Breastfeeding can be a fulfilling and bonding experience, but it sometimes comes with challenges such as mastitis and blocked milk ducts. These conditions can be painful and stressful for new mothers, but understanding and managing them can significantly improve your breastfeeding journey. In this blog, we’ll explore what mastitis and blocked milk ducts are, their symptoms, causes, and how physiotherapy, particularly in the pelvic health domain, can help. This information is especially valuable for mothers in North York looking for local resources and support.
What is Mastitis?
Mastitis is an inflammation of breast tissue that often involves an infection. This condition can cause breast pain, swelling, warmth, and redness. In some cases, mothers might experience fever and chills. It typically occurs in breastfeeding women when milk ducts become blocked or when bacteria enter the breast through a cracked nipple.

Symptoms of Mastitis
Common symptoms of mastitis include:
- Breast pain or tenderness
- Swelling and warmth in the affected area
- Redness, often in a wedge-shaped pattern
- Fever and chills
- Fatigue
Causes of Mastitis
Mastitis is often caused by:
- Blocked milk ducts: When milk isn’t fully drained from the breast, it can cause a blockage, leading to inflammation.
- Bacterial infection: Bacteria from the baby’s mouth or the mother’s skin can enter the breast through a cracked nipple.
Understanding Blocked Milk Ducts
Blocked milk ducts are a common issue for breastfeeding mothers. When a duct is blocked, it prevents the milk from flowing freely through the breast, leading to a backup of milk and potential inflammation.
Symptoms of Blocked Milk Ducts
- A small, hard lump in the breast that may be tender to the touch
- Discomfort or pain in one area of the breast
- A decrease in milk supply from the affected breast
- Milk blebs or blisters on the nipple
Causes of Blocked Milk Ducts
- Infrequent breastfeeding or pumping
- Poor latch or ineffective sucking by the baby
- Pressure on the breast from tight clothing or a poorly fitting bra
- Stress and fatigue
How Physiotherapy Can Help
Physiotherapy can be an effective treatment for mastitis and blocked milk ducts. Specialized techniques used by physiotherapists in the pelvic health domain can alleviate symptoms and prevent recurrence. Here are some ways physiotherapy can help:
Therapeutic Ultrasound
Therapeutic ultrasound is a non-invasive treatment that uses sound waves to reduce inflammation and pain. It can help to clear blocked ducts and promote milk flow.
Breast Massage Techniques
Our Physiotherapists in North York can teach you proper breast massage techniques to relieve blocked ducts. This includes:
- Gentle circular motions around the lump
- Moving the lump towards the nipple
- Massage before and during breastfeeding to aid milk flow
Education and Support
Our Physiotherapists in North York provide education on proper breastfeeding techniques, ensuring a good latch and advising on optimal breastfeeding positions. They also offer support and strategies to manage stress and fatigue, which are crucial for overall well-being.
Local Resources in North York
For mothers in North York, Triangle Physiotherapy North York specializes in pelvic health and offers targeted treatments for breastfeeding-related issues. Our clinic provides a supportive environment where mothers can receive personalized care and practical advice.
Prevention Tips
Preventing mastitis and blocked milk ducts involves:
- Frequent breastfeeding or pumping to keep the milk flowing
- Ensuring the baby has a good latch
- Varying breastfeeding positions
- Wearing loose-fitting, comfortable bras
- Staying hydrated and maintaining a balanced diet
Mastitis and blocked milk ducts can be challenging, but with the right understanding and support, they are manageable. Physiotherapy offers effective treatments and strategies to help mothers overcome these issues and continue their breastfeeding journey with confidence. If you’re in North York and experiencing breastfeeding challenges, consider reaching out to a local pelvic health physiotherapist for specialized care.
For more information or to book an appointment, contact our clinic today and take the first step towards a pain-free breastfeeding experience.
“For those dealing with mastitis or blocked milk ducts, Triangle Physiotherapy provides expert care across various locations including Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village.”
Managing mastitis and blocked milk ducts can be challenging, but with the right care, recovery is possible. For comprehensive support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas can help you manage symptoms effectively and promote healing.
Vaginal atrophy, also known as atrophic vaginitis, is a condition that many women experience, especially after menopause. It involves changes in the vaginal area that can cause discomfort and other symptoms. Fortunately, our pelvic health physiotherapists in North York can help manage these symptoms and improve your quality of life.
What is Vaginal Atrophy?
