihood of future injuries.
Prevention
Preventing future Colles’ fractures involves both lifestyle modifications and awareness. Here are some strategies to consider:
1. Fall Prevention: Improve home safety by removing tripping hazards, installing handrails, and ensuring adequate lighting.
2. Bone Health: Engage in weight-bearing exercises and maintain a diet rich in calcium and vitamin D to support bone density.
3. Regular Check-ups: Especially for older adults, regular bone density tests and discussions with healthcare providers about osteoporosis can be critical.
By focusing on prevention, you can significantly lower the risk of future wrist fractures.
FAQs
1. What are the symptoms of a Colles’ fracture?
Symptoms typically include pain and swelling in the wrist, a visible deformity (such as a “dinner fork” appearance), and difficulty moving the wrist or fingers.
2. How long does it take to recover from a Colles’ fracture?
Recovery can vary, but most people see significant improvement within 6 to 12 weeks. Full recovery may take longer, especially for older adults.
3. Can I prevent a Colles’ fracture?
Yes, by improving home safety, maintaining bone health through diet and exercise, and being mindful of your balance and stability, you can reduce your risk of a Colles’ fracture.
4. Are there any long-term effects after recovery?
Some individuals may experience stiffness, reduced range of motion, or chronic pain, particularly if the fracture was severe.
Engaging in rehabilitation exercises can help mitigate these issues. — Understanding and effectively managing a Colles’ fracture is key to ensuring a smooth recovery and maintaining wrist health. By following a comprehensive rehabilitation plan and taking preventive measures, individuals can regain their strength and enjoy a more active lifestyle.
Knee pain can significantly impact your daily activities and overall quality of life. Whether it’s due to an injury, arthritis, or overuse, finding effective relief is essential. Physiotherapy is a valuable tool in managing knee pain, providing strategies to alleviate discomfort and improve function. Whether your knee pain is from a fall, a sports injury, arthritis or everyday aches and pains, our physiotherapists at Triangle Physiotherapy are here to help you navigate your recovery.
Understanding Knee Pain
Knee pain can arise from various conditions, including ligament injuries, tendonitis, bursitis, post-surgery or osteoarthritis. The pain may manifest as sharp, dull, or throbbing sensations, making it challenging to perform everyday tasks. Understanding the underlying cause is crucial for effective treatment. Physiotherapy takes a comprehensive approach to address not only the symptoms but also the root cause of the pain.
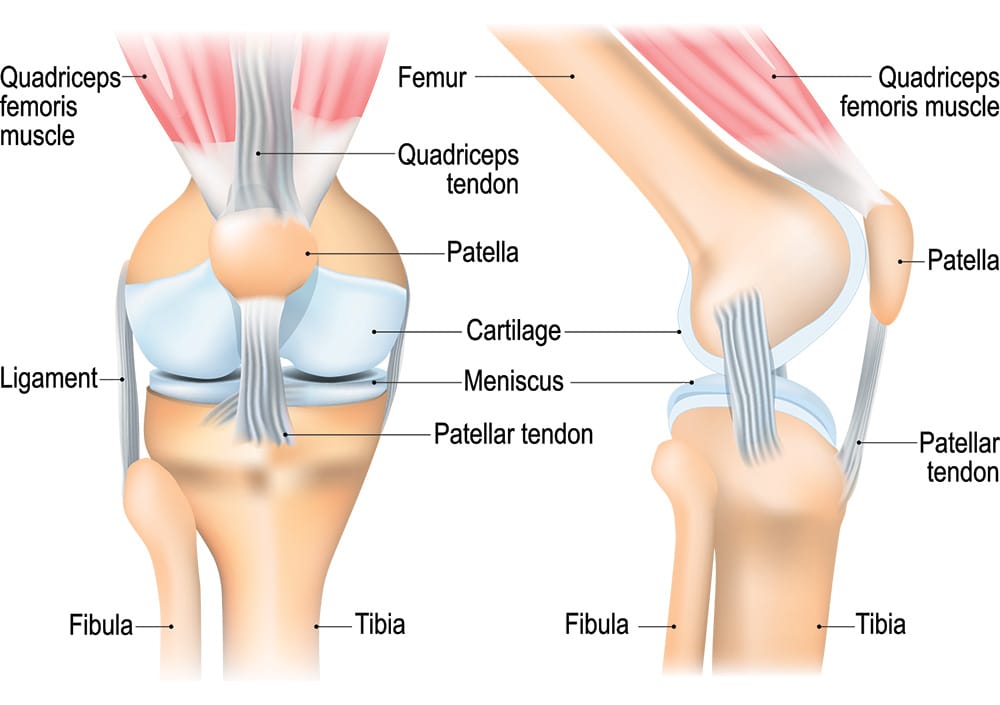
The Role of Physiotherapy
Physiotherapy offers a structured treatment plan tailored to your specific needs. A physiotherapist will conduct a thorough assessment, reviewing your medical history and evaluating your knee’s function. Based on this assessment, they will develop an individualized treatment plan focused on relieving pain, restoring mobility, and strengthening the muscles around the knee.
