Understanding the Pelvic Floor and Bladder Health
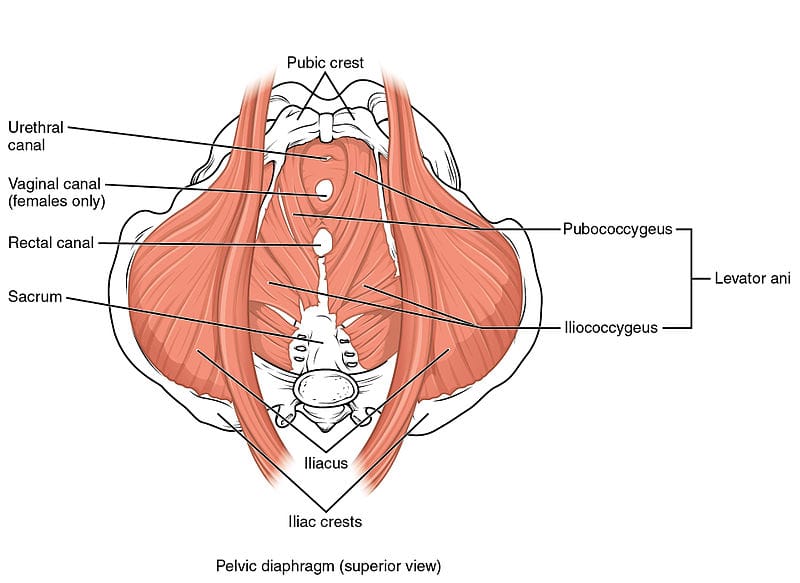
The pelvic floor consists of a group of muscles that support the bladder, bowel, and uterus (in women). These muscles are responsible for controlling urination, bowel movements, and sexual function. When weakened, common issues such as incontinence, pelvic organ prolapse, and sexual dysfunction can arise. Understanding the role of these muscles is the first step toward strengthening them.
Strengthening you pelvic floor can lead to a stress-free lifestyle. Schedule an appointment with one of the pelvic health physiotherapists at Triangle Physiotherapy.
Key functions of the Pelvic Floor:
- Support of pelvic organs
- Control of bladder and bowel movements
- Sexual health and satisfaction
Benefits of Strengthening the Pelvic Floor
By keeping your pelvic floor muscles strong, you can experience several benefits beyond preventing common issues like incontinence. Some of these include:
- Enhanced bladder control: Strong muscles prevent leakage during activities like sneezing, laughing, or exercising.
- Better posture: The pelvic floor is connected to core muscles, and strengthening it can improve your overall posture.
- Improved sexual function: Strengthening the pelvic muscles can lead to better sexual sensations and enhanced satisfaction.
- Postpartum recovery: New mothers can benefit from a stronger pelvic floor to regain muscle strength after childbirth.
Lifestyle Changes for Pelvic Health

Incorporating small but impactful changes in your daily routine can go a long way in improving pelvic floor and bladder health. Here are a few simple yet effective lifestyle adjustments:
- Stay hydrated but mindful of fluids: Drink plenty of water throughout the day, but reduce intake of caffeinated or carbonated drinks that can irritate the bladder.
- Maintain a healthy weight: Excess weight puts pressure on the pelvic floor, weakening it over time. Maintaining a healthy BMI can reduce strain.
- Eat a fiber-rich diet: Consuming enough fiber prevents constipation, which can stress the pelvic floor.
- Quit smoking: Chronic coughing caused by smoking weakens the pelvic floor muscles over time.
Strengthening your pelvic floor and bladder is a journey that requires consistency and dedication. By incorporating simple exercises, making mindful lifestyle changes, and considering professional or holistic support, you can enjoy better control, confidence, and overall well-being. Remember, prevention is always better than cure, so taking steps to support your pelvic health now will benefit you in the long run.
This lifestyle guide offers a comprehensive approach to strengthening your pelvic floor and bladder. By following these tips and making small adjustments, you’ll be well on your way to a healthier and stronger pelvic floor.
Contact us today to book an appointment with one of our pelvic health physiotherapists at either of our 8 locations and get your recovery journey started.
Vaginal atrophy, also known as atrophic vaginitis, is a condition that many women experience, especially after menopause. It involves changes in the vaginal area that can cause discomfort and other symptoms. Fortunately, our pelvic health physiotherapists in North York can help manage these symptoms and improve your quality of life.
What is Vaginal Atrophy?
