A Quiet Strength That Deserves Care
At Triangle Physiotherapy, we believe some of the most important muscles in your body are also the most overlooked. Your pelvic floor plays a vital role in posture, movement, bladder and bowel control, and overall core stability. When it’s not functioning at its best, daily life can feel uncomfortable or limiting. That’s where pelvic floor physiotherapy comes in – gentle, targeted care designed to restore balance, strength, and confidence.
What Is Pelvic Floor Physiotherapy?
Pelvic floor physiotherapy focuses on assessing and treating the muscles, joints, and connective tissues of the pelvic region. These muscles support your spine and hips and work closely with your core. At our clinic, we take a respectful, evidence-based approach, creating personalized treatment plans that may include guided exercises, breathing techniques, posture correction, and movement education.
Whether symptoms are related to pregnancy, postpartum recovery, sports, prolonged sitting, or everyday stress, pelvic physiotherapy can help improve function and comfort – without judgment and at your pace.
Why Toronto Residents Choose Pelvic Physiotherapy

Living in a fast-paced city like Toronto often means long commutes, desk-based work, and limited recovery time. These factors can place extra strain on the pelvic region. Many people searching for pelvic physiotherapy near me are surprised to learn how common pelvic floor issues are – and how effective physiotherapy can be.
At Triangle Physiotherapy, our goal is not just symptom relief, but long-term improvement. We empower you with knowledge and tools so you feel confident moving through daily life again.
Pelvic Floor Physiotherapy in Etobicoke and Across Toronto
If you’re looking for pelvic floor physiotherapy Etobicoke or elsewhere in the city, our team is proud to serve diverse Toronto communities. We work closely with each client, listening carefully and adjusting care as your body progresses. This personalized approach is why many of our clients consider us among the options when searching for the best physiotherapist in Toronto.
Our clinic blends clinical expertise with a welcoming environment, making Physiotherapy Toronto residents can trust accessible and supportive.
A Triangle Physiotherapy Promise
We see pelvic physiotherapy as a partnership. Your body has an incredible ability to heal when given the right guidance. At Triangle Physiotherapy, we’re here to guide, educate, and support you every step of the way.
If you’re ready to restore balance, rebuild strength, and regain confidence, pelvic floor physiotherapy may be the missing piece. We’re proud to be part of your journey toward better movement and better living – right here in Toronto.
Moving to a new country brings change – new routines, new languages, and often, new health challenges. For many immigrant and refugee women, pelvic health may not be something they’ve had the space or support to focus on. But whether you’re healing after childbirth, living with persistent discomfort, or noticing changes to your bladder or bowel habits, pelvic floor therapy can help.
At Triangle Physiotherapy, we understand that seeking this kind of care can feel intimidating – especially when it’s unfamiliar or culturally sensitive. That’s why we take a respectful, understanding approach to help women from all walks of life get the care they need with dignity.
What Is Pelvic Floor Therapy?
Your pelvic floor is a group of muscles that support the bladder, uterus, and bowel. These muscles can weaken or tighten due to childbirth, trauma, menopause, chronic stress, or even from long-term habits like holding in urine. When your pelvic floor isn’t functioning well, it can lead to symptoms like:
- Leaking urine when you laugh, cough, or lift something
- Pain during intimacy
- Pressure or heaviness in the pelvis
- Difficulty going to the bathroom
- Lower back or hip pain
Pelvic floor therapy is a specialized form of physiotherapy that focuses on restoring strength, mobility, and coordination to these muscles.
Why Cultural Sensitivity Matters

In many cultures, talking about pelvic health is uncomfortable – or even considered off-limits. Some women may have never heard of pelvic therapy before. Others may feel uncertain about what an assessment involves, or fear being judged for asking questions. We hear you. And we’re here to change that experience.
Our physiotherapists are trained to communicate with empathy and simplicity – using plain language, educational visuals, or even interpreter support where needed. We honour each person’s comfort level, and always explain every step before proceeding. You’ll never be rushed, and you’ll always have the option to say “no” or “not today.”
Supporting the Whole Person
For many women who’ve experienced displacement, violence, or trauma, the body holds more than physical tension – it holds emotional memory too. That’s why we offer trauma-informed care, meaning we work with extra gentleness, respect, and awareness of your emotional state. Your trust is never assumed – it’s earned over time.