Pain Management Techniques for Knee Pain
Physiotherapists employ various techniques to manage knee pain effectively. These can include:
- Manual Therapy: Hands-on techniques to mobilize the knee joint and surrounding tissues, reducing stiffness and improving range of motion.
- IMS: Intra muscular Stimulation is an effective tool to trace and treat the root cause, reducing recurrence.
- Modalities: Methods such as ultrasound, heat, or cold therapy can help alleviate pain and inflammation. Read about PEACE and LOVE protocol instead of PRICE.
- Education: Learning about your condition, including proper body mechanics and strategies to avoid aggravating your knee, is vital for long-term management.
Strengthening Exercises
Strengthening the muscles surrounding the knee is crucial for stability and pain relief. Physiotherapists will guide you through targeted exercises that focus on the quadriceps, hamstrings, and calves. These exercises help improve strength and support the knee joint, reducing strain and preventing further injuries.
Mobility and Flexibility
Maintaining mobility and flexibility in the knee is essential for functional movement. Physiotherapy includes stretching exercises and gentle range-of-motion activities to help restore flexibility and reduce stiffness. This focus on mobility not only alleviates pain but also enhances your overall physical activity levels.
Knee Pain Prevention Strategies
Preventing future knee pain is a key aspect of physiotherapy. Your physiotherapist will educate you on proper techniques for daily activities, including walking, climbing stairs, and exercising. They will also address any risk factors, such as muscle imbalances or poor posture, to help you avoid re-injury.
FAQs
Can a physiotherapist help with my knee pain?
Yes, physiotherapists specialize in treating knee pain through tailored rehabilitation programs that target the underlying causes and symptoms.
What should I expect during my first visit to Triangle Physiotherapy?
During your first visit, you’ll undergo a comprehensive assessment, where your physiotherapist will evaluate your knee’s condition, discuss your medical history, and outline your treatment goals. A personalized plan will be created based on this information.
How many sessions will I need?
The number of sessions varies depending on the severity of your knee pain and your progress. Some patients may notice improvement in a few sessions, while others may require ongoing treatment. Your physiotherapist will provide an estimate during your assessment.
Do I need a referral to see a physiotherapist?
No, you do not need a referral to access physiotherapy services. You can book an appointment directly, unless required by your insurance for billing purposes.
How soon can I expect pain relief?
Many patients report relief within a few sessions, but the timeline may vary based on individual circumstances and the underlying cause of the knee pain.
How can I ensure effective management of my knee pain?
Engaging in physiotherapy, adhering to your rehabilitation plan, and performing prescribed exercises regularly are vital for managing knee pain effectively. Open communication with your physiotherapist will also help track your progress.
Conclusion
Physiotherapy is a powerful resource for managing knee pain. By understanding the nature of your condition and engaging in a tailored treatment plan, you can alleviate pain, restore function, and improve your quality of life. If you’re struggling with knee pain, consider the benefits that physiotherapy can provide in your recovery journey. To get help for your knee pain, you can call any of the locations of Triangle Physiotherapy or simply Book An Appointment online.
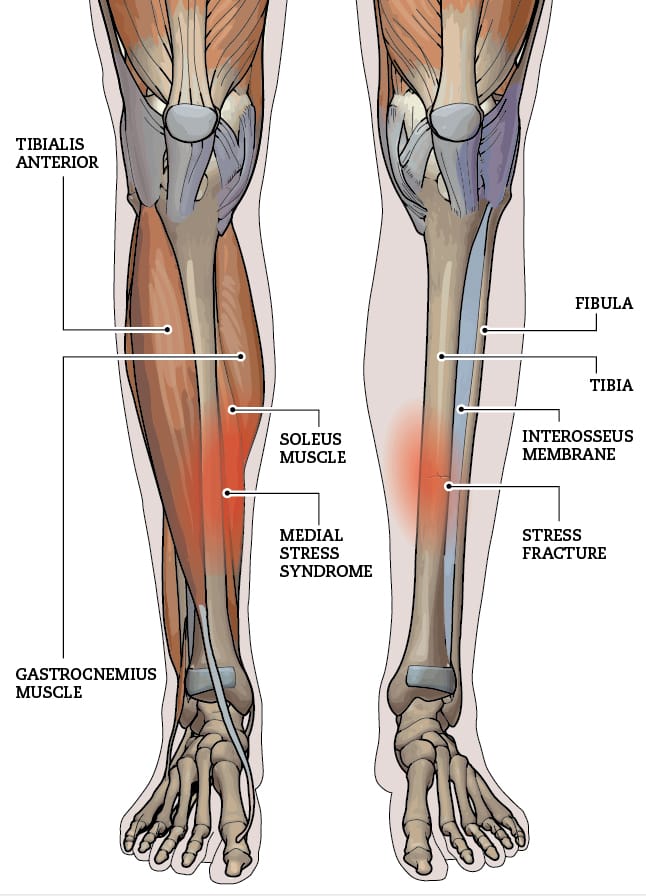
Tibial stress fractures are a common injury among runners, often arising from overuse and repetitive impact on the lower legs. These small discontinuous fractures in the tibia can lead to significant pain and time spent off the tracks, making understanding, recovery, and prevention crucial for athletes. Let’s explore the nature of tibial stress fractures, how to recover effectively, and strategies to prevent future injuries.