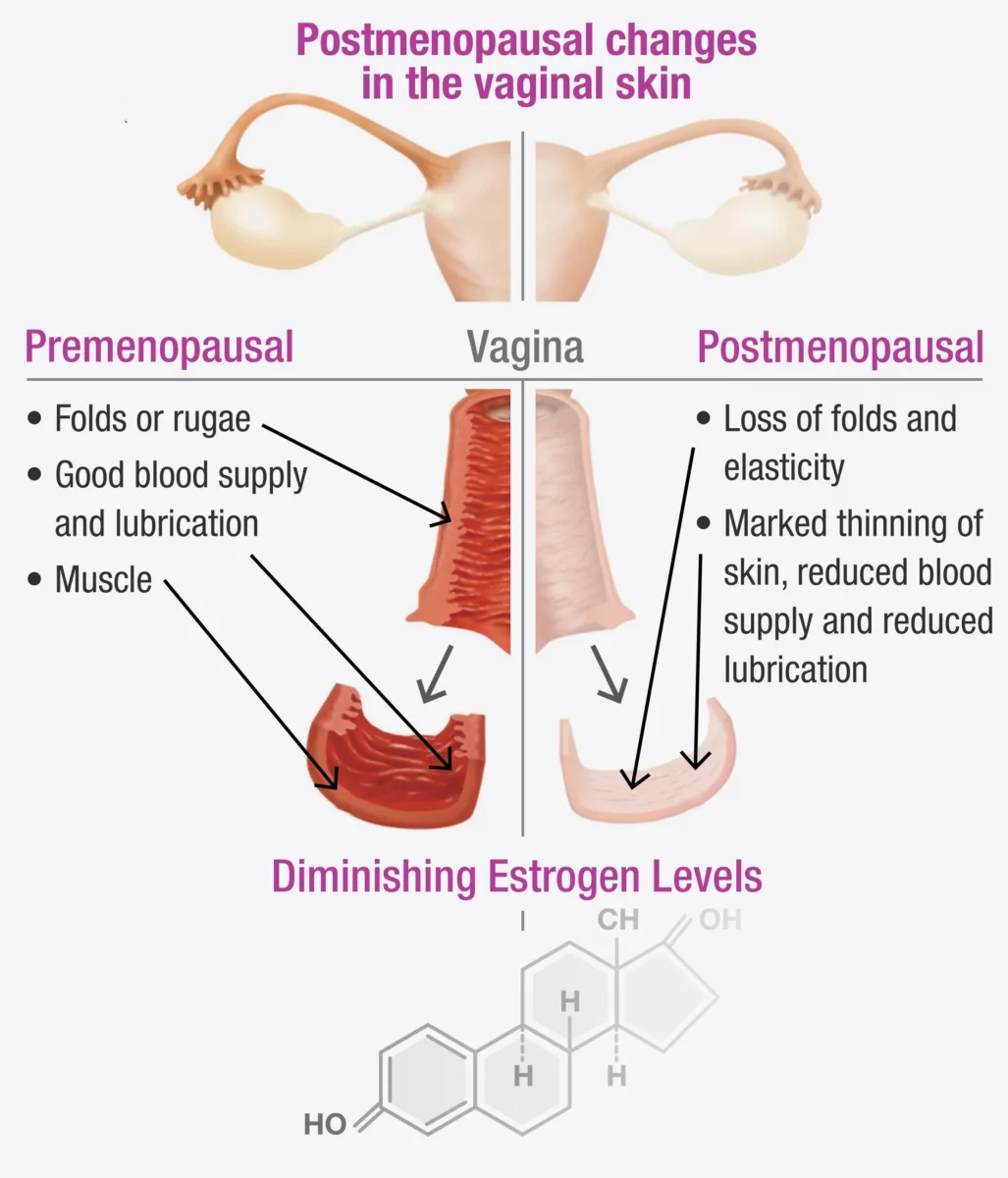
Vaginal atrophy often happens during menopause when the levels of estrogen, a hormone in a woman’s body, decrease. When this happens, it can lead to:
- Dryness: The vagina becomes less moist, leading to dryness and irritation.
- Thinning of Vaginal Walls: The walls of the vagina become thinner and less flexible.
- Inflammation and Redness: The vaginal area can become inflamed and red, causing pain.
- Urinary Symptoms: You might experience more frequent urination, a strong urge to urinate, or urinary tract infections (UTIs).
These changes can make everyday activities uncomfortable and affect your sex life.
If vaginal atrophy is not treated and a woman continues to experience painful intercourse, the vaginal muscles may react by tightening to protect the body. Over time, this tightening can become an automatic response (vaginismus) that continues even after the atrophy has been treated.
Fortunately, both conditions can be treated with the help of a pelvic health Physiotherapist in North York. In fact, it is often necessary to treat vaginal atrophy and vaginismus together, as addressing one without the other can be challenging.
