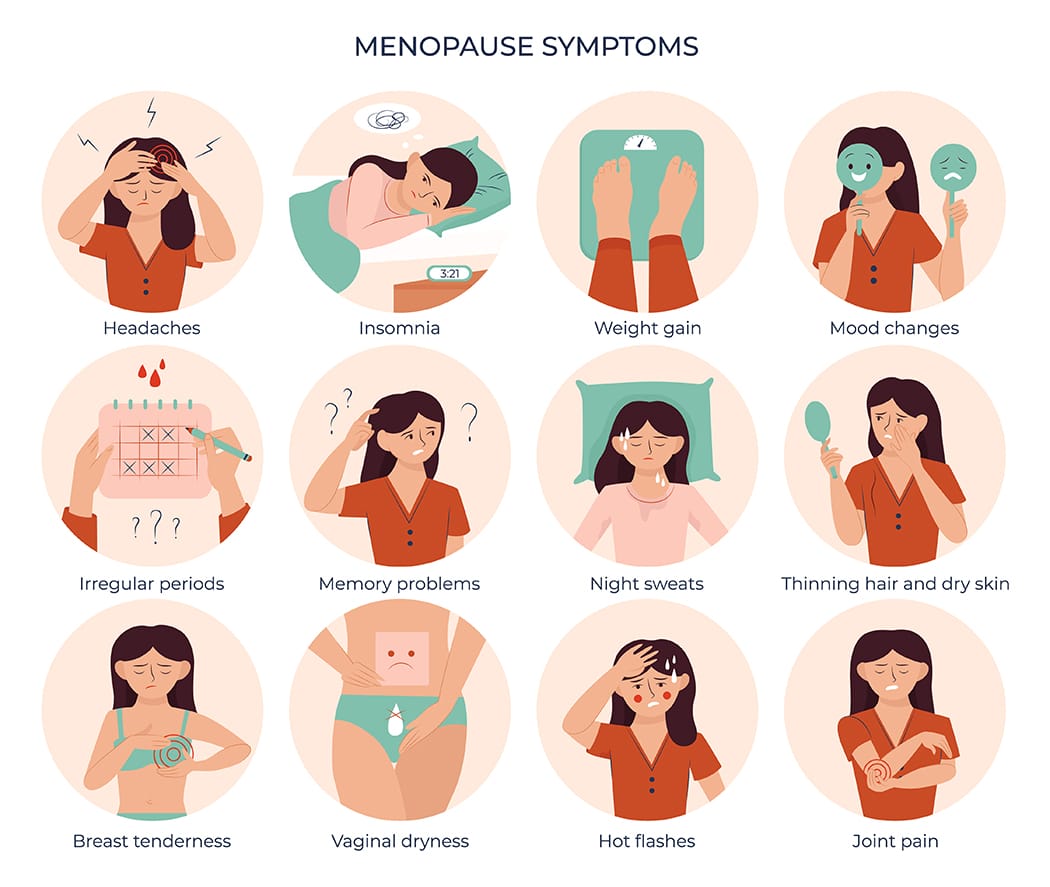
After menopause, women face an increased risk of knee injuries due to hormonal changes, decreased muscle strength, and other age-related factors. These changes, combined with weight gain and joint instability, can make the knees more vulnerable. However, with the right prevention strategies, knee injuries can be minimized, allowing you to stay active and pain-free. Give us a call at one of our Toronto locations and our physiotherapists at Triangle Physiotherapy can help you.
What Causes Knee Injuries in Post-Menopausal Women?