Our physiotherapists at Triangle Physiotherapy have the expertise and experience to help with injuries such as these.

FAQs on Tibial Stress Fractures
Q: What are the symptoms of a tibial stress fracture?
A: Common symptoms include localized pain along the shin, swelling, and tenderness that worsens with activity.
Q: How long does it take to recover from a tibial stress fracture?
A: Recovery time can vary, typically ranging from 6 to 12 weeks, depending on the severity of the fracture and adherence to a proper recovery plan.
Q: Can I still run with a tibial stress fracture?
A: It’s essential to avoid running until cleared by a healthcare professional, as continuing to run can worsen the injury.
Q: What type of shoes should I wear to prevent tibial stress fractures?
A: Look for shoes that offer good cushioning and support, tailored to your foot type and running style.
Q: Are there any specific exercises I should avoid during recovery?
A: High-impact exercises should be avoided initially; focus on low-impact activities until fully recovered. By understanding tibial stress fractures and employing the right recovery and prevention strategies, runners can bounce back stronger and continue enjoying their sport safely.
Understanding Recovery of Tibial Stress Fractures
Recovering from a tibial stress fracture involves a multifaceted approach that emphasizes rest and gradual rehabilitation. Initially, it’s essential to reduce weight-bearing activities to allow the bone to heal properly. Depending on the severity of the fracture, this may require crutches or a walking boot. Once the initial pain subsides, a structured recovery plan should include a gradual return to activity, typically guided by a Physiotherapist. Monitoring pain levels during this phase is critical; any increase in pain may indicate that you are pushing too hard, too soon.
Neuromuscular Exercises for Tibial Stress Fractures
Neuromuscular exercises play a vital role in recovery by enhancing coordination, balance, and muscle strength. These exercises can help to correct any biomechanical issues that may have contributed to the injury. Examples include: Balance training: Improve balance and strengthen stabilizing muscles. Agility drills- Help enhance neuromuscular control and prevent future injuries. Proprioception training- Activities like balance boards can improve body awareness and stability. Incorporating these exercises into your routine can significantly aid in the healing process and prepare your body for a return to running.
Mobility Incorporation
Restoring mobility is another critical aspect of recovery. Restricted movement can lead to stiffness and further complications. Gentle stretching and mobility exercises can help maintain flexibility in the surrounding muscles and joints. Key mobility exercises can include working on key muscles like Calf, Hip flexor mobility to name a few. Regularly integrating these mobility exercises will not only aid in recovery but also improve overall performance in the long run.
Progressive Resistance Exercises
Once you are pain-free and have regained some mobility, incorporating progressive resistance exercises is essential for rebuilding strength. This phase focuses on strengthening the muscles surrounding the tibia to provide better support and prevent future stress fractures. Examples include strengthening the calves and improving ankle stability, build strength in the quadriceps, hamstrings, and glutes. Start with light resistance and gradually increase intensity as your strength improves, always prioritizing proper form to prevent re-injury.
Prevention
Preventing tibial stress fractures is all about maintaining a balanced training regimen. Pay attention to warning signs such as persistent pain or fatigue and adjust your training accordingly. Integrating a proper rehab plan under the supervision of a physiotherapist along with proper relaxation techniques provided by Massage therapist can significantly reduce the risk of developing a tibial stress fracture and maintain your running routine.
Suffered a Tibial Stress Fracture Injury? Book an appointment with us to get on the road to recovery.
Arthritis and joint pain are common conditions that can significantly affect daily life. These issues often lead to discomfort, stiffness, and decreased mobility, making everyday activities challenging. Fortunately, physiotherapy offers effective strategies to manage these symptoms and improve quality of life.
If you would like to learn more about how Triangle Physiotherapy can help you manage your arthritis pain, contact us today!
Understanding Arthritis and Joint Pain
Arthritis encompasses various conditions that cause inflammation in the joints, leading to pain and stiffness. Osteoarthritis and rheumatoid arthritis are two prevalent types. While arthritis can be caused by age, injury, or autoimmune disorders, the impact on an individual’s well-being can be profound. Beyond physical discomfort, arthritis can lead to emotional distress and social withdrawal, emphasizing the need for effective management strategies.
The Role of Physiotherapy for Arthritis

Physiotherapy is a cornerstone in managing arthritis and joint pain. A skilled physiotherapist can assess your condition and create a personalized treatment plan tailored to your specific needs. This plan may include various interventions, such as manual therapy, therapeutic exercises, and education about joint protection techniques.
Tailored Exercise Programs
Exercise is crucial for managing arthritis. A physiotherapist can guide you in developing a safe and effective exercise routine that enhances strength, flexibility, and range of motion. Low-impact activities such as swimming, cycling, and walking are often recommended, as they minimize stress on the joints while promoting movement.
Manual Therapy
Manual therapy techniques, such as joint mobilization and soft tissue massage, can help alleviate pain and improve joint function. These hands-on approaches can reduce stiffness and enhance circulation around the affected joints, providing immediate relief and promoting long-term recovery.