Symptoms to Watch For
You might have vaginal atrophy if you notice:
- Pain During Sex: Painful intercourse (called dyspareunia) is a common symptom.
- Itching or Burning: These sensations can be uncomfortable and persistent.
- Frequent UTIs: More urinary tract infections than usual.
- Vaginal Bleeding or Discharge: Unusual bleeding or discharge can occur.
- Difficulty Urinating: Problems with urination, such as a strong urge or pain.
Recognizing these symptoms early can help you get the treatment you need sooner.
How a Pelvic Health Physiotherapist Can Help with Menopause and Vaginal Atrophy
A pelvic health physiotherapist is a specialist who focuses on the muscles and tissues in the pelvic area. They can provide various treatments to help manage vaginal atrophy. Here’s how they can assist:
1. Assessment and Diagnosis
The first step is a thorough check-up, which includes:
- Reviewing Your Medical History: Discussing your symptoms, medical history, and any medications you are taking.
- Physical Examination: Checking the condition of your vaginal walls, pelvic floor muscles, and surrounding tissues.
2. Customized Exercise Programs
These physiotherapists create specific exercise programs to strengthen and relax your pelvic floor muscles. These exercises can:
- Improve Muscle Tone: Making the vaginal muscles stronger and more flexible.
- Boost Blood Flow: Increasing circulation to help with healing and tissue health.
3. Manual Therapy and Techniques
Hands-on techniques are used to improve the flexibility and function of your pelvic area, such as:
- Myofascial Release: Reducing tension in the pelvic muscles.
- Scar Tissue Mobilization: Addressing any scarring or adhesions in the vaginal area.
4. Education and Lifestyle Advice for Menopause
Education is a key part of therapy, including advice on:
- Diet and Hydration: Eating a balanced diet and staying hydrated for overall health.
- Relaxation Techniques: Learning how to relax your pelvic floor muscles to reduce discomfort.
5. Use of Devices and Modalities
They might suggest using certain devices and techniques, such as:
- Vaginal Dilators: These help gently stretch the vaginal walls, making them more flexible.
- Electrostimulation: Using mild electrical impulses to strengthen pelvic muscles.
How do I find a pelvic health physiotherapist in North York?
We have 8 locations with pelvic health physiotherapists to help you. If you are going through menopause and are seeing signs of vaginal atrophy, Book an Appointment today!
Pelvic Health Physiotherapists in North York:
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
At Triangle Physiotherapy, we understand that conditions like menopause and vaginal atrophy can significantly impact your quality of life. Our team of experienced professionals is here to help you through specialized physiotherapy treatments designed to address these and other related concerns. Whether you’re seeking Physiotherapy in Etobicoke, Physiotherapy in Oakville, Physiotherapy in North York, or Physiotherapy in Toronto, we have clinics conveniently located across the region. Visit us at Physiotherapy Lawrence Park, Physiotherapy Clinic Queens Quay, Physiotherapy Erin Mills, Physiotherapy Mississauga, or Physiotherapy Liberty Village to start your journey towards better health and well-being.
March 8th marks International Women’s Day and Triangle Physiotherapy is proud to be able to empower women to advocate for themselves and their health needs.
Our goal is to encourage women to focus on their health, both, physical and mental. Build your healthcare team and schedule regular visits, in addition to exercising regularly and eating healthy.
Women’s Health and the Pelvic Floor
Women’s health is intricately connected to the well-being of the pelvic floor, a group of muscles, ligaments, and tissues supporting the uterus, bladder, and rectum. Maintaining a healthy pelvic floor is crucial for various functions, including urinary and bowel control, sexual function, and providing support during pregnancy. Pregnancy, childbirth, hormonal changes, and aging can impact the pelvic floor, leading to issues like incontinence, pelvic organ prolapse, and sexual dysfunction.
Maintaining a healthy lifestyle, proper posture, and seeking guidance from a pelvic health physiotherapist are essential for women’s pelvic floor health. Awareness and proactive care contribute to overall well-being, enabling women to lead active and fulfilling lives while addressing potential pelvic floor challenges.
What are the symptoms of Pelvic Floor Dysfunction?
Pelvic Floor Dysfunction (PFD) can manifest through various symptoms, which may vary in intensity and duration. Common signs of PFD include:
- Urinary Issues:
- Urinary incontinence: Involuntary leakage of urine.
- Frequent urination: The need to urinate more often than usual.
- Difficulty emptying the bladder: Struggling to fully release urine.
- Bowel Issues:
- Constipation: Difficulty passing stools or infrequent bowel movements.
- Straining during bowel movements: Experiencing difficulty while trying to have a bowel movement.
- Pelvic Pain:
- Pelvic pain or discomfort: Discomfort in the pelvic region, which may be persistent or intermittent.
- Pain during sexual intercourse: Discomfort or pain during sexual activity.
- Muscle Tension:
- Tight or spasming pelvic muscles: Increased muscle tension in the pelvic floor.
- Pelvic Organ Prolapse:
- The feeling of pressure or fullness in the pelvic area: Sensation of something bulging or descending into the vagina.
- Lower Back Pain:
- Chronic lower back pain: Discomfort or pain in the lower back region.
- Changes in Posture:
- Altered posture: Changes in the alignment of the spine and pelvis.
How a Pelvic Health Physiotherapist can help and what to expect?
A Pelvic Health Physiotherapist specializes in assessing and treating conditions related to the pelvic floor and surrounding areas. Here’s how they can help and what to expect during a session:
- Assessment:
- A thorough assessment of your medical history, pelvic health, and relevant symptoms.
- Physical examination, which may include internal and external assessments to evaluate the strength, flexibility, and coordination of the pelvic floor muscles.
- Education:
- Detailed explanation of pelvic anatomy and the role of pelvic floor muscles in various functions.
- Guidance on lifestyle factors, posture, and habits that may contribute to pelvic health issues.
- Pelvic Floor Exercises:
- Prescribing personalized pelvic floor exercises, to strengthen or relax specific muscles based on the assessment findings.
- Teaching proper technique and ensuring exercises are performed correctly.
- Manual Therapy:
- Hands-on techniques to release tension in the pelvic floor muscles or surrounding tissues.
- Myofascial release and trigger point therapy to address muscle knots or tightness.
- Biofeedback:
- Using biofeedback tools to provide real-time information about pelvic floor muscle activity.
- Assisting individuals in learning how to control and coordinate their pelvic floor muscles.
- Behavioral Strategies:
- Implementing behavioral strategies for managing and improving bladder and bowel function.
- Developing strategies for optimizing pelvic health during daily activities.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
On International Women’s Day, let’s celebrate the strength and resilience of women everywhere. For those seeking expert support for their health and wellness, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas are committed to empowering women through personalized care and treatment plans.
Pelvic Health physiotherapists advocate the importance of educating individuals about their pelvic health. They are often asked by patients if an internal exam is necessary. Many patients refrain from seeking help for pelvic health issues because of the fear of internal examination. While internal exams are not a must, they can be very helpful to pelvic health physiotherapists in determining the condition of the pelvic floor.
What is an Internal Pelvic Exam?
A pelvic floor assessment, which may or may not include an internal pelvic exam, entails a pelvic health physiotherapist examining the pelvic floor muscles, tissues, and organs by inserting a gloved hand into the vagina or rectum. This examination is crucial for assessing the well-being and performance of the pelvic floor, allowing for the detection of any possible problems or issues.
Why is an internal pelvic exam important?
- Detailed Assessment of Pelvic Floor Muscles: An internal pelvic exam allows the physiotherapist to assess the tone, strength, flexibility, and coordination of the pelvic floor muscles. This information is crucial in developing an accurate understanding of the patient’s pelvic health.
- Identification of Muscle Imbalances: Through internal palpation, a physiotherapist can identify any muscle imbalances or asymmetries in the pelvic floor. This helps in tailoring the treatment plan to address specific issues, such as hypertonic (overactive) or hypotonic (underactive) muscles.
- Assessment of Pelvic Organ Function: Internal examination enables the physiotherapist to assess the function of pelvic organs, such as the bladder, uterus, and rectum. This is important in cases where dysfunction or weakness in the pelvic floor muscles may be contributing to issues such as urinary incontinence or pelvic organ prolapse.
- Evaluation of Connective Tissues and Nerves: The internal exam allows the physiotherapist to assess the condition of connective tissues, ligaments, and nerves in the pelvic region. Dysfunction in these structures can contribute to pelvic pain and other symptoms, and the internal exam helps in identifying such issues.
- Assessment of Trigger Points and Tenderness: The physiotherapist can identify trigger points and areas of tenderness within the pelvic floor muscles. This information is crucial in designing a targeted treatment plan, which may include manual therapy techniques to release muscle tension.
- Feedback on Exercise Performance: During an internal pelvic exam, the physiotherapist may guide the patient through specific exercises to assess the effectiveness of pelvic floor muscle contractions. Real-time feedback helps the patient learn proper muscle engagement and control.
- Patient Education and Empowerment: The internal exam provides an opportunity for the physiotherapist to educate the patient about their pelvic floor anatomy, function, and any specific issues identified during the assessment. This empowers the patient to actively participate in their treatment plan and make lifestyle changes that support pelvic health.

Do I have to have an internal exam during a pelvic health assessment?
