Arthritis and joint pain are common conditions that can significantly affect daily life. These issues often lead to discomfort, stiffness, and decreased mobility, making everyday activities challenging. Fortunately, physiotherapy offers effective strategies to manage these symptoms and improve quality of life.
If you would like to learn more about how Triangle Physiotherapy can help you manage your arthritis pain, contact us today!
Understanding Arthritis and Joint Pain
Arthritis encompasses various conditions that cause inflammation in the joints, leading to pain and stiffness. Osteoarthritis and rheumatoid arthritis are two prevalent types. While arthritis can be caused by age, injury, or autoimmune disorders, the impact on an individual’s well-being can be profound. Beyond physical discomfort, arthritis can lead to emotional distress and social withdrawal, emphasizing the need for effective management strategies.
The Role of Physiotherapy for Arthritis

Physiotherapy is a cornerstone in managing arthritis and joint pain. A skilled physiotherapist can assess your condition and create a personalized treatment plan tailored to your specific needs. This plan may include various interventions, such as manual therapy, therapeutic exercises, and education about joint protection techniques.
Tailored Exercise Programs
Exercise is crucial for managing arthritis. A physiotherapist can guide you in developing a safe and effective exercise routine that enhances strength, flexibility, and range of motion. Low-impact activities such as swimming, cycling, and walking are often recommended, as they minimize stress on the joints while promoting movement.
Manual Therapy
Manual therapy techniques, such as joint mobilization and soft tissue massage, can help alleviate pain and improve joint function. These hands-on approaches can reduce stiffness and enhance circulation around the affected joints, providing immediate relief and promoting long-term recovery.
Education and Self-Management Strategies
An essential aspect of physiotherapy is educating patients about their condition. Understanding arthritis and its impact on the body empowers individuals to make informed choices. Physiotherapists teach joint protection strategies, ergonomic principles, and how to modify activities to minimize strain on the joints. This knowledge helps individuals take an active role in managing their pain.
Incorporating Lifestyle Changes
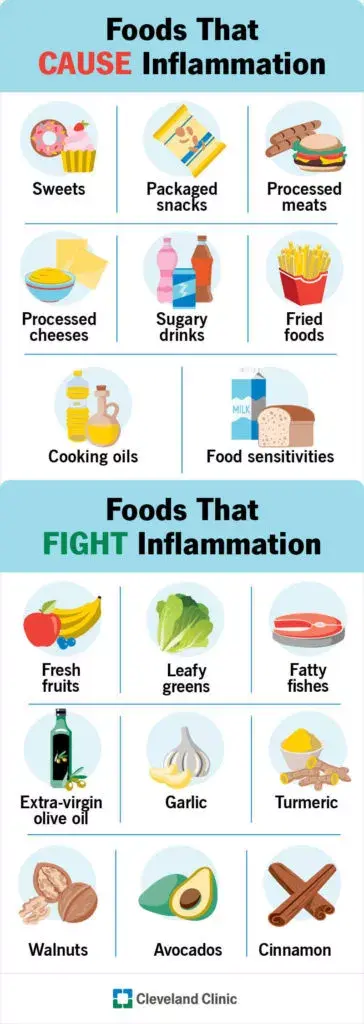
In addition to physiotherapy, adopting a healthy lifestyle can further alleviate arthritis symptoms. Maintaining a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can support joint health. Staying hydrated and managing stress through relaxation techniques can also be beneficial.
Tips for Managing Arthritis and Joint Pain
- Stay Active: Engage in regular, low-impact exercise to keep joints moving and muscles strong.
- Listen to Your Body: Be aware of your pain levels and modify activities as needed.
- Use Supportive Devices: Braces, splints, or orthotics can provide additional support and stability.
- Prioritize Rest: Ensure you get adequate rest to allow your body to recover.
- Consult Professionals: Always seek guidance from healthcare providers or physiotherapists before starting new activities.