Education and Self-Management Strategies
An essential aspect of physiotherapy is educating patients about their condition. Understanding arthritis and its impact on the body empowers individuals to make informed choices. Physiotherapists teach joint protection strategies, ergonomic principles, and how to modify activities to minimize strain on the joints. This knowledge helps individuals take an active role in managing their pain.
Incorporating Lifestyle Changes
In addition to physiotherapy, adopting a healthy lifestyle can further alleviate arthritis symptoms. Maintaining a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can support joint health. Staying hydrated and managing stress through relaxation techniques can also be beneficial.
Tips for Managing Arthritis and Joint Pain
- Stay Active: Engage in regular, low-impact exercise to keep joints moving and muscles strong.
- Listen to Your Body: Be aware of your pain levels and modify activities as needed.
- Use Supportive Devices: Braces, splints, or orthotics can provide additional support and stability.
- Prioritize Rest: Ensure you get adequate rest to allow your body to recover.
- Consult Professionals: Always seek guidance from healthcare providers or physiotherapists before starting new activities.
Managing arthritis and joint pain can be challenging, but physiotherapy offers effective tools to enhance your quality of life. Through personalized treatment plans, education, and lifestyle adjustments, individuals can regain control over their bodies and reduce the impact of pain. With the right support and commitment to an active lifestyle, it is possible to live a fulfilling life despite arthritis. Embracing physiotherapy can be a transformative step towards achieving better joint health and overall well-being.
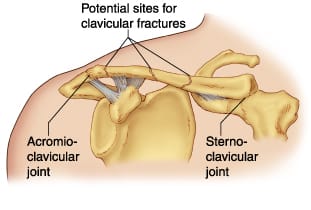
Clavicular fractures, commonly known as broken collarbones, are prevalent injuries, especially among athletes and those engaged in physical activities. This type of fracture typically occurs due to falls, direct trauma to collarbone or shoulder, or collisions. Understanding the clavicular fractures in detail, their recovery process, and preventive measures can help individuals better manage their healing journey and minimize the risk of future injuries.
Schedule an appointment with one of the physiotherapists at one of the 8 locations of Triangle Physiotherapy if you have had a clavicular fracture and are looking to achieve optimal recovery.
What is the recovery timeline for clavicular fractures?
The recovery timeline for a clavicular fracture can vary based on the severity of the break and the individual’s overall health. Generally, non-displaced fractures may heal within 6 to 12 weeks with conservative treatment, including rest, immobilization, and pain management. In more severe cases, surgical intervention may be necessary, leading to a slightly extended recovery period. During this time, it’s essential to follow medical advice and engage in a structured rehabilitation program under the supervision of a Physiotherapist to restore strength and function to the shoulder.
What type of exercises are beneficial in the rehabilitation Clavicular Fractures?
Neuromuscular Exercises
Neuromuscular exercises play a crucial role in the rehabilitation process. These exercises focus on improving coordination and communication between the nervous system and muscles, which is vital for shoulder recovery. Some forms of improving the neuro-muscle link could be gentle isometric contractions of the shoulder muscles without joint movement, activating the shoulder blade muscles. As healing progresses, activities that involve controlled movements can help enhance muscle activation and prevent stiffness, promoting a smoother transition to more strenuous exercises.
Mobility Incorporation
Incorporating mobility exercises into the rehabilitation program is essential for restoring range of motion in the shoulder. Gentle stretching and mobility drills should begin as soon as cleared by a healthcare professional. Physiotherapist would be the perfect healthcare practitioner that can guide you in terms of muscle activation and rehabilitation. Common exercises include pendulum swings and passive arm movements. These activities not only help to alleviate stiffness but also prepare the shoulder for more demanding functional tasks. Regularly practicing mobility exercises ensures that the joint remains flexible and reduces the risk of future injuries.
Progressive Resistance Exercises
Once the shoulder has regained sufficient mobility and strength, progressive resistance exercises can be introduced. These exercises aim to gradually increase the load on the muscles surrounding the shoulder joint, facilitating strength development and functional recovery. Starting with lightweight resistance bands or dumbbells, individuals can perform exercises focusing on rotator cuff, shoulder stabilizers as well as the scapular muscles. The key is to focus on form and gradually increase resistance as strength improves, avoiding any pain or discomfort.
How can clavicular fractures be prevented?
Preventing clavicular fractures involves a combination of strength training, proper technique, and awareness of one’s surroundings. In order to prevent clavicular fractures, one needs a multidisciplinary approach under the supervision of a Physiotherapist, Chiropractor and a Massage Therapist. Engaging in shoulder-strengthening exercises can improve stability and reduce the likelihood of injuries. Athletes should prioritize learning proper falling techniques to minimize impact during falls or collisions. Additionally, wearing protective gear in high-risk sports can provide an extra layer of safety. Overall, being proactive about shoulder health can significantly decrease the chances of experiencing a clavicular fracture.
Other FAQ’s
FAQs
Q: How can I tell if I have a clavicular fracture?