It’s important to note that internal pelvic exams are conducted with the patient’s informed consent, and physiotherapists ensure a comfortable and respectful environment during the assessment. The goal is to provide comprehensive care and address the specific needs of individuals experiencing pelvic health issues. That being said, if you are not comfortable being internally examined, please let your physiotherapist know before the start of your assessment.
How do I prepare for an internal pelvic exam?
Preparing for an internal pelvic exam involves a combination of physical and mental preparation. It’s essential to communicate openly with your pelvic health physiotherapist and follow their instructions. Here are some general guidelines to help you prepare:
Comfortable Clothing: Wear comfortable, easy-to-remove clothing. You may be asked to undress from the waist down, so wearing a skirt or loose pants can be convenient.
Relaxation Techniques: Practice relaxation techniques such as deep breathing to help ease anxiety and tension. Relaxing your pelvic muscles can make the exam more comfortable.
Communicate with your Physiotherapist: Inform your pelvic health physiotherapist about any concerns, fears, or past traumatic experiences related to pelvic exams. They can adjust their approach and provide additional support.
Ask Questions: Feel free to ask any questions you may have about the procedure. Knowing what to expect can help alleviate anxiety.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Understanding the need for an internal exam during a pelvic health assessment can help you make informed decisions about your care. If you’re looking for specialized support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can provide comprehensive pelvic health assessments tailored to your comfort and needs.
Triangle Physiotherapy in Mississauga is a full-service clinic that offers specialized services like Pelvic Health Physiotherapy. Our pelvic health physiotherapists are trained professionals who, apart from being experts in their field, are also empathetic individuals who understand the sensitive nature of the conditions that make people seek pelvic health physiotherapy.
Tell me more about your Mississauga Pelvic Health physiotherapists.

Our Mississauga Pelvic Health physiotherapists have training in the field of pelvic health physiotherapy and are committed to providing the best care to the community in Mississauga, be it new moms, women with prolapse or incontinence issues, pessary fittings, labour and delivery support, and more. We also have a pelvic health physiotherapist who is trained to help children. Our pelvic health physiotherapists are also able to help men with their pelvic health issues.
What type of conditions can a pelvic floor physiotherapist treat?
Some of the conditions treated by our Mississauga Pelvic Health physiotherapists are:
- Incontinence (urinary and fecal)
- Pelvic organ prolapse and pessary fittings
- Constipation
- Diastasis recti
- Vaginismus
- Pelvic pain
- Pelvic girdle pain during pregnancy and postpartum)
- Coccydynia (tailbone pain)
- Pudendal neuralgia
- Interstitial cystitis
- Female and Male Sexual dysfunction
- Prostatitis
- Rectal pain and dysfunction
- Irritable bowel syndrome
- Anal incontinence
- Anal fissures and fistulas
- Anal neuralgia
- Rectal prolapse
I just gave birth recently. How soon should I see a pelvic health physiotherapist
The pelvic floor muscles may get stretched or damaged during delivery, whether by C-Section or vaginal. This may cause issues of the pelvic floor that manifest as urinary or fecal incontinence, urinary urgency or frequency, pain during sexual activity, pelvic organ prolapse, pelvic pain, lower back pain, diastasis recti, or scar pain. Many of these issues can be addresed by pelvic health physiotherapy, however, our pelvic physiotherapists in Mississauga recommend waiting at least six weeks after delivery to allow the body time to heal from childbirth.
Can I speak to a pelvic health physiotherapist in Mississauga prior to booking a consultation?
We can certainly connect you with the best pelvic floor physiotherapist in Mississauga that can answer any questions you may have. Click here to book a discovery call.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Finding the right pelvic health physiotherapist is crucial for effective treatment and recovery. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists specialize in pelvic health, providing personalized treatment plans to help you achieve the best possible outcomes.”
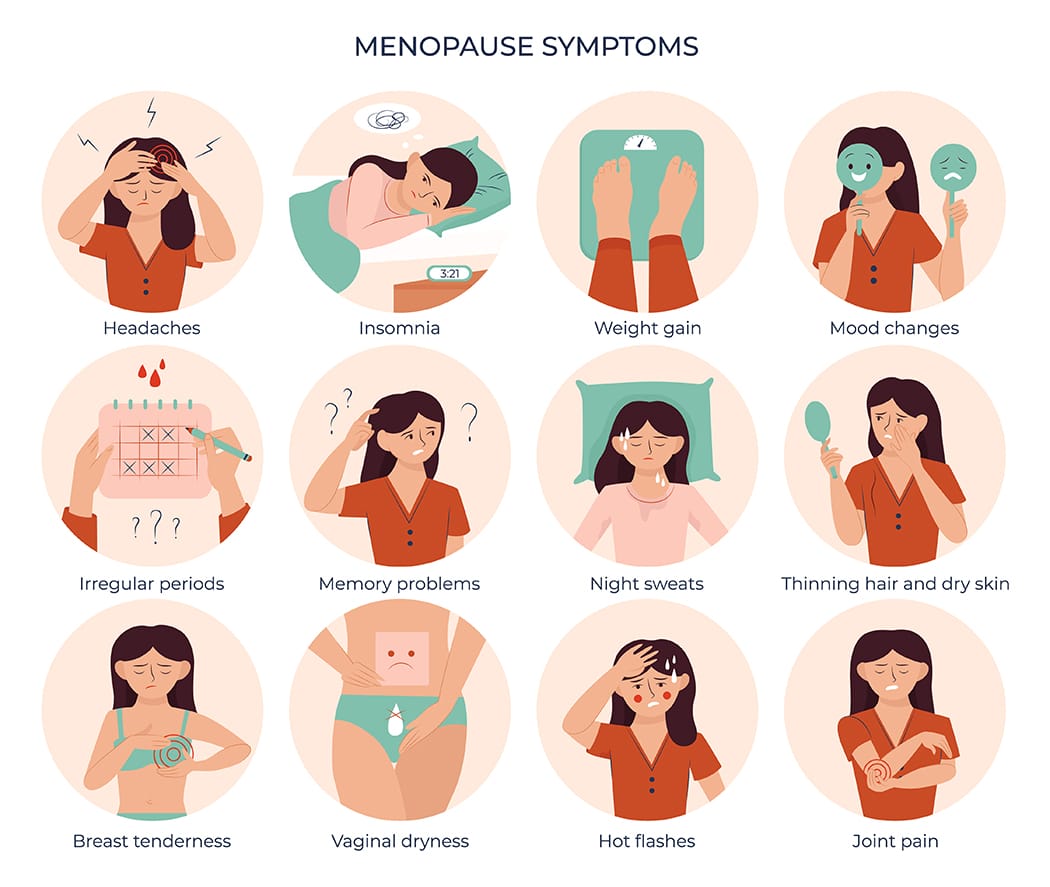
Menopause can be a very overwhelming time for a lot of women. During this period, there are a lot of hormonal changes that can influence the way you feel in your body. Menopause tends to start between the ages of 45 to 55. This can include a range of symptoms such as hot flashes and mood swings to vaginal dryness and changes in pelvic health.

How does Menopause affect pelvic health?
Many women don’t realize that menopause can affect pelvic health. As estrogen levels decline, tissues in the vagina, urethra, and bladder can become thinner, drier, and less elastic, leading to a condition called vaginal atrophy. This can cause uncomfortable symptoms such as vaginal dryness, itching, burning, and pain during sex. In addition, menopause can also increase the risk of pelvic floor disorders, such as incontinence and prolapse. But don’t worry, many of these conditions can be improved through pelvic physiotherapy!
What is pelvic floor physiotherapy?
Pelvic floor physiotherapy is a specialized form of physiotherapy that focuses on the pelvic floor muscles, which support the pelvic organs (bladder, uterus, and rectum) and control bladder and bowel function. Pelvic physiotherapy can help to improve pelvic health during menopause and beyond, providing relief from uncomfortable symptoms and reducing the risk of pelvic floor disorders.
What does Pelvic Health Physiotherapy Involve?
Pelvic floor physiotherapy involves a range of techniques designed to improve the strength, coordination, and function of the pelvic floor muscles. These techniques may include pelvic floor exercises, biofeedback, electrical stimulation, manual therapy, and education on lifestyle modifications. It is an effective alternative to drug based therapy and surgery, and allows for you to take your health into your own hands.
How Can Pelvic Physiotherapy Help During Menopause?
- Pelvic physiotherapy can help to address a range of pelvic health issues that can arise during menopause, including:
- Vaginal Dryness: Pelvic physiotherapy can help to improve blood flow to the vaginal area, which can increase lubrication and reduce discomfort during intercourse. Additionally, exercises to strengthen the pelvic floor muscles can help to improve vaginal tone and elasticity.
- Urinary Incontinence: Pelvic physiotherapy can help to strengthen the pelvic floor muscles that support the bladder, which can improve bladder control and reduce urinary incontinence.
- Prolapse: Pelvic physiotherapy can help with prolapse symptoms or post-hysterectomy. With a prolapse, there is commonly increased muscle tone causing the organ to descend. This can be improved with exercise and treatment. Post hysterectomy, there can be pelvic floor weakness or altered sensation internally which can also be treated through strengthening and sensitization work.
- Painful Intercourse: Pelvic physiotherapy can help to improve vaginal tone and elasticity, which can reduce pain and discomfort during intercourse.
How can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“While menopause symptoms can be challenging, they are not inevitable for everyone and can be managed with the right care. Triangle Physiotherapy offers specialized services to help you navigate this stage of life across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can provide personalized treatment plans to alleviate symptoms and improve your quality of life.”
Written by Roshni Ravi, Pelvic Health Physiotherapist
Stress incontinence is a type of urinary incontinence that occurs with physical activity or exertion. This can be from coughing, sneezing, laughing or exercise e.g. jumping. All of these actions can put pressure on the bladder thereby causing leaks. The pelvic floor is important in preventing this leaks and supporting the bladder.
Pelvic floor exercises such as a kegel are commonly recommended for leaks. However, a lot of time the pelvic floor is actually tight rather than weak. Reverse Kegels involve relaxing the pelvic floor muscles, allowing them to lengthen and release tension. This helps to prevent over-tightening and over-activity of the pelvic floor muscles, which can contribute to stress incontinence.

Hypertonic pelvic floor
Hypertonic pelvic floor refers to a condition where the pelvic floor muscles are in a state of excessive and persistent contraction. This can lead to a number of symptoms, including pelvic pain, urinary and fecal incontinence, and sexual dysfunction.
Hypertonic pelvic floor can be caused by a number of factors, including pregnancy, childbirth, surgery, chronic constipation, and chronic pelvic pain. It can also be a result of excessive or improper use of pelvic floor muscle exercises, such as Kegels.
Treatment for Hypertonic pelvic floor
Treatment for hypertonic pelvic floor typically involves a combination of physical therapy and relaxation techniques. Physical therapy may include manual therapy to release muscle tension, as well as exercises to stretch and relax the pelvic floor muscles. Relaxation techniques, such as deep breathing, progressive muscle relaxation, and biofeedback, can also be helpful in reducing muscle tension.
If you’re experiencing leaks, reach out to a pelvic floor therapist for an assessment or discovery call!
FAQ’s about Stress Incontinence
Q: What is stress incontinence?
A: Stress incontinence is a type of urinary incontinence that occurs when pressure is placed on the bladder, such as during coughing, sneezing, laughing, or exercising, and causes involuntary urine leakage.
Q: What causes stress incontinence?
A: Stress incontinence is typically caused by weakened pelvic floor muscles and/or a weakened urethral sphincter, which can occur due to aging, pregnancy and childbirth, menopause, obesity, chronic coughing, or certain medical conditions.
Q: Who is at risk for developing stress incontinence?
A: Women are more likely to develop stress incontinence than men, especially those who have gone through pregnancy and childbirth, menopause, or pelvic surgery. Other risk factors include obesity, chronic coughing, and certain medical conditions that affect the bladder or nervous system.
Q: How is stress incontinence diagnosed?
A: Stress incontinence can be diagnosed through a physical exam, a urine test, and other tests such as a bladder diary or urodynamic testing.
Q: What are the treatment options for stress incontinence?
A: Treatment options for stress incontinence may include:
- pelvic floor exercises,
- behavioral therapies,
- medications,
- medical devices such as pessaries, and in some cases,
- surgery.
Q: Can stress incontinence be prevented?
A: While stress incontinence may not be completely preventable, there are steps you can take to reduce your risk. Maintaining a healthy weight, doing regular pelvic floor exercises, and avoiding smoking and excessive caffeine consumption are some of these.
Q: Is stress incontinence a normal part of aging?
A: While stress incontinence is more common in older adults, it is not a normal part of aging and should not be ignored or accepted as an inevitable consequence of getting older. Treatment options are available, and seeking help from a healthcare provider is important.
Managing stress incontinence effectively involves a combination of pelvic floor exercises, lifestyle changes, and sometimes physiotherapy. For those seeking professional physiotherapy services to help manage incontinence and improve pelvic health, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans to help you achieve a leak-free life and enhanced quality of life.
Did you know children can benefit from pelvic physiotherapy too?
Most children are dry at night by school age. Approximately, 30% of children wet the bed at 4 ½ years of age. Fecal incontinence is also common in children. If a child has regular soiling or poo accidents after the age of 4 they should be assessed.
There is no cause to worry. Pelvic Health issues in children can be resolved with the help of a trained pelvic health physiotherapist at Triangle Physiotherapy.
Common conditions experienced by children include:
Constipation: infrequent bowel movements, frequent movements with pain or difficulty
Incontinence: inability to maintain bowel or bladder function. Could be inability to make it to the bathroom in time or leakage with giggles and coughing
Bed Wetting (Enuresis): leaking urine through the night while sleeping.
Voiding issues (eg. Dysfunctional voiding & postponement): inappropriately engaging pelvic floor muscles during voiding or delaying going to the bathroom, sometimes as a result of fear or pain.
Did you know 85% of children have bed wetting or fecal incontinence because of constipation?

If your child is 5 or older and experiencing any of the above symptoms pediatric Pelvic Floor Physiotherapy can help them get back to being kids, and relieve familial stress!
Our trained therapists create a personalized treatment plan with parents and children to better target your concerns and furthermore improve your child’s overall quality of life. Treatment is always in a way that is fun and engaging for your young one.
What does a pelvic floor assessment entail?
Your physical therapist will start by taking a detailed child developmental and family history. We may also ask you to complete a bladder diary to better track your child’s voiding patterns and perform a functional assessment of their breathing. Thereafter, the physiotherapist will do a visual assessment for which the child need not undress. Sometimes, the physiotherapist will use externally placed sensors to assess the functioning of the pelvic floor muscles.
Note: An internal assessment is not performed.
What does the pelvic floor treatment entail?
- Education dietary foods/irritants, habit training, digestion, pelvic floor anatomy
- Biofeedback machines using Bluetooth to keep children engaged playing games with the aid of their pelvic floor muscles.
- Electrical Stimulation
- Toilet training
- Massage
Which locations of Triangle Physiotherapy offer Pediatric Pelvic Health in Toronto?
Pediatric Pelvic Floor Physiotherapy is offered at Triangle Physiotherapy North York, Triangle Physiotherapy Mississauga and Triangle Physiotherapy Lawrence Park.
Click here to book an appointment for your child.
Pediatric pelvic floor physiotherapy is essential for addressing bladder and bowel control issues in children. Triangle Physiotherapy offers specialized services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team provides personalized care to help young patients overcome these challenges and improve their quality of life.
What is incontinence?
Incontinence can be a fairly sensitive or embarrassing subject to those who suffer from it. Incontinence is the involuntary loss of urine or feces from the bladder and bowel. But know this, incontinence is an ACCIDENT, it is something that is uncontrollable and can happen to any expecting mother.
Urinary incontinence affects around 10-13 million men and women, and it is twice as common in women as in men. Anthony Atala, MD, said, “I would say virtually all pregnant women experience some type of incontinence”. Incontinence should not rule your pregnancy or your life.

What does pregnancy have to do with incontinence?
Pregnancy can interfere with the normal way your urethra relaxes and contracts. You are able to urinate when the muscles around your urethra relax, allowing urine to pass through your bladder and out of your body. After urination, the muscles around your urethra contract, holding off urine flow until your body is ready to urinate again. Hormone changes during pregnancy and the additional pressure on the bladder from your uterus can cause stress incontinence. Mothers who are experiencing stress incontinence may urinate whilst sneezing, walking, coughing, laughing, running, and during exercise. Women who have a family history of incontinence, gain more weight than recommended during pregnancy, and are over the age of 35 are at higher risk of experiencing incontinence.
How do I avoid incontinence during pregnancy?
There are numerous ways to avoid pregnancy incontinence, along with visiting a pelvic health physiotherapist, to avoid leakage.
- Schedule your bathroom breaks. Try to make it to the toilet at least every two hours, as when pregnant, women urinate more frequently.
- If you think your bathroom visits are proper, try practicing kegel exercises. Kegels help strengthen the pelvic floor. Practicing a kegel is the same as stopping the flow of urine within your urethra. Contract your muscles to the count of ten and then release. Repeat exercises ten to twenty times in a row two to three times a day. The average time to see results is four to eight weeks of regular practice.
- Watching your weight while carrying has a significant effect on developing incontinence. Women who gain more weight during pregnancy are more likely to experience incontinence. Combining these factors with your pelvic physiotherapist will lower your risk of developing incontinence during your pregnancy, allowing your experience to be worry-free.
If you are still unsure or worried about the risk of incontinence during your pregnancy, contact a pelvic floor physiotherapist at Triangle Physiotherapy. Triangle Physiotherapy has eight convenient locations: Etobicoke, Oakville, Mississauga, North York, Toronto, and King West. At Triangle Physiotherapy, our team is compromised of professionals who love what they do. Triangle staff will ensure that you will have a safe and comfortable pregnancy while in their care, and will help get your pregnancy back on track and in your hands.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Incontinence during pregnancy can be challenging, but physiotherapy can help manage symptoms and improve pelvic floor strength. If you’re looking for specialized physiotherapy services to support incontinence management, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans to help you stay comfortable and healthy throughout your pregnancy journey.