Managing arthritis and joint pain can be challenging, but physiotherapy offers effective tools to enhance your quality of life. Through personalized treatment plans, education, and lifestyle adjustments, individuals can regain control over their bodies and reduce the impact of pain. With the right support and commitment to an active lifestyle, it is possible to live a fulfilling life despite arthritis. Embracing physiotherapy can be a transformative step towards achieving better joint health and overall well-being.
As we age, maintaining mobility and independence becomes increasingly important for overall quality of life. For many elderly individuals, staying active and independent can be challenging due to various age-related factors. Physiotherapy emerges as a crucial tool in addressing these challenges, helping seniors preserve their physical function and improve their daily living. This blog explores the importance of physiotherapy for the elderly, highlighting causes of mobility issues, preventive measures, and effective exercises to support strength and mobility.
Our experienced practitioners at Triangle Physiotherapy can help you to stay active and prevent any mobility issues that may arise with age.
Call us today to learn more about how we can help you start moving better.
Causes
Several factors contribute to decreased mobility in elderly individuals. Common causes include:
- Muscle Weakness: Aging often leads to muscle loss, making it harder to perform everyday activities.
- Joint Stiffness: Reduced flexibility and joint pain can limit movement.
- Balance Problems: Deteriorating balance increases the risk of falls, which can lead to serious injuries.
- Chronic Conditions: Diseases such as arthritis, osteoporosis, and cardiovascular issues can impact physical ability.
Understanding these causes helps in designing targeted physiotherapy interventions to address specific challenges and improve overall function.
Prevention

Preventive measures play a vital role in maintaining mobility and independence as we age. Regular physical activity, a balanced diet, and routine medical check-ups can help mitigate some of the issues that arise with aging. Your Physiotherapist will help you incorporate the following into daily routines can be beneficial:
- Regular Exercise: Engaging in physical activities such as walking, swimming, or biking helps maintain muscle strength and joint flexibility.
- Healthy Diet: A diet rich in calcium and vitamin D supports bone health, while protein helps in muscle maintenance.
- Routine Check-ups: Regular visits to healthcare professionals can help manage chronic conditions and prevent complications.
Importance of Physiotherapy
Physiotherapy is essential for elderly individuals to address and manage mobility issues. It offers several benefits:
- Personalized Care: Physiotherapists design customized exercise programs based on individual needs and limitations.
- Pain Management: Through techniques like manual therapy and modalities such as heat or cold therapy, physiotherapy can help alleviate pain.
- Fall Prevention: Physiotherapy can enhance balance and coordination, reducing the risk of falls and related injuries.
- Enhanced Quality of Life: Improved mobility and independence contribute to a better overall quality of life and increased participation in social activities.
Strengthening and Mobility Exercises
Strengthening and mobility exercises are fundamental components of physiotherapy for seniors. These exercises help maintain and improve physical function:
- Strengthening Exercises: Focus on major muscle groups to enhance overall strength. Examples include seated leg lifts, wall push-ups, and resistance band exercises.
- Mobility Exercises: Improve joint flexibility and range of motion. Simple activities such as ankle circles, shoulder rolls, and gentle stretching can be beneficial.
- Additionally, the GLA:D Program for Knee and Hip Arthritis can be very beneficial because it provides education and targeted exercise that can be applied to movement in everyday activities.
Regular practice of these exercises helps prevent muscle atrophy and joint stiffness, promoting better movement and function.
Neuromuscular Exercises
Neuromuscular exercises target coordination, balance, and proprioception (the sense of body position). These exercises are crucial for fall prevention and overall stability:
- Balance Training: Activities such as standing on one leg, heel-to-toe walking, and balance board exercises enhance stability.
- Coordination Drills: Exercises like toe taps, marching in place, and dynamic movements help improve coordination and reaction times.
- Proprioceptive Exercises: Incorporate activities that challenge the senses and improve body awareness, such as using a wobble cushion or performing slow, controlled movements.