A: Symptoms may include sharp pain at the site of the injury, swelling, bruising, and difficulty moving the shoulder. A visible deformity or “bump” over the collarbone may also indicate a fracture.
Q: Do all clavicular fractures require surgery?
A: No, not all fractures require surgery. Non-displaced fractures are often treated conservatively, while displaced fractures or those involving significant displacement may necessitate surgical intervention.
Q: How long will it take to return to normal activities?
A: Recovery times vary but typically range from 6 to 12 weeks for non-displaced fractures. Full recovery and return to sports may take longer, depending on the nature of the fracture and rehabilitation progress.
Q: Are there any long-term effects of a clavicular fracture?
A: Most individuals recover fully without long-term complications. However, some may experience residual pain or reduced strength in the shoulder. Engaging in a comprehensive rehabilitation program can help mitigate these risks.
Q: What should I do if I suspect a clavicular fracture?
A: Seek medical attention immediately. A healthcare professional can provide an accurate diagnosis and develop a treatment plan tailored to your needs. By understanding clavicular fractures and their recovery process, individuals can better navigate their healing journey and take proactive steps to prevent future injuries. Always consult with healthcare professionals to ensure the best outcomes during recovery and rehabilitation.
If you would like to start you post-fracture rehab at Triangle Physiotherapy, contact us today to schedule a physiotherapy appointment.
Living an active lifestyle is crucial for our overall health and well-being. It’s not just about hitting the gym; it’s about integrating movement into your daily life. Whether you’re looking to enhance your mobility or recover from an injury, physiotherapy in Oakville can play a key role in helping you stay active. Here are seven tips that can help you embrace a more active lifestyle, focusing on various exercise types, prevention strategies, and the importance of physiotherapy.

1. Embrace Neuromuscular Exercises
Neuromuscular exercises are all about improving your body’s ability to perform coordinated movements. Think of activities like yoga, Pilates, or tai chi. These exercises enhance balance, agility, and coordination, which are essential for daily activities and overall mobility.
Start by incorporating short sessions into your routine. Even 15 minutes of yoga in the morning can make a difference. If you’re in Oakville, you can consult a physiotherapist to ensure your movements are precise and safe, helping you avoid injury. As you become more comfortable, explore different styles or join a class to keep things exciting.
2. Incorporate Progressive Resistance Exercises
Progressive resistance exercises are crucial for building strength and endurance. These exercises involve gradually increasing the amount of weight or resistance you use, helping your muscles adapt and grow stronger over time.
You don’t need a gym membership to do this. Bodyweight exercises like push-ups, squats, and lunges can be done anywhere. For those in Oakville looking to enhance their routine, physiotherapy can offer personalized advice on proper technique, especially if you’re recovering from an injury or have muscle imbalances. Aim for two to three sessions per week, focusing on major muscle groups for balanced strength development.
3. Prioritize Mobility Exercises
Mobility exercises enhance your range of motion and flexibility, reducing the risk of injury. Think dynamic stretches or mobility drills that prepare your body for movement.
Integrate these exercises into your warm-up routine before any physical activity. Simple movements like arm circles, hip openers, and ankle rolls can improve your mobility significantly. If you’re looking for guidance, physiotherapy in Oakville can assist in identifying areas of stiffness or restricted movement and provide tailored exercises to improve your flexibility.
Good mobility isn’t just for athletes; it’s essential for everyone. It helps with daily tasks like bending down to tie your shoes or reaching for items on high shelves.
4. Focus on Prevention
Incorporating preventative measures into your active lifestyle is key. This includes listening to your body and recognizing signs of overexertion or fatigue. Stretching before and after exercise can help reduce muscle tension and soreness.
If you are in Oakville, regular visits to a physiotherapist can help you prevent injuries before they happen. They can evaluate your movement patterns and suggest exercises that align with your fitness goals while minimizing the risk of injury. Prevention is always better than cure, so pay attention to your body’s signals and adapt your routine accordingly.
5. Understand the Importance of Physiotherapy
Physiotherapy plays a vital role in maintaining an active lifestyle, especially if you’ve had past injuries or chronic pain. A physiotherapist can assess your movement patterns, identify weaknesses, and design a tailored exercise program to help you improve.
If you’re in Oakville, a local physiotherapy clinic can provide valuable insights even when you feel fine. Consulting a professional early on can help you develop a balanced routine that enhances your strength and mobility, reducing your risk of injury in the long run.
6. Tips for Safely Performing Exercises
Safety should always be a priority when exercising. Here are some tips to ensure you stay injury-free:
- Warm Up and Cool Down: Spend at least five to ten minutes warming up before any workout and cooling down afterward.
- Focus on Form: Proper form is essential to prevent injuries. If you’re unsure, don’t hesitate to ask for guidance or watch instructional videos. Better yet, seek advice from a physiotherapist in Oakville to ensure you’re doing exercises correctly.
- Start Slow: If you’re new to a type of exercise, ease into it. Gradually increase intensity and duration as your body adapts.
- Stay Hydrated: Dehydration can lead to fatigue and injuries, so drink plenty of water before, during, and after exercise.