Financial Support Through IFHP
We’re proud to support newcomers who are eligible under the Interim Federal Health Program (IFHP), which may cover pelvic physiotherapy services. If you’re unsure whether you qualify, our team can help guide you through the process.
Small Steps, Big Changes
You don’t need to live with discomfort. You don’t need to feel embarrassed. You deserve care that sees you as a whole person – not just a patient. At Triangle Physiotherapy, we’re committed to creating a safe, welcoming space where healing feels possible.
If you’re new to Canada and navigating pelvic health concerns, we invite you to book a private session with one of our skilled therapists. We’re here to listen, support, and help you reclaim your strength – one step at a time.
Becoming a mother in a new country comes with more than sleepless nights and diaper changes. For many refugee and newcomer women, the postpartum period is layered with physical healing, emotional weight, and the challenges of adjusting to a new life – often without extended family or familiar support systems.
At Triangle Physiotherapy, we believe that every mother deserves to heal with dignity – especially those who’ve endured the hardships of displacement, trauma, or migration. Postpartum pelvic floor therapy is one important step toward feeling whole again, and we’re here to make that journey a safe and supported one.
The Hidden Struggles After Birth
After childbirth, it’s common to experience pelvic floor symptoms such as:
- Leaking urine when coughing, sneezing, or laughing
- A feeling of heaviness or pressure in the pelvic area
- Pain during intercourse
- Core weakness or back pain
- Difficulty controlling bowel or bladder movements
In many cases, these symptoms are brushed aside as “normal,” especially in communities where pelvic health isn’t openly discussed. But just because something is common doesn’t mean you have to live with it.
A Safe Space to Heal
We know that seeking care for intimate concerns can feel overwhelming – especially if you’re navigating language barriers, unfamiliar healthcare systems, or past trauma. That’s why our approach is gentle, respectful, and culturally aware.
Our physiotherapists use plain language, explain every step, and offer flexible options based on your comfort level. Interpreter services or visual aids are available when needed, and your privacy is always respected. We want you to feel seen, not rushed.
You’ll never be made to feel ashamed of your body, your experience, or your questions.
Why Pelvic Therapy Matters for Refugee Mothers

Many refugee mothers have gone through high-stress pregnancies or deliveries in challenging environments. Some may have experienced traumatic births, long journeys, or physical strain without access to postpartum care. These experiences can affect how the body recovers—and how safe you feel in your own skin.
Pelvic floor therapy helps rebuild strength, relieve pain, and restore control over your body. But beyond that, it’s about giving you back a sense of confidence, autonomy, and peace – because you deserve to feel like yourself again.
Coverage Through IFHP
Triangle Physiotherapy offers services covered under the Interim Federal Health Program (IFHP) for eligible refugee patients. If you’re unsure about your coverage or how to access care, our team will guide you through each step – no judgment, just support.
You Are Not Alone
If you’re a postpartum refugee mom, know this: your healing matters. Your body has carried you through so much. You deserve care that honors not just your physical needs, but your story too.
At Triangle Physiotherapy, we’re here to walk beside you with compassion, clinical expertise, and a commitment to your recovery.
Reach out today. Let’s take that first step – together.
What to expect and how to feel empowered from day one
When it comes to pelvic health, there’s often a mix of curiosity, concern, and even confusion – especially if you’ve never seen a pelvic physiotherapist before. Whether you’re navigating postpartum recovery, persistent discomfort, or changes with age, know this: you’re not alone, and help is closer than you think.
At Triangle Physiotherapy North York, we know that walking into your first pelvic physiotherapy appointment can feel like a big step. That’s why we’ve created a safe, welcoming environment where education and empathy come first.
Here’s what to expect – plus some helpful prep tips so you can feel confident and informed ahead of your first visit.
What Is Pelvic Physiotherapy?
Pelvic physiotherapy focuses on the muscles, ligaments, and connective tissues that support the bladder, uterus (or prostate), and bowel. When these structures are weak, tight, or not working in coordination, it can lead to issues like:
- Bladder leaks or urgency
- Pain during sex
- Constipation
- Pelvic or lower back pain
- Heaviness or pressure in the pelvic region
- Discomfort during movement or exercise
Pelvic physiotherapy in North York is designed to assess and treat these concerns through a combination of hands-on therapy, targeted exercises, posture training, and patient education.
What Happens at Your First Appointment?

Your first session at Triangle Physiotherapy North York will feel a lot like a detailed conversation mixed with gentle movement-based assessment.
Here’s a breakdown of what to expect:
- History & Concerns: We start with your story. This includes your symptoms, medical background, lifestyle habits, and any previous injuries or surgeries.
- Education & Consent: We explain how the pelvic floor functions and what could be contributing to your symptoms. If an internal assessment is helpful, it’s discussed with complete transparency and only done with your full, informed consent.
- Movement & Posture Check: You may be asked to walk, squat, or move in certain ways so we can observe muscle coordination and alignment.
- Personalized Plan: Based on your needs, we build a care plan with treatment goals, exercises, and follow-up recommendations.
The goal? Helping you feel heard, informed, and never rushed. You’re in charge of your journey – we’re simply your support team.
Tips Before You Arrive
- Wear comfy clothes that let you move freely
- Bring a list of symptoms, questions, or goals
- Come with an open mind – pelvic physio is often gentler and more holistic than people expect
Why Triangle Physiotherapy North York?
We take pride in being a trusted name for pelvic physiotherapy in North York, with an emphasis on:
- Respectful, patient-centered care
- Highly trained pelvic health therapists
- Private, one-on-one sessions
- Flexible scheduling and direct billing options
- A clinic culture that prioritizes comfort, dignity, and real progress
Your First Step Starts Here
Taking care of your pelvic health is nothing to be shy about – it’s an important part of your well-being. Whether you’re experiencing symptoms or just want to better understand your body, we’re here to help.
Book your initial pelvic physiotherapy session at Triangle Physiotherapy North York today. Your comfort, confidence, and health matter here.
When most people think of pelvic physiotherapy, they assume it’s only for women. But here’s the truth: men have pelvic floors too, and they can face serious health issues when those muscles aren’t functioning properly. Whether you’re recovering from surgery, dealing with chronic pelvic pain, or experiencing bladder or bowel issues, pelvic physiotherapy in Oakville could be the answer you’ve been looking for.
At Triangle Physiotherapy Oakville, we believe men’s pelvic health deserves attention, compassion, and expert care – just like any other health concern. So let’s talk about it.
What Is Pelvic Physiotherapy for Men?
Pelvic physiotherapy focuses on the muscles, ligaments, and tissues in the pelvic region. For men, this includes everything from the lower abdomen to the base of the spine – areas crucial for bladder, bowel, and sexual function.
Common conditions treated include:
- Urinary incontinence or urgency
- Erectile dysfunction
- Pelvic pain or discomfort
- Post-prostatectomy recovery
- Bowel control issues
- Pain during or after physical activity
These aren’t just “in your head” – they’re very real, physical issues that deserve professional care. And yes, there is help available at a physiotherapy clinic near me.
Why Men Often Don’t Talk About Pelvic Health
For many men – especially middle-aged adults, male refugees, or those recovering from surgery – talking about pelvic health can feel awkward or uncomfortable. But ignoring the symptoms doesn’t make them go away.
At Triangle Physiotherapy Oakville, we create a safe, respectful environment where you can talk openly and receive expert care from trained pelvic health professionals. We’re here to help, not to judge.
How Pelvic Physiotherapy Can Help

Still wondering how pelvic physiotherapy Oakville services actually work? Here’s what you can expect:
1. A Thorough Initial Assessment
We begin with a private, one-on-one consultation to understand your symptoms, health history, and goals. You’ll never be rushed or made to feel uncomfortable.
2. Customized Treatment Plan
Your treatment might include:
- Pelvic floor muscle retraining
- Breathing and posture techniques
- Manual therapy
- Bladder and bowel retraining
- Lifestyle and movement coaching
Our goal is long-term relief and restoring normal function – not just quick fixes.
3. Ongoing Support & Education
We’ll give you tools and techniques to manage symptoms at home, and we’ll be with you every step of the way.
If you’ve been Googling “best physiotherapist near me” for male pelvic issues – this is where your search ends.
Why Choose Triangle Physiotherapy Oakville?
Choosing a clinic for something as personal as pelvic health is a big step. Here’s why men trust Triangle Physiotherapy Clinic Near Me:
- Experienced pelvic health physiotherapists trained to work with male-specific conditions
- Confidential, one-on-one sessions in a private setting
- Customized, evidence-based treatment plans
- Convenient Oakville location with flexible appointments
Whether you’re dealing with post-surgical recovery, pelvic pain, or chronic urinary issues, our team is ready to help.
It’s Not “Too Late” or “Too Weird” – It’s Health
We get it. For many men, reaching out about pelvic health feels unfamiliar. But your quality of life matters. You don’t need to suffer in silence.
If you’ve been searching for pelvic physiotherapy Oakville, it’s time to take action. Triangle Physiotherapy offers the specialized care you need, in a place where you’ll feel respected and supported.
Book Your Appointment Today
Pelvic pain, incontinence, or dysfunction aren’t just “normal” signs of aging—they’re treatable. Don’t wait until the symptoms get worse.
📍 Looking for physiotherapy Oakville, or the best physiotherapist near me for men’s health issues?
📞 Book a consultation at Triangle Physiotherapy Oakville and start your journey toward recovery today.
Selecting an appropriate pelvic physiotherapy clinic is crucial for women’s recovery and long-term health. Whether you’re experiencing pelvic discomfort, issues related to pregnancy, postpartum recovery, or problems with bladder and bowel function, collaborating with a top pelvic health physiotherapist in Toronto guarantees you receive tailored and effective treatment. With numerous options available, the search for the right clinic can feel daunting, but it doesn’t have to be difficult.
We can help you identify what to consider when selecting a pelvic physiotherapy clinic in Toronto and how to find the best option for your specific requirements.
Why Pelvic Physiotherapy is Important for Women’s Health
Pelvic physiotherapy concentrates on the muscles, ligaments, and connective tissues in the pelvic area. These components are essential for supporting the bladder, uterus, and bowel, in addition to maintaining core stability and sexual health.
Here are several prevalent reasons why women pursue pelvic physiotherapy in Toronto:
- Postpartum recovery following vaginal or cesarean births
- Pelvic organ prolapse
- Urinary or fecal incontinence
- Pelvic discomfort or pain
- Pain during intercourse
- Preparation for childbirth
- Menstrual health issues
- Perimenopausal and menopausal symptoms
Engaging with a qualified pelvic health physiotherapist can assist you in regaining strength, enhancing functionality, averting long-term problems, and significantly improving your quality of life.
Key Factors to Consider When Choosing a Pelvic Health Clinic

Choosing the optimal pelvic physiotherapy clinic goes beyond just an online search.
Here’s what to consider:
- Qualifications and Specialization Seek out clinics that have physiotherapists with specialized training in pelvic health, such as certifications in pelvic floor rehabilitation, postpartum care, or women’s health specialties. Suggestion: Inquire about the therapist’s experience in treating your particular condition, like postpartum recovery or pelvic pain related to endometriosis.
- Detailed Assessment and Customized Treatment Plans The foremost physiotherapists in Toronto prioritize understanding your medical history and objectives. An initial comprehensive assessment should incorporate: An in-depth discussion regarding your symptoms and lifestyle A physical examination of your pelvic muscles (when appropriate) A tailored treatment plan that adapts as you make progress
- Privacy and Comfort as pelvic physiotherapy can be a personal experience, the clinic atmosphere should foster a sense of safety and respect. Look for: Private treatment rooms A caring and professional staff Transparent explanations about each step of the process
- Clinic Reputation and Feedback Investigate online reviews and testimonials to assess other patients’ experiences. You may also reach out to friends, family, or your healthcare provider for reliable recommendations on pelvic physiotherapy in Toronto.
- Convenient Location and Adaptable Scheduling Regularity is essential for recovery. A clinic conveniently situated near your home or workplace can facilitate consistent appointment attendance.
Questions to Ask Before You Book
To help you make an educated choice, consider asking these questions when assessing a pelvic physiotherapy clinic:
- What pelvic health certifications do your pelvic health physiotherapists possess?
- How long do assessment and follow-up sessions last?
- Will I have a dedicated physiotherapist throughout my treatment? Do you provide virtual consultations or follow-up care?
- What are the costs and insurance coverage options?
Benefits of Choosing the Right Pelvic Health Physiotherapist
Partnering with the right professional can offer transformative benefits, including:
- Accelerated Recovery: Specialized treatment supports safe and effective healing.
- Pain Relief: Target the underlying causes of pelvic discomfort.
- Increased Confidence: Regain mastery over your body and health.
- Ongoing Wellness: Prevent future complications through education and preventative measures.
By choosing a clinic with experienced therapists and a nurturing environment, you enhance your chances of success.
Final Thoughts: Prioritize Your Health and Comfort
Your pelvic wellness is intricately linked to your overall health. By selecting the top pelvic health physiotherapist in Toronto, you’re making a valuable investment in your future health, self-assurance, and quality of life. Dedicate time to explore clinics, inquire, and make sure you feel at ease with your care team. Finding the right match will make your healing journey more seamless and empowering.
FAQs About Pelvic Physiotherapy in Toronto
- How does pelvic physiotherapy differ from standard physiotherapy?
Pelvic physiotherapy specifically targets the muscles and tissues of the pelvic floor, whereas standard physiotherapy deals with general musculoskeletal issues.
- How many appointments will I require?
This depends on your specific condition. Some individuals notice progress after 4–6 sessions, while others might need ongoing treatment.
- Is pelvic physiotherapy included in insurance plans in Toronto?
The majority of extended health insurance plans do cover physiotherapy services. Be sure to verify your coverage with your provider.
- Can I begin pelvic physiotherapy while I’m pregnant?
Absolutely! In fact, prenatal pelvic physiotherapy can assist in preparing your body for childbirth and subsequent recovery.
- What type of clothing should I wear to my initial appointment?
Opt for comfortable, loose-fitting attire that allows for easy movement.
Conclusion
Selecting the right pelvic physiotherapy clinic in Toronto is a vital step towards improved women’s health and recovery. Concentrate on finding a qualified, caring, and conveniently located provider who comprehends your individual requirements. With the right assistance, you can heal, avert future complications, and rebuild your confidence in your body.
Pelvic health is an essential but often overlooked component of overall well-being. Whether it’s postpartum recovery, chronic pelvic pain, or bladder dysfunction, pelvic floor issues can have a real impact on quality of life – but too many people suffer in silence. At Triangle Physiotherapy Toronto, our goal is to change that by helping people understand when pelvic physiotherapy is needed, what treatment involves, and how it supports lasting recovery.
What Is Pelvic Physiotherapy?
Pelvic physiotherapy focuses on the muscles, ligaments, and connective tissues in the pelvic region. These structures support organs like the bladder, uterus, and rectum and play a critical role in core strength, posture, continence, and even sexual function.
Dysfunction in these muscles – whether from trauma, overuse, surgery, or childbirth – can result in symptoms such as:
- Pelvic pressure or pain
- Urinary urgency or incontinence
- Constipation or pain during bowel movements
- Painful intercourse
- Lower back or tailbone pain
Many people are surprised to learn how common these symptoms are, or that physiotherapy can help. That’s where early assessment comes in.
Who Needs Pelvic Physiotherapy?
At our Toronto clinic, we work with a wide range of clients – from new moms to high-performance athletes and individuals recovering from surgery or dealing with chronic conditions. Pelvic physiotherapy isn’t just for women or new parents (though both groups benefit greatly); it’s also effective for:
- Men recovering from prostate surgery
- Individuals with persistent lower back or hip pain
- People experiencing unexplained pelvic discomfort
- Athletes with core instability or pelvic floor strain
By normalizing pelvic physiotherapy as a proactive and preventive treatment, we aim to make it more accessible and less intimidating for all.
Our Approach at Triangle Physiotherapy Toronto
1. Comprehensive Assessment
Your journey starts with a detailed clinical assessment, which includes a discussion of symptoms, medical history, lifestyle factors, and, if appropriate, an internal exam to check pelvic floor function. Our environment is respectful and private, ensuring you feel safe throughout.
2. Personalized Treatment Plan
Based on your assessment, we’ll develop a plan tailored to your needs and goals. This may include:
- Manual therapy to release muscle tension
- Neuromuscular retraining
- Breathing and core coordination exercises
- Postural and movement education
- Home exercises to support ongoing care
- Pessary fitting
3. Timelines and Expectations
Treatment timelines vary depending on the issue. Some clients feel better in just a few sessions, while others benefit from ongoing care over several weeks. Your therapist will guide you through realistic expectations and check-ins along the way.
Why Choose Triangle Physiotherapy Toronto?

Pelvic health is deeply personal, and our clinicians are trained to provide expert, empathetic care. At Triangle Physiotherapy Toronto, we combine clinical insight with a supportive approach – educating clients while empowering them to take charge of their healing.
We also offer flexible appointments, direct billing, and convenient booking options for busy Toronto lifestyles.
If you’re dealing with discomfort or simply want to take a proactive step toward better pelvic health, book a consultation today.
Let’s work together to restore comfort, strength, and confidence.
Because healing doesn’t end after delivery
Bringing a new life into the world is no small feat – and neither is the recovery that follows. While many focus on the baby’s well-being (rightfully so!), new moms often put their own healing on the backburner. But those aches, leaks, or feelings of pressure after childbirth? They’re signals that your body needs care too.
At Triangle Physiotherapy North York, we specialize in postpartum pelvic physiotherapy to help you recover in a way that’s safe, informed, and empowering – no matter what kind of birth you had.
What Happens to the Pelvic Floor After Birth?
During pregnancy and delivery, your pelvic floor muscles go through a lot. These muscles support your bladder, uterus, and bowel – and during childbirth, they stretch, strain, and in some cases, tear.
It’s completely normal to feel different after giving birth. But “common” doesn’t mean “should be ignored.”
Signs your pelvic floor needs attention may include:
- Leaking when you laugh, cough, or run
- Pain or discomfort during intimacy
- A heavy or dragging sensation in your pelvis
- Ab separation (diastasis recti)
- Trouble regaining core strength
- Lower back or hip pain
If you’re experiencing any of these, know that postpartum pelvic physiotherapy in North York can help you feel stronger, more comfortable, and more confident in your body again.
How Physiotherapy Helps with Postpartum Recovery

At Triangle Physiotherapy North York, we create personalized recovery plans tailored to your birth experience, current symptoms, and future goals – whether that’s lifting your baby pain-free or getting back to your workout routine.
Here’s how we support your healing:
- Pelvic floor rehab: Gentle techniques to restore muscle tone, function, and coordination
- Core reconditioning: Safe exercises to reconnect with your deep abdominal muscles and rebuild stability
- Breathing & posture work: Learn how daily movements and habits affect your recovery
- Manual therapy: Hands-on treatment for scars, tightness, or alignment issues
- Education: We explain what’s happening in your body, so you feel confident and in control
It’s not about “bouncing back” – it’s about building forward, with guidance and care.
Why Choose Triangle Physiotherapy North York?
Postpartum healing looks different for everyone. Our team understands the physical and emotional aspects of recovery, and we’re here to walk with you every step of the way.
Here’s what you’ll get with us:
- Experienced pelvic health physiotherapists trained in postpartum care
- Private, one-on-one sessions designed around your comfort and pace
- Flexible scheduling including evening and weekend appointments
- Direct billing to most insurance providers
- A focus on realistic, long-term recovery – not pressure to “snap back”
We’re proud to be a trusted provider of postpartum pelvic physiotherapy in North York, helping new moms feel stronger, supported, and empowered.
Ready to Focus on You?
You deserve time to heal, support that understands, and a recovery plan that puts you first. Let’s get you back to feeling like yourself – with a little extra strength for chasing after that new bundle of joy.
Book your postpartum pelvic assessment today at Triangle Physiotherapy North York. We’re here for your recovery, your questions, and your next chapter.
When it comes to women’s health, two conditions often mentioned together are Polycystic Ovary Syndrome (PCOS) and Endometriosis. While both can impact fertility and overall well-being, they are distinct conditions with different causes, symptoms, and treatments. The pelvic health physiotherapists at Triangle Physiotherapy help us break down the key differences to help you better understand them.
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects how the ovaries function. It is one of the most common endocrine disorders among women of reproductive age.
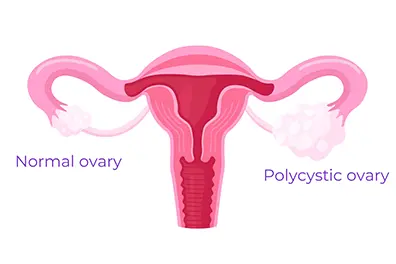
Common Symptoms of PCOS:
- Irregular or Absent Periods: Due to hormonal imbalances, women with PCOS often experience infrequent or prolonged menstrual cycles.
- Excess Hair Growth and Acne: Elevated levels of androgens (male hormones) can lead to hirsutism (excess facial and body hair), acne, and even hair thinning on the scalp.
- Insulin Resistance: Many women with PCOS struggle with insulin resistance, which can increase the risk of type 2 diabetes.
- Ovarian Cysts: Despite its name, not all women with PCOS have cysts on their ovaries, but some may develop multiple small fluid-filled sacs.
What is Endometriosis?
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside of it, leading to inflammation, scarring, and pain.
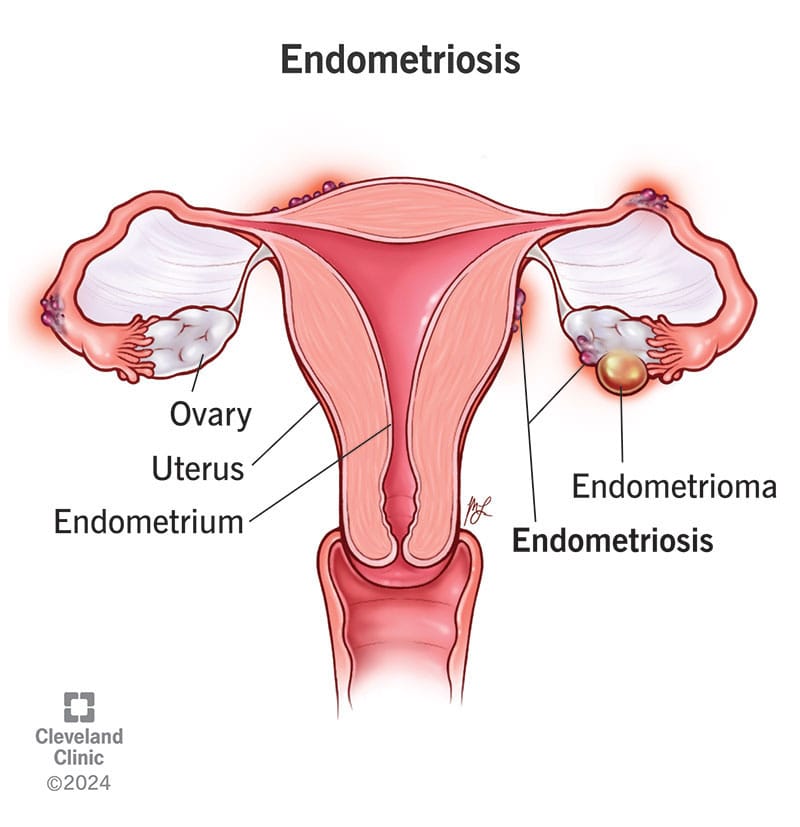
Common Symptoms of Endometriosis:
- Severe Menstrual Cramps: One of the hallmark symptoms of endometriosis is intense pelvic pain that can start before and last beyond the menstrual cycle.
- Heavy Periods: Women with endometriosis often experience unusually heavy menstrual bleeding.
- Pain During Intercourse: Pain during or after sex is a common complaint due to the presence of endometrial-like tissue outside the uterus.
- Chronic Pelvic Pain: Many women with endometriosis experience ongoing pelvic discomfort, even outside their periods.
Key Differences Between PCOS and Endometriosis
| Feature | PCOS | Endometriosis |
|---|---|---|
| Cause | Hormonal imbalance | Endometrial-like tissue growing outside the uterus |
| Periods | Irregular or absent | Heavy and painful |
| Pain | Not always present | Severe pelvic pain |
| Fertility Impact | May cause ovulation issues | May lead to scarring and blockages |
| Hormonal Symptoms | Excess androgens (acne, hair growth) | Usually no androgen-related issues |
How Are PCOS and Endometriosis Treated?
Since these conditions have different causes, their treatments also vary:
- PCOS Treatment: May involve hormonal birth control, lifestyle changes, insulin-sensitizing medications (like Metformin), and fertility treatments if pregnancy is desired.
- Endometriosis Treatment: Can include pain management (NSAIDs), hormonal therapy (such as birth control or GnRH agonists), and in severe cases, surgery to remove endometrial-like tissue.
The Bottom Line
Both PCOS (Polycystic Ovary Syndrome) and Endometriosis are complex conditions that need personalized treatment. If you notice symptoms of either, it’s important to talk to a healthcare provider to get the right diagnosis and treatment plan.
Along with medical care, adding Physiotherapy Oakville can also help. Physiotherapy can ease pelvic pain, improve movement, and reduce muscle tension caused by these conditions. It supports your overall well-being and helps you feel better over time.
By combining medical advice and physiotherapy, you can manage symptoms more effectively and improve your quality of life.
💬 Do you or someone you know struggle with these conditions? Let’s continue raising awareness and supporting women’s health! 💙
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Menopause is a fact of life for people who menstruate – periods need to stop eventually! So why don’t we talk about menopause more often? Even when we do talk about it, there seem to be a lot of misconceptions and myths. It’s time to bust them wide open!
1. Menopause symptoms are mostly hot flashes and mood swings
Though it may be true that hot flashes and mood swings are common symptoms of menopause, it is so much more than that! In fact, comprehensive lists of menopausal symptoms have over 100 different symptoms! Our naturopathic doctor and pelvic health physiotherapists at Triangle Physiotherapy can help educate you on the symptoms and their natural management.
2. Menopausal symptoms are unpreventable and a fact of life for all women

Some women have their periods stop without experiencing any symptoms at all! But even if you’re not one of those lucky people, there are things you can do to help this transitional time in your life to be more manageable. Talk to your naturopathic doctor to find out what you can do!
3. During peri-menopause, your periods always get lighter and farther apart
Though this may be true that eventually your periods become lighter and farther apart, it often doesn’t start that way. Many women find that when menopause begins, it’s actually the exact opposite of this. Periods can become more frequent and heavier before they eventually peter out.
4. The only mood changes that happen during menopause are irritability and mood swings
This is one of the most important myths for us to clarify. Yes, it’s true that irritability, anger, and mood swings are all potential symptoms of menopause. But anxiety and depression are part of what can happen during menopause, too. Instead of thinking of a menopausal woman as “cranky and short-tempered”, keep in mind that they may be going through anxiety and depression. Check up on menopausal women, and ensure they have the mental health support they often need at this time.
5. Menopause only happens after age 50
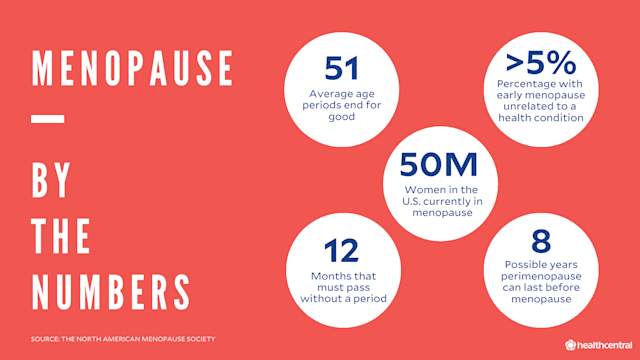
The most common age for menopause to happen is 50, but there is a lot of variance with this. In fact, some women can even go into menopause in their 30’s!
6. A hysterectomy always causes menopause
If you have a total hysterectomy, it is true that you will enter menopause post-surgery. But if your ovaries are not removed, then this isn’t the case. You would go through menopause naturally, and this could happen many years after your hysterectomy.
7. An IUD can cause you to skip over menopause
IUD’s have no impact on when you will go through menopause. What they can do, however, is help to manage some of the bleeding symptoms that can occur along with menopause.
8. Menopause marks the end of a woman’s sex life
Absolutely not! Women can have healthy sex lives well beyond menopause! Some symptoms of declining estrogen levels, such as lower libido and vaginal dryness, may make intercourse more difficult. However, there are natural options that can help to manage these symptoms to make intercourse more pleasurable for you. Be sure to speak to a naturopathic doctor if you would like to explore more of these options. Our pelvic health physiotherapists can also help you navigate the effects menopause can have on your sex life.
9. Menopause lasts a couple of years
It’s usually much longer than this. In fact, menopausal symptoms can begin up to 10 years before your periods actually stop!
10. Men go through menopause too
Nope. You may have heard of “andropause” or “manopause”, which refer to when testosterone levels decline in men. However, this testosterone decline happens very slowly, over several years. In menopause, the hormonal fluctuations are more drastic and happen much more quickly. This is why menopause can cause uncomfortable symptoms.
We hope this helped to clear up some of the common myths out there about menopause. If you have any further questions about menopause or women’s health, reach out to our naturopathic doctor at Triangle Physiotherapy and book an appointment today!