Several factors contribute to knee injuries in post-menopausal women, including:
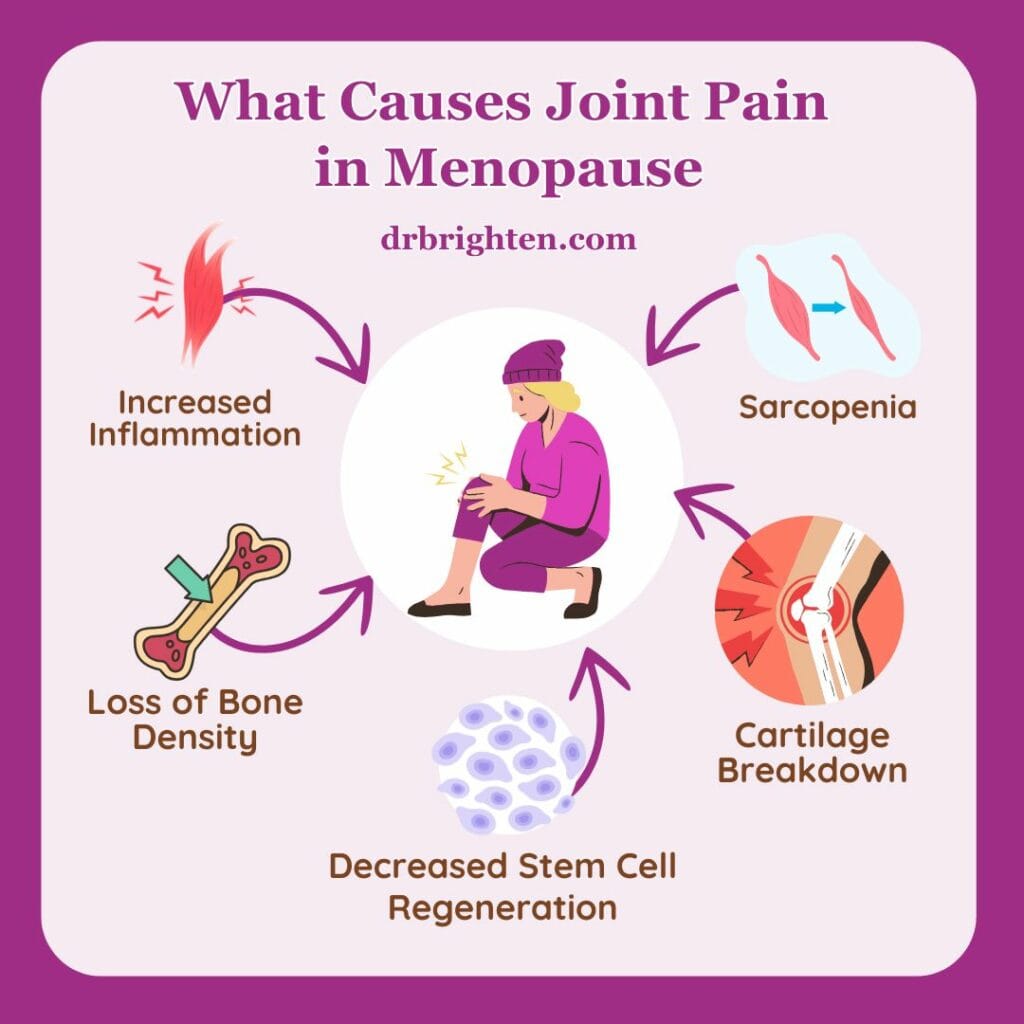
- Hormonal Changes: The drop in estrogen after menopause can weaken bones, muscles, and ligaments, increasing the risk of knee injuries.
- Muscle Weakness: Aging leads to a natural decline in muscle mass, which weakens the muscles surrounding the knee, leaving it less supported.
- Joint Instability: Weakened muscles and bones contribute to joint instability, making the knee more prone to sprains, strains, and tears.
- Weight Gain: Many women gain weight after menopause, which places added stress on the knee joints, leading to pain and increasing the risk of conditions like osteoarthritis.
Common Knee Injuries Post-Menopause
Some of the most common knee injuries women face include:
- Osteoarthritis: A condition where the knee’s cartilage wears down, causing pain and stiffness.
- Patellofemoral Pain Syndrome: Pain around the kneecap often caused by overuse or poor alignment.
- Ligament Injuries: Sprains or tears in the knee’s ligaments, such as the ACL or MCL, from sudden movements or falls.
- Tendonitis: Inflammation of the tendons, usually due to overuse or muscle imbalances.
Preventing Knee Injuries
Here are some essential physiotherapy tips to help prevent knee injuries post-menopause:
- Strengthen Muscles Around the Knee: Build strength in the quadriceps, hamstrings, and calves through exercises like squats and lunges to support the knee joint.
- Maintain a Healthy Weight: Extra weight adds stress to the knees, so managing weight through diet and exercise can reduce knee strain.
- Increase Mobility: Stretching the quadriceps, hamstrings, and calves can prevent tightness, but having overall mobility helps keep the joints healthy.
- Low-Impact Exercises: Activities like swimming, cycling, or walking are easier on the knees while still strengthening muscles and improving cardiovascular health.
- Strengthen Core and Hips: Strong core and hip muscles improve overall stability, reducing strain on the knees.
- Wear Supportive Footwear: Shoes with proper arch support and cushioning can reduce stress on the knees, especially during physical activities.
- Use Proper Technique: Ensure correct form when exercising, lifting, or performing daily tasks to avoid unnecessary stress on the knees.
- Balance Exercises: Improve stability and prevent falls with exercises that challenge balance, such as standing on one leg.
Managing Knee Injuries
If knee pain or injury occurs, here are some strategies for managing it:
- Physiotherapy: A physiotherapist can design a program to improve strength, flexibility, and mobility, helping you recover and prevent further injury.
- Braces or Sleeves: Knee supports can provide stability and reduce pain during activity.
Conclusion
Post-menopausal women are at higher risk for knee injuries, but with proactive care, the risk can be minimized. Strengthening the knee muscles, maintaining a healthy weight, and practicing good form are key to keeping your knees healthy. If knee pain occurs, working with a physiotherapist and using the right treatments can help you stay active and injury-free. Book an appointment with one of the physiotherapists at Triangle Physiotherapy in Toronto to get help today!
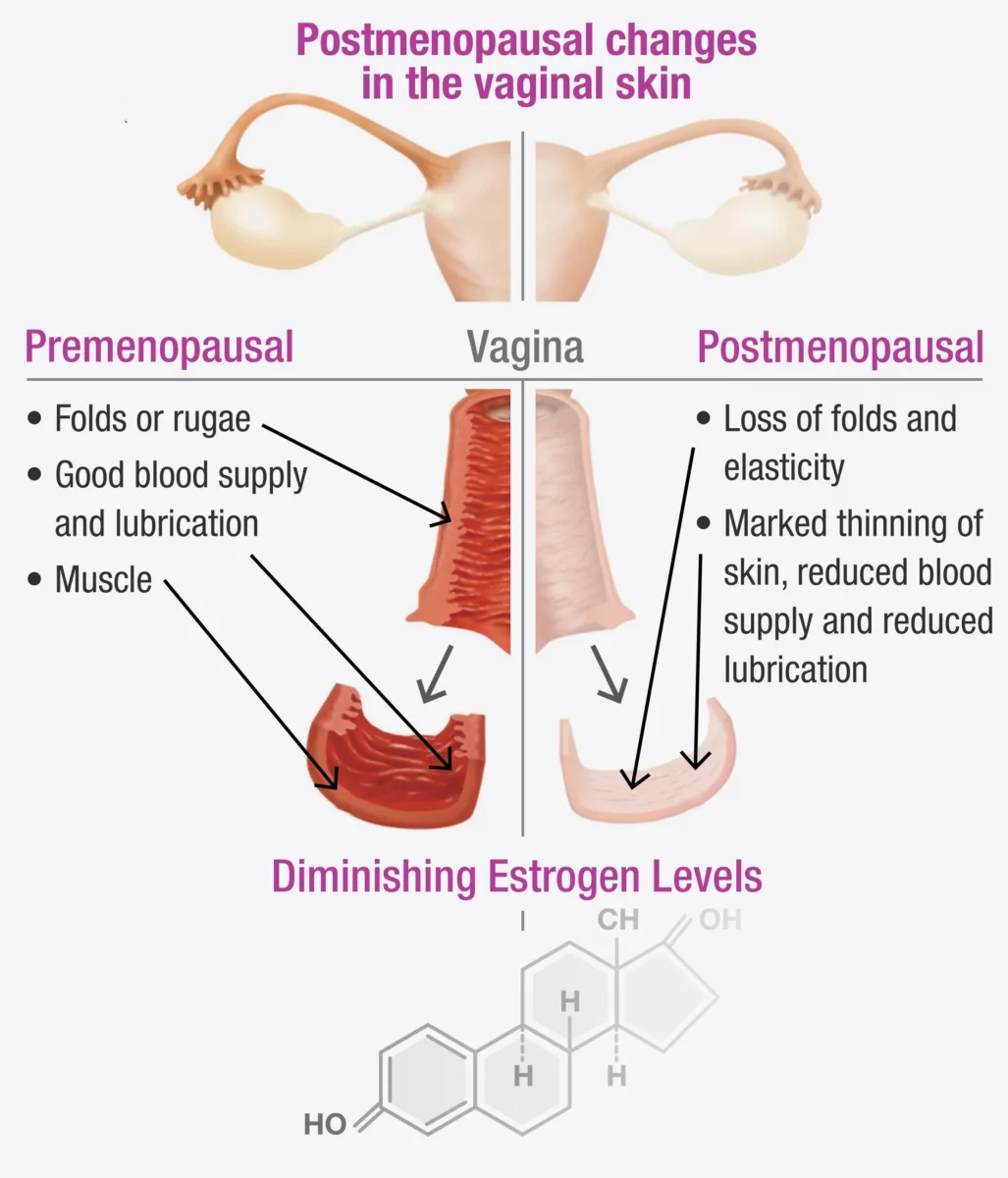
Vaginal atrophy, also known as atrophic vaginitis, is a condition that many women experience, especially after menopause. It involves changes in the vaginal area that can cause discomfort and other symptoms. Fortunately, our pelvic health physiotherapists in North York can help manage these symptoms and improve your quality of life.
What is Vaginal Atrophy?
Vaginal atrophy often happens during menopause when the levels of estrogen, a hormone in a woman’s body, decrease. When this happens, it can lead to:
- Dryness: The vagina becomes less moist, leading to dryness and irritation.
- Thinning of Vaginal Walls: The walls of the vagina become thinner and less flexible.
- Inflammation and Redness: The vaginal area can become inflamed and red, causing pain.
- Urinary Symptoms: You might experience more frequent urination, a strong urge to urinate, or urinary tract infections (UTIs).
These changes can make everyday activities uncomfortable and affect your sex life.
If vaginal atrophy is not treated and a woman continues to experience painful intercourse, the vaginal muscles may react by tightening to protect the body. Over time, this tightening can become an automatic response (vaginismus) that continues even after the atrophy has been treated.
Fortunately, both conditions can be treated with the help of a pelvic health Physiotherapist in North York. In fact, it is often necessary to treat vaginal atrophy and vaginismus together, as addressing one without the other can be challenging.
Symptoms to Watch For
You might have vaginal atrophy if you notice:
- Pain During Sex: Painful intercourse (called dyspareunia) is a common symptom.
- Itching or Burning: These sensations can be uncomfortable and persistent.
- Frequent UTIs: More urinary tract infections than usual.
- Vaginal Bleeding or Discharge: Unusual bleeding or discharge can occur.
- Difficulty Urinating: Problems with urination, such as a strong urge or pain.
Recognizing these symptoms early can help you get the treatment you need sooner.
How a Pelvic Health Physiotherapist Can Help with Menopause and Vaginal Atrophy
A pelvic health physiotherapist is a specialist who focuses on the muscles and tissues in the pelvic area. They can provide various treatments to help manage vaginal atrophy. Here’s how they can assist:
1. Assessment and Diagnosis
The first step is a thorough check-up, which includes:
- Reviewing Your Medical History: Discussing your symptoms, medical history, and any medications you are taking.
- Physical Examination: Checking the condition of your vaginal walls, pelvic floor muscles, and surrounding tissues.
2. Customized Exercise Programs
These physiotherapists create specific exercise programs to strengthen and relax your pelvic floor muscles. These exercises can:
- Improve Muscle Tone: Making the vaginal muscles stronger and more flexible.
- Boost Blood Flow: Increasing circulation to help with healing and tissue health.
3. Manual Therapy and Techniques
Hands-on techniques are used to improve the flexibility and function of your pelvic area, such as:
- Myofascial Release: Reducing tension in the pelvic muscles.
- Scar Tissue Mobilization: Addressing any scarring or adhesions in the vaginal area.
4. Education and Lifestyle Advice for Menopause
Education is a key part of therapy, including advice on:
- Diet and Hydration: Eating a balanced diet and staying hydrated for overall health.
- Relaxation Techniques: Learning how to relax your pelvic floor muscles to reduce discomfort.
5. Use of Devices and Modalities
They might suggest using certain devices and techniques, such as:
- Vaginal Dilators: These help gently stretch the vaginal walls, making them more flexible.
- Electrostimulation: Using mild electrical impulses to strengthen pelvic muscles.
How do I find a pelvic health physiotherapist in North York?
We have 8 locations with pelvic health physiotherapists to help you. If you are going through menopause and are seeing signs of vaginal atrophy, Book an Appointment today!
Pelvic Health Physiotherapists in North York:
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
At Triangle Physiotherapy, we understand that conditions like menopause and vaginal atrophy can significantly impact your quality of life. Our team of experienced professionals is here to help you through specialized physiotherapy treatments designed to address these and other related concerns. Whether you’re seeking Physiotherapy in Etobicoke, Physiotherapy in Oakville, Physiotherapy in North York, or Physiotherapy in Toronto, we have clinics conveniently located across the region. Visit us at Physiotherapy Lawrence Park, Physiotherapy Clinic Queens Quay, Physiotherapy Erin Mills, Physiotherapy Mississauga, or Physiotherapy Liberty Village to start your journey towards better health and well-being.