7. Make Movement a Daily Habit
Lastly, find ways to incorporate more movement into your daily routine. Take the stairs instead of the elevator, walk or bike for short errands, or even set a timer to remind you to stretch or take a quick walk every hour.
If you’re based in Oakville, there are various local parks and trails where you can get moving outdoors. Additionally, a physiotherapy consultation can help you find creative ways to integrate movement into your routine, especially if you’re dealing with mobility limitations.
The key is to make movement enjoyable. Try different activities until you find what you love, and remember that every little bit counts!
Check out this article on the Concept of Wellness.
Hiking is a wonderful way to explore nature and stay active, but it’s not without its risks. Understanding common hiking injuries, their causes, symptoms, and effective prevention strategies can make your outdoor adventures safer and more enjoyable. Here’s a comprehensive guide to help you stay injury-free on the trails.
Understanding Hiking Related Injuries
Hiking can lead to various injuries, often related to the terrain, equipment, or physical condition of the hiker. Common hiking injuries include:
- Sprained Ankles: Caused by uneven ground, rocks, or roots.
- Knee Injuries: Such as patellar tendonitis or meniscus tears from repetitive strain.
- Muscle Strains: Typically in the calves, thighs, or lower back due to overexertion.
- Blisters and Hotspots: Resulting from friction and poorly fitting footwear.
- Sunburn and Heat Exhaustion: Due to prolonged exposure to the sun and inadequate hydration.
- Back Injuries: Resulting from improper lifting of heavy backpacks or poor posture.

Causes and Symptoms
Each type of injury has specific causes and symptoms:
- Sprained Ankles: Twisting the ankle on unstable ground, causing pain, swelling, and difficulty walking.
- Knee Injuries: Overuse, sudden twists, or impacts leading to pain, swelling, and limited mobility.
- Muscle Strains: Overstretching or overloading muscles, resulting in pain, stiffness, and reduced range of motion.
- Blisters and Hotspots: Friction from ill-fitting socks or boots causing painful, fluid-filled sacs on the skin.
- Sunburn and Heat Exhaustion: Excessive sun exposure leading to red, painful skin, dehydration, dizziness, and nausea.
- Back Injuries: Lifting heavy loads improperly, causing pain, stiffness, or spasms in the lower back.
Importance of Physiotherapy for Hiking Injuries
Physiotherapy plays a crucial role in treating hiking injuries by promoting recovery, restoring mobility, and preventing future problems. Benefits include:
- Pain Relief: Through targeted exercises and techniques.
- Restoration of Mobility: Enhancing flexibility and range of motion.
- Improvement in Strength: Strengthening muscles to support injured areas.
- Prevention of Recurrence: Teaching proper movement patterns and injury prevention strategies.
Key Principles of Physiotherapy Exercises for Pain Relief
Physiotherapy exercises focus on alleviating pain and promoting healing:
- Stretching and Range of Motion Exercises: Improve flexibility and joint function.
- Proprioception Training: Enhance balance and stability to prevent re-injury.
- Manual Therapy: Techniques such as massage or joint mobilization to reduce pain and inflammation.
Strengthening Exercises
Building strength is essential for recovery and injury prevention:
- Core Strengthening: Supports the back and improves posture.
- Lower Body Exercises: Target muscles in the legs and hips for stability.
- Resistance Training: Uses bands or weights to strengthen specific muscle groups.
Neuromuscular Exercises for Pain Management and Prevention
These exercises improve coordination and control:
- Balance Exercises: Enhance stability on uneven terrain.
- Functional Movements: Mimic hiking motions to improve efficiency and reduce strain.
Progressive Resistance Training
Gradually increasing resistance builds strength:
- Incremental Loading: Challenges muscles without causing undue stress.
- Specificity: Tailors exercises to mimic hiking movements and demands.
Incorporating Stretching and Flexibility Exercises in Your Routine
Regular stretching maintains muscle elasticity and joint flexibility:
- Pre-hike Stretching: Warms up muscles and prepares them for activity.
- Post-hike Stretching: Helps muscles recover and prevents stiffness.
Tips for Safely Performing Physiotherapy Exercises
Follow these guidelines to avoid further injury:
- Consult a Professional: Get a personalized exercise plan from a physiotherapist.
- Start Gradually: Increase intensity and duration of exercises as tolerated.
- Listen to Your Body: Stop if you feel pain beyond normal discomfort.
- Stay Consistent: Perform exercises regularly for best results.
Hiking injuries can be prevented and managed effectively with the right knowledge and preparation. By understanding the causes, symptoms, and treatment options for common hiking injuries, along with incorporating physiotherapy exercises into your routine, you can enjoy the trails safely and confidently. Remember, safety and preparation are key to a rewarding hiking experience—happy trails!
Conclusion
Don’t let these physical conditions ever ride on you. You can consult any of our locations of Triangle Physiotherapy or simply Book An Appointment online.
“Whether you’re dealing with hiking-related injuries or any other physical discomfort, Triangle Physiotherapy offers expert care at multiple locations across the GTA. Our clinics provide Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Visit us to receive tailored treatment that helps you get back on your feet and enjoy the activities you love.”