Safety Tips
Safety is paramount when performing exercises, especially for seniors. Consider these tips to ensure a safe and effective physiotherapy routine:
- Consult a Professional: Always seek guidance from a qualified physiotherapist before starting any new exercise program.
- Start Slowly: Begin with low-intensity exercises and gradually increase intensity to avoid overexertion.
- Use Proper Equipment: Ensure that any exercise equipment is appropriate and in good condition to prevent accidents.
- Listen to Your Body: Pay attention to any discomfort or pain and stop the activity if necessary.
Call us today to learn more and get started!
Physiotherapy can be highly beneficial for individuals suffering from knee osteoarthritis (OA) by addressing pain, improving function, and enhancing the overall quality of life.
What is Knee Osteoarthritis (OA)?
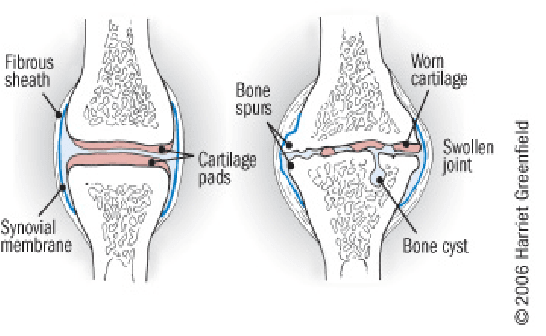
Knee OA is a degenerative joint disease that is typically a result of wear and tear and causes progressive loss of the articular cartilage of the joint.
What are the causes of Knee OA?
Knee osteoarthritis (OA) is a complex condition influenced by a variety of factors. Here are the primary causes and contributing factors:
1. Aging
- Natural Wear and Tear: As people age, the cartilage that cushions the knee joint gradually wears away, leading to OA.
- Decreased Ability to Heal: Older cartilage has a reduced ability to repair itself, making it more susceptible to damage.
2. Genetics
- Family History: Genetic predisposition can play a significant role. If OA runs in your family, you might be more likely to develop it.
- Genetic Mutations: Certain genetic mutations can affect cartilage production and maintenance.
3. Joint Injuries
- Previous Injuries: Injuries such as fractures, ligament tears, or meniscus damage can increase the risk of OA.
- Repetitive Stress Injuries: Repeated stress or overuse of the knee joint, often due to occupational or recreational activities, can lead to OA.
4. Obesity
- Increased Joint Load: Excess body weight puts additional stress on the knee joints, accelerating cartilage breakdown.
- Inflammation: Fat tissue produces inflammatory chemicals that can contribute to joint damage.
5. Mechanical Factors
- Joint Alignment: Abnormal joint alignment, such as bowlegs or knock-knees, can increase stress on certain parts of the knee.
- Muscle Weakness: Weak muscles around the knee, particularly the quadriceps, can lead to increased joint stress.
6. Gender
- Higher Risk in Women: Women, especially those over 50, are more likely to develop knee OA compared to men. Hormonal differences might contribute to this increased risk.
7. Metabolic and Systemic Factors
- Metabolic Syndrome: Conditions like diabetes and metabolic syndrome are associated with an increased risk of OA due to systemic inflammation and metabolic disturbances.
- Inflammatory Diseases: Conditions such as rheumatoid arthritis can predispose individuals to secondary OA.
8. Lifestyle Factors
- Physical Activity: Both excessive and insufficient physical activity can affect joint health. High-impact sports can lead to joint injuries, while sedentary lifestyles can weaken muscles and joints.
- Diet: Poor nutrition can affect joint health. For example, deficiencies in vitamins D and C can impair cartilage maintenance and repair.
9. Joint Biomechanics
- Meniscus Tears: Damage to the meniscus can disrupt joint mechanics and contribute to OA.
- Ligament Damage: Injuries to ligaments, such as the ACL, can destabilize the knee and lead to abnormal wear patterns.
10. Inflammation
- Low-Grade Inflammation: Chronic low-grade inflammation can contribute to the breakdown of cartilage and other joint tissues.
Understanding these causes and contributing factors can help in the prevention and management of knee osteoarthritis, emphasizing the importance of maintaining a healthy lifestyle, avoiding joint injuries, and seeking early intervention for symptoms.
What are the most common symptoms of Knee OA?
Knee osteoarthritis (OA) typically presents with a range of symptoms that can vary in intensity from mild to severe. The most common symptoms include:
1. Pain
- Activity-Related Pain: Pain that worsens with activity or weight-bearing and improves with rest.
- Persistent Pain: Chronic pain that may be present even at rest or during the night in more advanced stages.
2. Stiffness
- Morning Stiffness: Stiffness in the knee that is usually worse in the morning or after periods of inactivity and typically lasts less than 30 minutes.
- Post-Activity Stiffness: Stiffness that occurs after prolonged sitting or resting.
3. Swelling
- Joint Swelling: Swelling around the knee joint due to inflammation or increased production of joint fluid.
- Effusion: Accumulation of excess fluid within the knee joint, leading to noticeable swelling.
4. Reduced Range of Motion
- Limited Flexibility: Difficulty bending or straightening the knee fully.
- Loss of Motion: Progressive decrease in the knee’s range of motion over time.
5. Grinding Sensation (Crepitus)
- Audible Cracking or Popping: A sensation of grinding, cracking, or popping sounds when moving the knee, often due to roughened cartilage surfaces.
6. Weakness or Instability
- Feeling of Giving Way: A sensation that the knee might buckle or give out, often due to muscle weakness or joint instability.
- Muscle Weakness: Weakness in the muscles surrounding the knee, particularly the quadriceps.
7. Deformity
- Joint Deformities: Changes in the shape of the knee joint, such as bowlegged (varus) or knock-kneed (valgus) appearance, due to uneven wear and joint damage.
8. Tenderness
- Joint Tenderness: Tenderness or pain when pressing on or around the knee joint.
9. Functional Impairment
- Difficulty with Activities: Challenges with everyday activities such as walking, climbing stairs, sitting, or standing due to pain and stiffness.
- Reduced Mobility: Decreased ability to perform normal daily activities and exercise.
10. Fatigue
- General Fatigue: Feeling of tiredness and reduced energy levels, often due to chronic pain and sleep disturbances.
These symptoms can significantly impact an individual’s quality of life and ability to perform daily activities. Early recognition and management of knee OA symptoms can help slow disease progression and improve function and comfort.
What are the treatment options for Knee OA?
The number 1 treatment option is conservative management (ie. Patient education, therapeutic exercise, activity modification, weight loss, bracing), surgery should be considered after a conservative approach (talk to your orthopaedic specialist for more information).
Physiotherapy can help by providing you with education about osteoarthritis, tailor an exercise program that is suitable for you, help you consider the best options for activity modifications, provide you with education on bracing, address psychosocial factors such as fear-avoidance, promote patient autonomy and get you back to doing the things you love to do!
Manual therapy- joint mobilization to help with stiffness. Muscle energy technique to help stretch surrounding muscles.
Modalities – heat/ice for pain relief, TENs/IFC for pain relief and inflammation control. Ultrasound for pain relief.
Exercises – help with improving mobility, ROM, strength, balance, aerobic capacity, promoting physical function, reducing knee pain and inflammation.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy can be a highly effective treatment for managing knee osteoarthritis by improving mobility, reducing pain, and enhancing overall function. Whether you are looking for physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are experienced physiotherapists ready to help you manage osteoarthritis and improve your quality of life.
Arthritis is a term used to describe inflammation of one or more joints, leading to pain, stiffness, and decreased mobility. There are many types of arthritis, but the two most common are osteoarthritis and rheumatoid arthritis.
What are the two most common types of Arthritis?
- Osteoarthritis (OA): This is the most common form of arthritis, often associated with aging or wear and tear on the joints. In OA, the protective cartilage that cushions the ends of bones wears down over time, leading to pain, swelling, and stiffness in the affected joint. Osteoarthritis can affect any joint but commonly occurs in the hands, knees, hips, and spine.
- Rheumatoid Arthritis (RA): Unlike osteoarthritis, rheumatoid arthritis is an autoimmune disorder in which the body’s immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints. This leads to inflammation, joint damage, and eventually erosion of the bone and cartilage. RA commonly affects the joints in the hands, wrists, and feet and can cause systemic symptoms such as fatigue, fever, and weight loss.
What are the causes of Arthritis?
While the causes of some forms of arthritis are unknown, arthritis can be caused by disease, injury, overuse and genetic predisposition.
What are 8 foods to avoid when you have arthritis?
When managing arthritis, it’s often recommended to avoid certain foods that may exacerbate inflammation or contribute to joint pain. Here are eight foods commonly suggested to avoid:
- Processed Foods: Foods high in processed sugars, refined carbohydrates, and unhealthy fats can contribute to inflammation. These include fast foods, sugary snacks, and processed meats.
- Saturated and Trans Fats: Foods high in saturated and trans fats, such as fried foods, processed snacks, and fatty cuts of meat, can promote inflammation and worsen arthritis symptoms.
- High Sodium Foods: Excessive sodium intake can lead to water retention and inflammation, potentially aggravating arthritis symptoms. Processed foods, canned soups, and salty snacks are common sources of high sodium.
- Nightshade Vegetables: Some individuals with arthritis find that nightshade vegetables like tomatoes, eggplants, peppers, and potatoes can worsen their symptoms. While more research is needed, some believe that certain compounds in these vegetables may contribute to inflammation in susceptible individuals.
- Gluten: For some people with arthritis, particularly those with rheumatoid arthritis, gluten may exacerbate inflammation and joint pain. Gluten is found in wheat, barley, rye, and products made from these grains.
- Dairy Products: Some people with arthritis may find that dairy products worsen their symptoms. While the evidence is mixed, some studies suggest that certain proteins in dairy may contribute to inflammation in susceptible individuals.
- Alcohol: Excessive alcohol consumption can lead to inflammation and may worsen arthritis symptoms. Additionally, alcohol can interact with some medications used to treat arthritis.
- Sugar-Sweetened Beverages: Sugary drinks like sodas and fruit juices can contribute to inflammation and weight gain, which may exacerbate arthritis symptoms. Opting for water, herbal teas, or unsweetened beverages is a better choice.
It’s important to note that individual responses to these foods can vary, and it may be helpful to keep a food diary to identify any specific triggers. Additionally, maintaining a balanced diet rich in fruits, vegetables, lean proteins, and healthy fats is generally beneficial for managing arthritis symptoms. Consulting with a healthcare professional or a registered dietitian for personalized dietary advice is also recommended.
What foods can I eat when I have arthritis?
Here are some foods that are often recommended for people with arthritis:
- Fatty Fish: Fatty fish like salmon, mackerel, sardines, and trout are rich in omega-3 fatty acids, which have anti-inflammatory properties. Consuming fatty fish regularly may help reduce inflammation and alleviate arthritis symptoms.
- Fruits and Vegetables: Colorful fruits and vegetables are high in antioxidants and other nutrients that can help reduce inflammation and promote overall health. Aim for a variety of fruits and vegetables, including berries, cherries, oranges, leafy greens, broccoli, and bell peppers.
- Whole Grains: Whole grains like brown rice, quinoa, oats, and whole wheat are rich in fiber and nutrients that can help support joint health. Choose whole grains over refined grains to maximize nutritional benefits.
- Nuts and Seeds: Nuts and seeds, such as almonds, walnuts, flaxseeds, and chia seeds, are good sources of healthy fats, protein, and antioxidants. They can help reduce inflammation and provide essential nutrients for joint health.
- Legumes: Legumes like beans, lentils, and chickpeas are rich in protein, fiber, and various vitamins and minerals. They can be a nutritious and filling addition to meals, providing plant-based protein and promoting overall health.
- Legumes: Legumes like beans, lentils, and chickpeas are rich in protein, fiber, and various vitamins and minerals. They can be a nutritious and filling addition to meals, providing plant-based protein and promoting overall health.
- Herbs and Spices: Certain herbs and spices have anti-inflammatory properties and can add flavor to meals without extra salt or unhealthy fats. Examples include turmeric, ginger, garlic, cinnamon, and rosemary.
- Dairy Alternatives: For individuals sensitive to dairy, alternatives like fortified plant-based milk (e.g., almond milk, soy milk) and dairy-free yogurt or cheese can provide calcium and other nutrients without exacerbating arthritis symptoms.
What is the best treatment for arthritis?
It’s important for individuals with arthritis to work closely with their healthcare providers to develop a comprehensive treatment plan tailored to their specific needs and preferences. This may involve a combination of medication, physiotherapy, lifestyle modifications, and other interventions to effectively manage symptoms and improve quality of life.
How do I book an appointment at a Triangle Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Managing arthritis involves not only proper diet but also effective physical therapy. For comprehensive care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can help manage arthritis symptoms and improve your quality of life through tailored treatment plans.
Winter weather can be challenging for individuals with arthritis, as cold temperatures and changes in atmospheric pressure can exacerbate joint pain and stiffness. Here are 10 tips to help manage arthritis during the winter months:
- Stay Warm:
- Start your day by using a heating pad or a warm bath or shower to increase the mobility in your joints and reduce pain before you go about your day.
- Dress in layers to trap heat and stay warm.
- Use heated blankets or warm packs on achy joints.
- Protect Your Joints:
- Wear gloves to keep your hands warm and protect your finger joints.
- Use knee-high socks and warm footwear to keep your feet and ankles insulated.
- Stay Active:
- Engage in gentle exercises to keep your joints flexible.
- Consider indoor activities like swimming, which is easy on the joints.
- Maintain a Healthy Weight:
- Excess weight can put more pressure on your joints, so try to maintain a healthy weight through a balanced diet and regular exercise.
- Stay Hydrated:
- Cold weather can lead to dehydration, which may worsen arthritis symptoms. Drink plenty of water to stay hydrated.
- Use Assistive Devices:
- Consider using assistive devices such as canes or braces to reduce the strain on affected joints.
- Manage Stress:
- Stress can exacerbate arthritis symptoms. Practice stress-reducing techniques like deep breathing, meditation, or yoga.
- Warm Up Before Activities:
- Before heading outdoors, warm up your body with gentle stretching exercises to prepare your joints for movement.
- Take Warm Baths:
- Soaking in a warm bath can help soothe joint pain and relax your muscles.
- Consult Your Doctor:
- Keep your healthcare provider informed about changes in your symptoms and discuss any concerns you have about managing arthritis in the winter.

Remember, it’s essential to tailor these tips to your specific situation, as arthritis can affect individuals differently. Always consult with your healthcare provider for personalized advice and treatment options.
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Winter weather can be challenging for those with arthritis, but with the right care, you can manage your symptoms effectively. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists can help you develop strategies to stay active and pain-free during the colder months.”
Physiotherapy can be beneficial for individuals with arthritis. Arthritis is a condition that involves inflammation and stiffness of the joints, leading to pain and reduced mobility. Physiotherapy aims to improve joint function, alleviate pain, and enhance overall quality of life through various techniques and exercises. Here are some frequently asked questions (FAQs) about physiotherapy and its role in managing arthritis:
What is arthritis or osteoarthritis?

- Arthritis, also known as Osteoarthritis (OA), is one of the most common causes of a decrease in mobility and an increase in disability among older adults. It is a common condition affecting the joints, most often the knees, hips, lower back, neck, and fingers.
- In a typical joint, there is a smooth layer of cartilage over the surfaces of the bones. This cartilage has several purposes, including distributing weight evenly during movement to minimize friction and absorb any shock.
- In OA, this cartilage breaks down and causes bones to rub against each other, producing pain and, therefore, disuse of that joint. Muscle weakness due to decreased use is a commonly associated issue in osteoarthritis, which affects function and mobility in many ways.
Can physiotherapy help with the pain?
Yes, physiotherapy can help manage arthritis pain by utilizing techniques such as manual therapy, joint mobilization, and soft tissue manipulation. These techniques can help reduce pain and improve joint function.
Can physiotherapy prevent joint deformities in arthritis patients?
Early intervention through physiotherapy can help prevent or minimize joint deformities by maintaining joint function, improving muscle balance around the affected joints, and promoting proper biomechanics.
Can physiotherapy reduce the need for medication?
In some cases, successful physiotherapy can lead to reduced reliance on pain medications or other arthritis-related drugs. However, this should always be discussed with a healthcare professional.
How long does it take to see results from physiotherapy for arthritis?
The timeline for seeing results can vary based on the severity of arthritis, the individual’s response to treatment, and consistency in following the physiotherapy program. Some individuals may experience improvements within a few weeks, while others might require more time.
Is physiotherapy suitable for all types of arthritis?
Physiotherapy can be beneficial for various types of arthritis, including osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. However, the approach may vary depending on the specific type and individual needs.
At Physiotherapy Oakville, our experienced physiotherapists create customized treatment plans tailored to the type of arthritis you have and your unique requirements. Scientific research supports the effectiveness of physiotherapy in managing arthritis symptoms, reducing pain, and improving joint function. By joining Physiotherapy Oakville, you can take advantage of evidence-based treatments and individualized care strategies that help you manage arthritis more effectively, enhance your quality of life, and maintain your mobility and independence.
How can strength training help arthritis?
- The strength in the muscles surrounding a joint is directly related to the progression of osteoarthritis. Studies show that muscle weakness after decreased use of the joint due to pain can actually make OA progress faster, further exacerbating the disability. In normal aging, there can already be some underlying muscle wasting or weakness, making function even more difficult.
- The goals of strength training are to decrease pain, protect against worsening of the condition, and improve self-efficacy and general health/well-being. Below are some ways strength training can help OA:
- Improve joint mechanics by offloading the join with stronger muscles
- Reduce joint pain by normalizing neural firing patterns
- Decrease cartilage degeneration by decreasing inflammatory chemicals in the body that breakdown cartilage
- Decrease depression and anxiety by increasing self-efficacy, independence, and mobility
- Older adults without existing osteoarthritis can lower their chances of getting it with increased strength!
What does the evidence show?
- Pain decreased by almost 50% in as little as 2 months of strength training
- Improve walking distance by 30-45%
- Significantly decrease progression of OA in the long-term, up to 30 months after beginning strengthening exercise
What are some of the changes I can expect to see after seeing a physiotherapist?
Changes you will see!
- Easier to go up and down the stairs
- Less pain during squatting and kneeling tasks
- Ability to walk longer and faster, allowing you to enjoy outdoor activities
- Better mood and decreased emotional stress
What are some exercises to do for arthritis?
Examples of exercises
- Swimming
- great for taking the weight of your joints but challenging your muscles against the weight of the water!
- Squatting up and down from a chair
- You do this every day and it will translate directly into easier activities of daily living!
- Biking
- Another very functional, strengthening exercise that also incorporates aerobic training to increase overall health
- Single leg balance
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Physiotherapy can play a significant role in managing arthritis by improving joint function and reducing pain. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you develop a personalized treatment plan to manage arthritis and enhance your quality of life.”