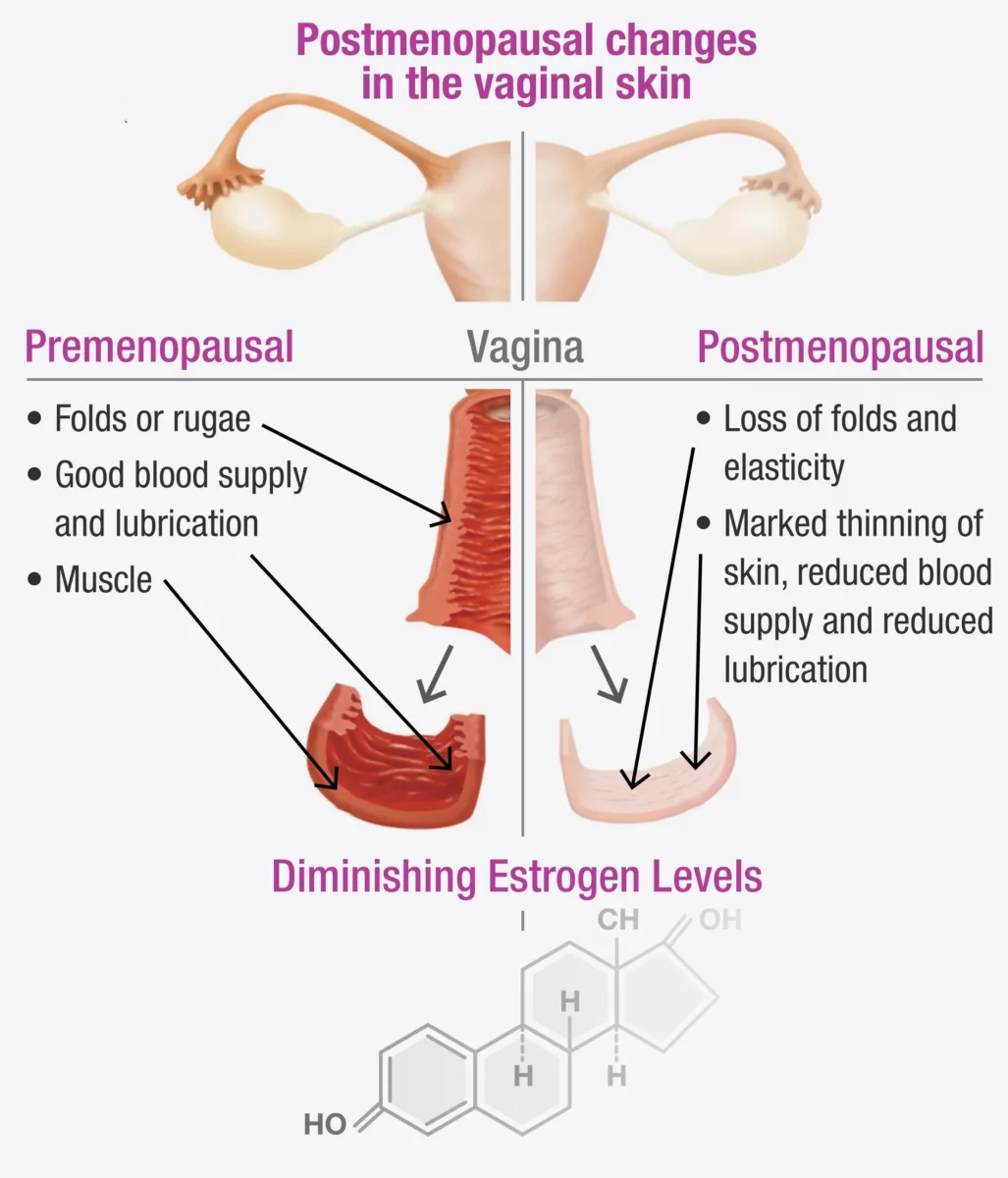
Vaginal atrophy often happens during menopause when the levels of estrogen, a hormone in a woman’s body, decrease. When this happens, it can lead to:
- Dryness: The vagina becomes less moist, leading to dryness and irritation.
- Thinning of Vaginal Walls: The walls of the vagina become thinner and less flexible.
- Inflammation and Redness: The vaginal area can become inflamed and red, causing pain.
- Urinary Symptoms: You might experience more frequent urination, a strong urge to urinate, or urinary tract infections (UTIs).
These changes can make everyday activities uncomfortable and affect your sex life.
If vaginal atrophy is not treated and a woman continues to experience painful intercourse, the vaginal muscles may react by tightening to protect the body. Over time, this tightening can become an automatic response (vaginismus) that continues even after the atrophy has been treated.
Fortunately, both conditions can be treated with the help of a pelvic health Physiotherapist in North York. In fact, it is often necessary to treat vaginal atrophy and vaginismus together, as addressing one without the other can be challenging.
Symptoms to Watch For
You might have vaginal atrophy if you notice:
- Pain During Sex: Painful intercourse (called dyspareunia) is a common symptom.
- Itching or Burning: These sensations can be uncomfortable and persistent.
- Frequent UTIs: More urinary tract infections than usual.
- Vaginal Bleeding or Discharge: Unusual bleeding or discharge can occur.
- Difficulty Urinating: Problems with urination, such as a strong urge or pain.
Recognizing these symptoms early can help you get the treatment you need sooner.
How a Pelvic Health Physiotherapist Can Help with Menopause and Vaginal Atrophy
A pelvic health physiotherapist is a specialist who focuses on the muscles and tissues in the pelvic area. They can provide various treatments to help manage vaginal atrophy. Here’s how they can assist:
1. Assessment and Diagnosis
The first step is a thorough check-up, which includes:
- Reviewing Your Medical History: Discussing your symptoms, medical history, and any medications you are taking.
- Physical Examination: Checking the condition of your vaginal walls, pelvic floor muscles, and surrounding tissues.
2. Customized Exercise Programs
These physiotherapists create specific exercise programs to strengthen and relax your pelvic floor muscles. These exercises can:
- Improve Muscle Tone: Making the vaginal muscles stronger and more flexible.
- Boost Blood Flow: Increasing circulation to help with healing and tissue health.
3. Manual Therapy and Techniques
Hands-on techniques are used to improve the flexibility and function of your pelvic area, such as:
- Myofascial Release: Reducing tension in the pelvic muscles.
- Scar Tissue Mobilization: Addressing any scarring or adhesions in the vaginal area.
4. Education and Lifestyle Advice for Menopause
Education is a key part of therapy, including advice on:
- Diet and Hydration: Eating a balanced diet and staying hydrated for overall health.
- Relaxation Techniques: Learning how to relax your pelvic floor muscles to reduce discomfort.
5. Use of Devices and Modalities
They might suggest using certain devices and techniques, such as:
- Vaginal Dilators: These help gently stretch the vaginal walls, making them more flexible.
- Electrostimulation: Using mild electrical impulses to strengthen pelvic muscles.
How do I find a pelvic health physiotherapist in North York?
We have 8 locations with pelvic health physiotherapists to help you. If you are going through menopause and are seeing signs of vaginal atrophy, Book an Appointment today!
Pelvic Health Physiotherapists in North York:
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
At Triangle Physiotherapy, we understand that conditions like menopause and vaginal atrophy can significantly impact your quality of life. Our team of experienced professionals is here to help you through specialized physiotherapy treatments designed to address these and other related concerns. Whether you’re seeking Physiotherapy in Etobicoke, Physiotherapy in Oakville, Physiotherapy in North York, or Physiotherapy in Toronto, we have clinics conveniently located across the region. Visit us at Physiotherapy Lawrence Park, Physiotherapy Clinic Queens Quay, Physiotherapy Erin Mills, Physiotherapy Mississauga, or Physiotherapy Liberty Village to start your journey towards better health and well-being.
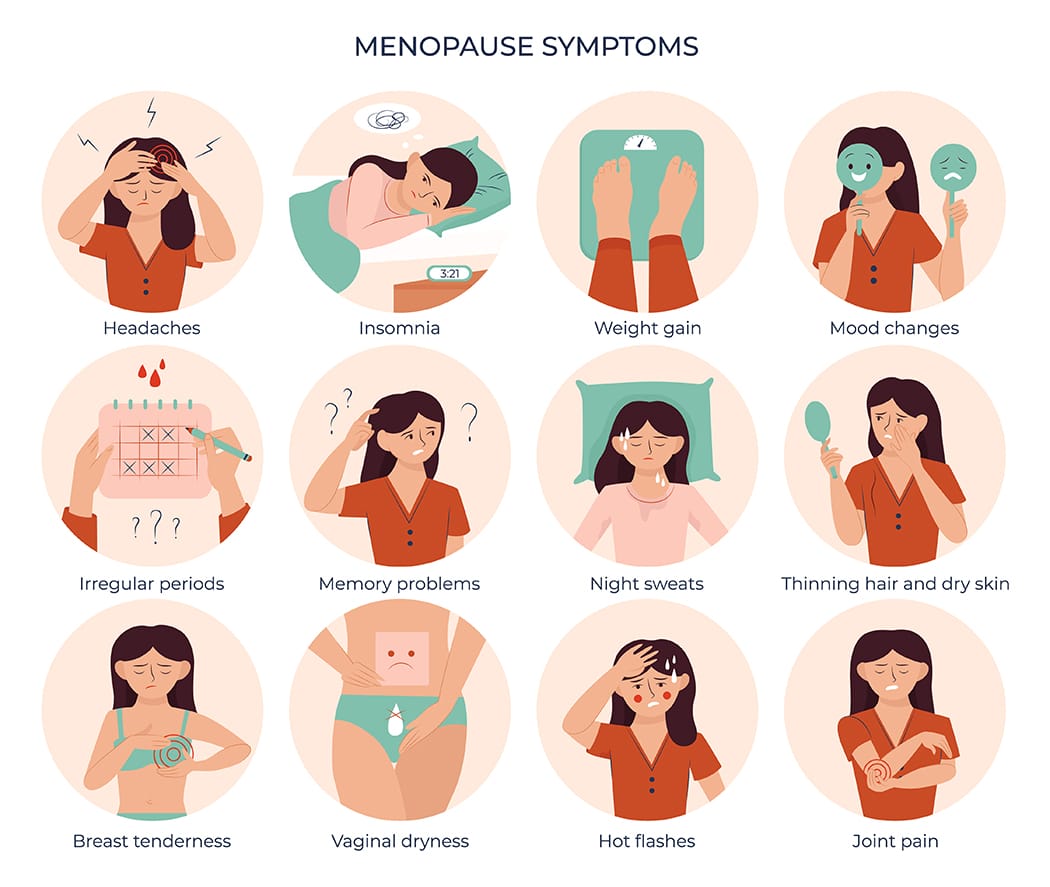
Menopause can be a very overwhelming time for a lot of women. During this period, there are a lot of hormonal changes that can influence the way you feel in your body. Menopause tends to start between the ages of 45 to 55. This can include a range of symptoms such as hot flashes and mood swings to vaginal dryness and changes in pelvic health.

How does Menopause affect pelvic health?
Many women don’t realize that menopause can affect pelvic health. As estrogen levels decline, tissues in the vagina, urethra, and bladder can become thinner, drier, and less elastic, leading to a condition called vaginal atrophy. This can cause uncomfortable symptoms such as vaginal dryness, itching, burning, and pain during sex. In addition, menopause can also increase the risk of pelvic floor disorders, such as incontinence and prolapse. But don’t worry, many of these conditions can be improved through pelvic physiotherapy!
What is pelvic floor physiotherapy?
Pelvic floor physiotherapy is a specialized form of physiotherapy that focuses on the pelvic floor muscles, which support the pelvic organs (bladder, uterus, and rectum) and control bladder and bowel function. Pelvic physiotherapy can help to improve pelvic health during menopause and beyond, providing relief from uncomfortable symptoms and reducing the risk of pelvic floor disorders.
What does Pelvic Health Physiotherapy Involve?
Pelvic floor physiotherapy involves a range of techniques designed to improve the strength, coordination, and function of the pelvic floor muscles. These techniques may include pelvic floor exercises, biofeedback, electrical stimulation, manual therapy, and education on lifestyle modifications. It is an effective alternative to drug based therapy and surgery, and allows for you to take your health into your own hands.
How Can Pelvic Physiotherapy Help During Menopause?
- Pelvic physiotherapy can help to address a range of pelvic health issues that can arise during menopause, including:
- Vaginal Dryness: Pelvic physiotherapy can help to improve blood flow to the vaginal area, which can increase lubrication and reduce discomfort during intercourse. Additionally, exercises to strengthen the pelvic floor muscles can help to improve vaginal tone and elasticity.
- Urinary Incontinence: Pelvic physiotherapy can help to strengthen the pelvic floor muscles that support the bladder, which can improve bladder control and reduce urinary incontinence.
- Prolapse: Pelvic physiotherapy can help with prolapse symptoms or post-hysterectomy. With a prolapse, there is commonly increased muscle tone causing the organ to descend. This can be improved with exercise and treatment. Post hysterectomy, there can be pelvic floor weakness or altered sensation internally which can also be treated through strengthening and sensitization work.
- Painful Intercourse: Pelvic physiotherapy can help to improve vaginal tone and elasticity, which can reduce pain and discomfort during intercourse.
How can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“While menopause symptoms can be challenging, they are not inevitable for everyone and can be managed with the right care. Triangle Physiotherapy offers specialized services to help you navigate this stage of life across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can provide personalized treatment plans to alleviate symptoms and improve your quality of life.”