Spinal fusion surgery is a medical procedure used to permanently join two or more vertebrae in the spine, eliminating motion between them. The goal of the surgery is to reduce pain, correct deformities, or improve stability in the spine.
When would I need Spinal Fusion Surgery?
Spinal fusion surgery is typically recommended for various spine conditions, including:
- Degenerative disc disease: When the discs between vertebrae break down, causing pain.
- Spondylolisthesis: When one vertebra slips forward over the one below it.
- Spinal stenosis: Narrowing of the spinal canal, leading to nerve compression.
- Scoliosis: Abnormal curvature of the spine.
- Fractures: Vertebrae that are broken or dislocated.
- Tumors: Removal of tumors that affect spinal stability.
- Infections: Infections that have caused damage to the vertebrae.
When do I start physiotherapy after surgery?
The timing of when to start physiotherapy after spinal fusion surgery depends on several factors, including the specifics of the surgery, the patient’s overall health, and the surgeon’s recommendations.
What does post-surgery rehab involve?
Immediate Postoperative Period (0-6 Weeks)
- Initial Phase: Physiotherapy may start in the hospital within a day or two after surgery. The focus is on gentle movements and exercises to improve circulation and prevent complications.
- Activities:
- Breathing exercises to prevent lung complications.
- Gentle leg movements like ankle pumps to improve blood flow.
- Log rolling technique for safe movement in and out of bed.
- Short, frequent walks to promote circulation and reduce stiffness.
Early Rehabilitation Phase (6-12 Weeks)
- When: Typically, more structured physical therapy begins around 4 to 6 weeks after surgery, depending on the surgeon’s assessment.
- Goals: Gradually increase mobility, start gentle strengthening exercises, and improve functional movements.
- Activities:
- Range of motion exercises.
- Gentle strengthening exercises for the core and lower extremities.
- Walking programs to gradually increase distance and duration.
- Education on proper body mechanics and posture.
Late Rehabilitation Phase (3-6 Months)
- When: Around 3 months post-surgery, assuming there are no complications.
- Goals: Restore full function, enhance strength and endurance, and improve posture and body mechanics.
- Activities:
- More advanced strengthening exercises using resistance bands or light weights.
- Low-impact aerobic exercises like swimming or cycling.
- Balance and coordination exercises.
- Functional training for daily activities.
Long-Term Rehabilitation Phase (6-12 Months)
- When: After 6 months, the patient should continue with physiotherapy based on individual progress and goals.
- Goals: Achieve optimal strength, flexibility, and functional ability, and prevent recurrence of symptoms.
- Activities:
- Progressive resistance training.
- Gradual reintroduction of higher-impact activities, if appropriate.
- Sport-specific training for athletes.
- Ongoing education on maintaining spine health.
Key Points to Consider
- Surgeon’s Recommendations: Always follow the specific guidelines and timelines provided by the surgeon, as they know the details of the surgery and individual patient needs.
- Listen to Your Body: Avoid pushing through pain. Pain is a signal that something might be wrong, and it’s important to communicate any discomfort to the physiotherapist or surgeon.
- Individual Variation: Each patient’s recovery is unique. Factors such as age, overall health, and the complexity of the surgery will influence the timing and intensity of physiotherapy.
Starting physiotherapy at the right time is crucial for a successful recovery, and adhering to a structured rehabilitation program can significantly enhance outcomes after spinal fusion surgery.
Click here to book an appointment for post-surgery rehab with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
General Information: The information provided on this blog is for general informational purposes only. While we strive to ensure the accuracy and relevance of our content, we make no guarantees about the completeness, reliability, or accuracy of the information.
Not Professional Advice: The content on this blog does not constitute professional advice. It is not a substitute for professional medical, legal, financial, or other professional advice. Always seek the guidance of a qualified professional with any questions you may have regarding your specific situation.
Recovering from spinal fusion surgery requires careful physiotherapy to restore mobility and strength. Whether you need physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are expert physiotherapists available to guide your recovery journey and help you regain your quality of life.
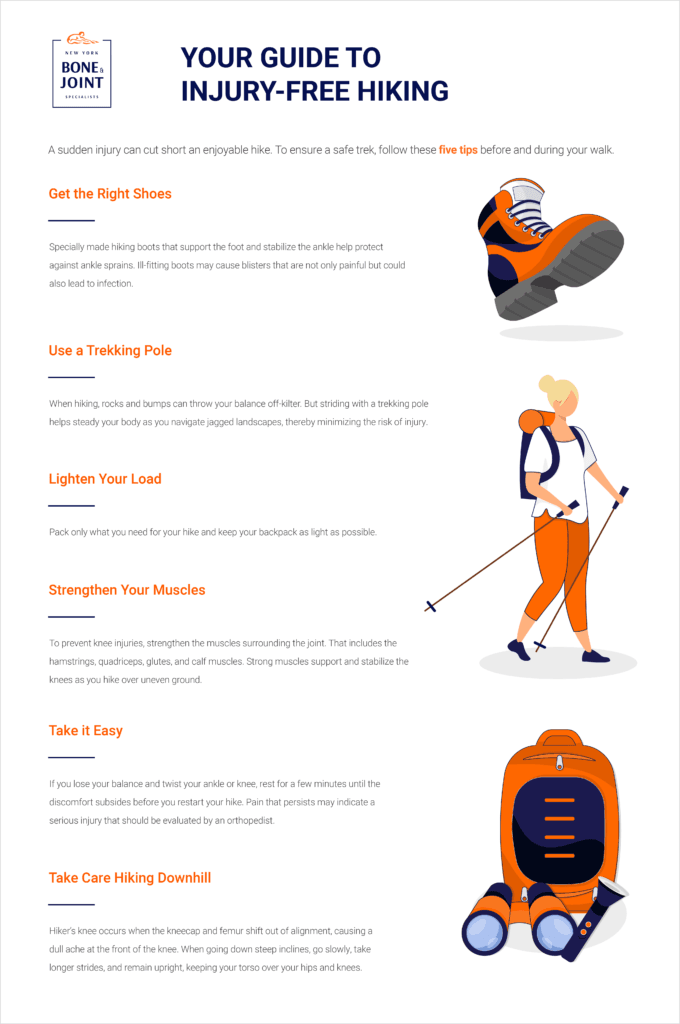
Hiking is a fantastic way to enjoy the great outdoors and stay fit, but it can also pose some risks. Whether you’re new to hiking or a seasoned backpacker, there are numerous factors to take into account before heading out on the trails. You need to evaluate your backpack’s weight, choose appropriate footwear, plan your food and hydration, check the weather, and map out your routes. Additionally, since hiking often takes you off the beaten path, it’s essential to take precautions against three common hiking injuries: knee pain, ankle sprains, and sore feet.
Is it necessary to warm up before hiking?
Yes, it is necessary to warm up before hiking. Warming up helps prepare your muscles and joints for physical activity, reducing the risk of injury. Here are some reasons why warming up is important before hiking:
Benefits of Warming Up Before Hiking
- Increases Blood Flow: A proper warm-up increases blood flow to your muscles, delivering oxygen and nutrients that help them perform better.
- Enhances Flexibility: Warming up loosens your muscles and increases your range of motion, making it easier to navigate uneven terrain.
- Reduces Injury Risk: Warm muscles are less prone to strains, sprains, and other injuries.
- Prepares Your Heart: Gradually increasing your heart rate helps prepare your cardiovascular system for the more strenuous activity of hiking.
- Improves Performance: A good warm-up can improve your overall performance, making your hike more enjoyable and less exhausting.
What are some effective warm up exercises to do before hiking?
Effective Warm-Up Exercises
- Walking or Light Jogging: Start with 5-10 minutes of brisk walking or light jogging to get your blood flowing.
- Dynamic Stretches: Perform dynamic stretches like leg swings, arm circles, and torso twists to loosen up your muscles and joints.
- Ankle Rotations: Rotate your ankles in circles to prepare them for the uneven terrain.
- Hip Circles: Rotate your hips to loosen the hip joints, which are crucial for hiking.
- Calf Raises: Perform calf raises to warm up your calves, which are heavily used during hiking.
Taking a few minutes to warm up before you start your hike can make a significant difference in your overall hiking experience and help prevent injuries.
What are the most common hiking injuries?
Some of the most common hiking injuries are:
- Knee Pain
- Ankle Sprain
- Foot Pain
Knee Pain when Hiking
Knee pain is a common issue among hikers, especially on longer or more challenging trails. Here’s a comprehensive approach to understanding, preventing, and managing knee pain when hiking:
Causes of Knee Pain While Hiking
- Overuse and Strain: Continuous stress on the knee joint from uphill climbs, downhill descents, or long sessions of hiking.
- Improper Biomechanics: Poor hiking technique, such as improper foot placement or stride, can strain the knee joint.
- Previous Injuries: Past knee injuries or conditions like arthritis can flare up during hiking.
- Improper Gear: Worn-out or inappropriate footwear lacking proper cushioning and support.
Ankle Sprain when Hiking
An ankle sprain can be a painful and frustrating injury, especially when hiking in rugged terrain. Here’s how to understand, prevent, and manage ankle sprains while hiking:
Causes of Ankle Sprains While Hiking
- Uneven Terrain: Stepping on uneven surfaces, rocks, or roots can twist or roll the ankle.
- Fatigue: Muscles that support the ankle can become tired, leading to less stability and increased risk of injury.
- Inadequate Footwear: Wearing shoes or boots without proper ankle support or that are worn out.
Foot Pain when Hiking
Foot pain while hiking can be uncomfortable and distracting. Here’s how to understand, prevent, and manage foot pain effectively:
Causes of Foot Pain While Hiking
- Improper Footwear: Shoes or boots that are too tight, loose, worn out, or lacking proper cushioning and support.
- Overuse or Strain: Prolonged walking or hiking, especially on challenging terrain, can strain the muscles and joints of the feet.
- Blisters: Friction from improperly fitting shoes or moisture buildup can lead to painful blisters.
If you get injured while hiking, consult one of our physiotherapists who can help you with treating the injuries as well as advise and educate you on prevention so you can enjoy your outdoor activities without pain and discomfort.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills