Axillary Web Syndrome (AWS) is a condition that often affects individuals who have undergone breast cancer treatments, particularly those who have had axillary lymph node dissection (ALND) or radiation therapy. This condition, also known as “cording,” involves the development of tight bands or cords of tissue in the armpit area, which can extend down the arm, causing pain and restricting movement. Though it is a common aftereffect of breast cancer treatment, AWS is not always well understood. In this blog, we’ll explore what AWS is, its symptoms, how it affects daily life, and how physiotherapy can help manage the condition.
If you have more questions about Axillary Web Syndrome, the cancer rehab physiotherapists at Triangle Physiotherapy would be more than happy to help you out.
What is Axillary Web Syndrome?
AWS occurs when tight bands of tissue, or “cords,” form under the skin in the armpit (axilla) and sometimes along the upper arm. These bands are typically made of scar tissue or fibrosis that develops after the removal of lymph nodes or following radiation therapy, both of which are common treatments for breast cancer. These tight bands can cause significant discomfort, limit the range of motion, and affect daily activities, such as reaching, lifting, or even carrying objects.
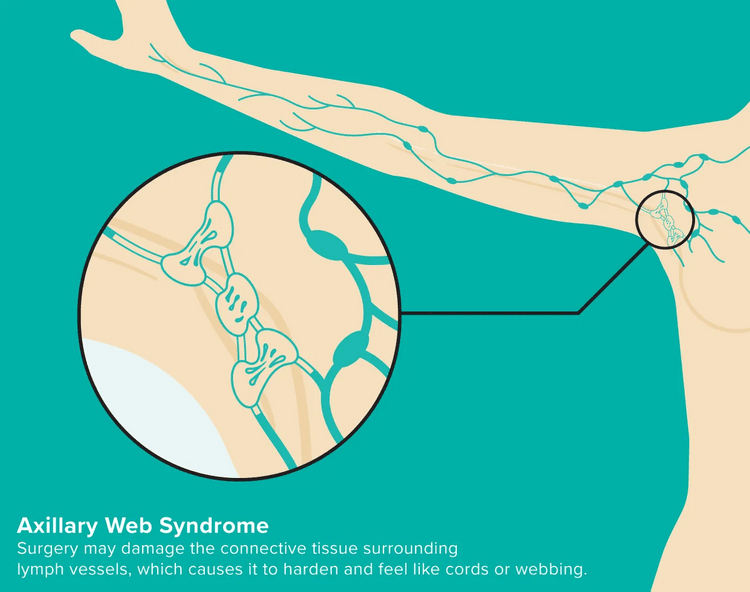
Picture Credit: healthline.com
AWS is usually diagnosed when the cords are palpated (felt) by a healthcare professional during a physical exam. In some cases, individuals may notice the bands themselves or feel a pulling sensation in the arm or chest.
Symptoms of AWS
The most noticeable symptom of AWS is the formation of tight, rope-like cords in the armpit area, but other symptoms may include:
- Pain: The cords can be painful to the touch and can cause discomfort during everyday activities.
- Restricted Mobility: Individuals with AWS often experience limited range of motion in the shoulder and arm, particularly when reaching overhead or behind.
- Tightness: A sensation of tightness or pulling in the chest, armpit, and down the arm is common.
- Swelling: Some people may also experience swelling in the arm or hand due to lymphatic fluid build-up, especially if there has been lymph node removal.
These symptoms can make simple tasks, like putting on a shirt, lifting objects, or even driving, much more difficult. For many people, AWS can impact their emotional well-being as well, as chronic pain and restricted mobility can be frustrating and limiting.
How Does AWS Affect Daily Life?
The symptoms of AWS can significantly affect an individual’s daily life. Limited shoulder and arm mobility can interfere with work, hobbies, and social activities. Pain and tightness may make it hard to perform basic activities, like reaching for items on a high shelf, carrying groceries, or participating in exercise. As a result, people with AWS may become less active, which can lead to muscle weakness, poor posture, and a reduced quality of life.
Additionally, AWS can lead to long-term issues, such as decreased self-esteem and increased stress, as individuals cope with their physical limitations. It’s important for people with AWS to seek support and find ways to manage the condition so that they can maintain a high quality of life during their recovery journey.
How Physiotherapy Can Help
Physiotherapy is one of the most effective treatments for managing AWS. A physiotherapist can develop a personalized rehabilitation program to help manage pain, improve mobility, and reduce the tightness associated with the condition. Common physiotherapy treatments for AWS include:
- Manual Therapy: Techniques like massage or myofascial release can help release tension in the affected tissues, reducing pain and increasing flexibility.
- Stretching and Mobility Exercises: Physiotherapists will guide patients through stretching exercises to improve the range of motion in the shoulder and arm. This can help reduce tightness and discomfort, allowing for greater movement.
- Strengthening Exercises: Strengthening the muscles around the shoulder and upper arm is essential for improving function and reducing strain. Physiotherapists can design specific exercises to help restore muscle strength and support the joint.
- Scar Tissue Management: Physiotherapists can use specific techniques to address scar tissue buildup that can contribute to AWS, helping to soften and break down fibrous tissue, improving movement and reducing pain.
Axillary Web Syndrome is a condition that can develop after breast cancer treatments and cause pain, tightness, and limited mobility. While it can be frustrating and limiting, it’s important to know that physiotherapy can be an effective way to manage the symptoms and improve quality of life. By working with a physiotherapist, individuals with AWS can regain movement, reduce discomfort, and take steps toward better overall health and well-being. If you or someone you know is experiencing symptoms of AWS, don’t hesitate to seek help and explore the benefits of physiotherapy for relief. Our Cancer Rehab Physiotherapists at Triangle Physiotherapy have training in helping individuals who have had cancer treatments to improve their quality of life.
Chemotherapy is an essential treatment for many types of cancer, but it often comes with side effects that can vary widely from person to person. While chemotherapy works to eliminate cancer cells, it can also affect healthy cells, leading to a range of physical symptoms. These side effects can be temporary, but they may be uncomfortable and affect your daily life.
When it comes to the side effects of cancer treatment, the cancer rehabilitation physiotherapists at Triangle Physiotherapy are knowledgeable and trained in helping you regain function and get back your quality of life.

In this post, we’ll cover 5 common symptoms to expect after chemotherapy and tips on how to manage them.
1. Fatigue
Fatigue is one of the most common side effects following chemotherapy. Unlike typical tiredness, this type of exhaustion can be overwhelming and persistent, making even the smallest tasks feel like a major effort. Chemotherapy can affect your red blood cells, which are responsible for carrying oxygen throughout your body, leading to feelings of extreme tiredness.
- What you can do: Try to rest when needed, but don’t forget to incorporate light activity into your day, like short walks or stretching. Small, frequent activities can boost your energy levels and help prevent muscle weakness. Additionally, make sleep a priority, and aim for a balanced diet to ensure your body has the nutrients it needs to recover.
2. Nausea and Vomiting
Chemotherapy drugs can trigger nausea and vomiting, which are especially common right after treatment. These symptoms occur because the chemotherapy affects the gastrointestinal tract, leading to discomfort in your stomach. The severity of nausea can vary depending on the drugs used, but it’s one of the most common concerns for many patients undergoing treatment.
- What you can do: Your doctor may prescribe anti-nausea medications, so make sure to take them as directed. Drinking small sips of water, ginger tea, or clear broths can help settle your stomach. Also, eating smaller, more frequent meals—rather than larger meals—can prevent your stomach from feeling overwhelmed. Avoiding heavy, greasy, or spicy foods may also reduce nausea.
3. Hair Loss
Hair loss is often one of the more noticeable side effects of chemotherapy. The powerful medications used during chemotherapy target rapidly dividing cells, including those in your hair follicles, which can cause your hair to fall out. Hair loss can begin within a few weeks of starting chemotherapy and can affect not just the scalp, but eyebrows, eyelashes, and body hair as well.
- What you can do: While hair loss is difficult to avoid, there are ways to manage it emotionally. Many people choose to wear wigs, scarves, or hats to help them feel more comfortable. If hair loss is affecting your self-esteem, consider talking to a counselor or joining a support group to help cope with the emotional impact. The good news is that hair usually starts to grow back once treatment is complete, though it might have a different texture or color temporarily.
4. Sensation Loss (Neuropathy)
Chemotherapy can cause nerve damage, leading to sensations of numbness, tingling, or weakness, particularly in the hands and feet. This condition, known as peripheral neuropathy, can be distressing and affect your ability to perform daily tasks like buttoning a shirt or walking. It happens because chemotherapy can damage the nerves responsible for sending signals to the brain, leading to these sensations.
- What you can do: While there’s no quick fix for neuropathy, there are ways to manage it. Talk to your doctor about medications that can help with nerve pain or discomfort. You might also benefit from physical therapy, which can help you improve balance and coordination. Taking care of your feet and hands by avoiding injury and wearing comfortable, well-fitting shoes can also reduce the impact of neuropathy. If you’re struggling with these symptoms, your healthcare provider can suggest exercises or tips to help alleviate the discomfort.
5. Changes in Appetite and Taste
Another side effect many chemotherapy patients experience is a shift in their appetite or the way food tastes. Chemotherapy can alter your sense of taste, often causing food to have a metallic or bitter flavor. In some cases, you might feel a loss of appetite, making it harder to eat enough to maintain your strength.
- What you can do: Try eating smaller meals more often throughout the day. If your appetite is low, experiment with foods that have strong flavors, such as citrus fruits or savory herbs, to help stimulate your taste buds. If food tastes off, using plastic utensils or drinking through a straw can sometimes help reduce the metallic taste. Additionally, staying hydrated and maintaining a balanced diet is important to ensure you’re getting enough nutrients.
Chemotherapy can be a life-saving treatment, but it often comes with side effects that may affect your quality of life. Fatigue, nausea, hair loss, sensation loss, and changes in appetite or taste are common symptoms that many patients face, but they are manageable with the right care and support. It’s important to communicate openly with your healthcare team about any symptoms you’re experiencing so they can adjust your treatment plan or provide supportive care to ease discomfort.
Cancer rehab will help you get back on your feet and help get rid of your neuropathy gradually. For breast cancer rehab, please remember to consult our expert physios who will help you get rid of the tight inelastic cords that formed due to radiation. You may notice it as shoulder restriction, but it needs to be treated by a physiotherapist over time.
Remember, recovery from chemotherapy is a gradual process, and many of these side effects will improve after treatment ends. Focus on taking care of your body, staying connected with your medical team, and reaching out for support when needed.
Reach out to us at Triangle Physiotherapy to book an assessment to get help managing Cancer Treatment side effects.
Chemotherapy-induced peripheral neuropathy (CIPN) is a common side effect that can significantly impact the quality of life for cancer patients. As chemotherapy drugs target rapidly dividing cells, they can inadvertently affect nerve cells, leading to symptoms that range from mild discomfort to debilitating pain. Understanding CIPN and exploring management strategies are essential steps in supporting patients through their cancer journey.
The Cancer Rehabilitation Physiotherapists at Triangle Physiotherapy are trained to help you navigate through the side effects of cancer treatment.
Understanding Chemotherapy-Induced Peripheral Neuropathy
CIPN is characterized by damage to the peripheral nerves, which can manifest in various ways, including tingling, numbness, burning sensations, and weakness in the hands and feet. This condition is not only uncomfortable but can also hinder daily activities and diminish overall well-being. Different chemotherapy agents, particularly platinum-based drugs, taxanes, and vinca alkaloids, are known to pose a higher risk for developing neuropathy.
Symptoms and Impact
The symptoms of CIPN can be diverse, including:
- Sensory changes: Tingling, numbness, or a “pins and needles” sensation.
- Motor issues: Weakness that may affect fine motor skills.
- Pain: Burning or sharp pain that can be constant or intermittent.
- Balance problems: Difficulty walking or maintaining stability, increasing the risk of falls.
The psychological impact of CIPN should not be overlooked, as patients may experience anxiety, depression, or a sense of loss of independence. Understanding the multifaceted nature of CIPN is crucial for effective management.
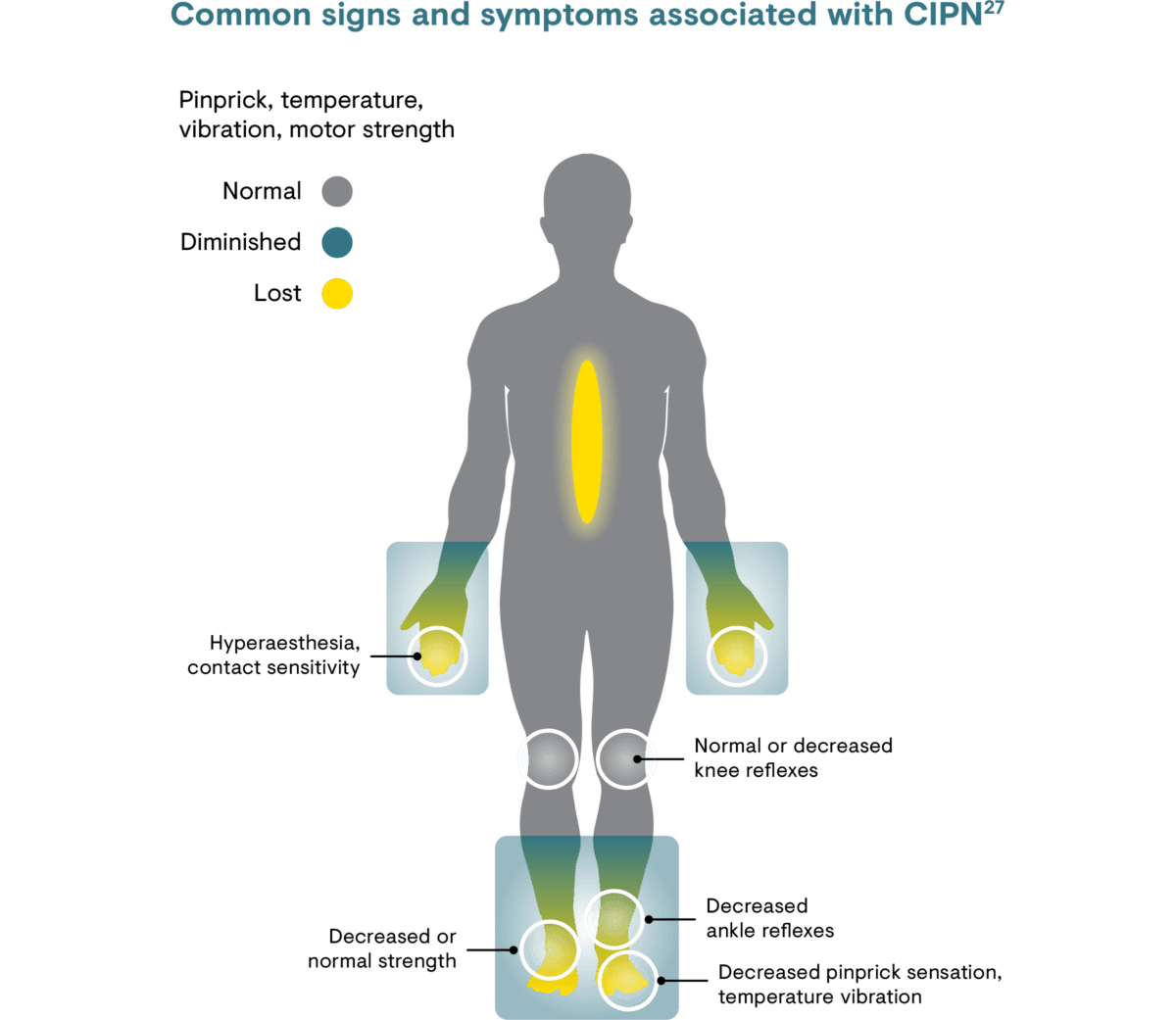
Picture Credit: https://www.grunenthal.com
Management Strategies
Education and Awareness
Empowering patients with knowledge about CIPN is vital. Understanding the potential for neuropathy allows patients to communicate effectively with their healthcare team and advocate for their needs. Regular screenings for neuropathy can help catch symptoms early, allowing for timely intervention.
Pharmacological Approaches
Medications such as anticonvulsants (e.g., gabapentin, pregabalin) and antidepressants (e.g., duloxetine) are often used to manage neuropathic pain. While these medications can be effective, it’s important for patients to discuss potential side effects and the best options for their individual situation with their oncologist.
Physical Rehabilitation
Engaging in physiotherapy can significantly aid in managing CIPN symptoms. A tailored rehabilitation program may include:
- Strength training: Gentle exercises to improve muscle strength and coordination.
- Balance training: Activities to enhance stability and reduce the risk of falls.
- Sensory retraining: Exercises that help patients re-learn normal sensations and improve tactile discrimination.
Incorporating regular physical activity can also boost overall health and mood.
Lifestyle Modifications
Adopting healthy lifestyle choices can help mitigate CIPN symptoms. Patients may benefit from:
- Nutritional support: A balanced diet rich in antioxidants and vitamins can support nerve health.
- Hydration: Staying well-hydrated may help reduce symptoms.
- Mindfulness practices: Techniques such as yoga, meditation, and deep-breathing exercises can reduce stress and improve overall well-being.
Complementary Therapies
Some patients find relief through complementary therapies such as acupuncture, massage, or mindfulness-based practices. While research on these therapies is still ongoing, many report positive outcomes in managing pain and improving quality of life.
CIPN FAQs
What should I do if I experience symptoms of CIPN?
It’s important to communicate any symptoms to your healthcare provider as soon as they arise. Early intervention can help manage symptoms more effectively.
Can CIPN be prevented?
While not all cases of CIPN can be prevented, discussing dose adjustments or alternative therapies with your oncologist may help mitigate risks.
How long does CIPN last?
The duration of CIPN varies among patients. Some may experience symptoms that resolve over time, while others may have persistent issues. Regular follow-up with your healthcare team is essential.
Is there a cure for CIPN?
Currently, there is no definitive cure for CIPN, but various management strategies can significantly alleviate symptoms and improve quality of life.
How common is CIPN?
Peripheral neuropathy after chemotherapy is very common. Experts estimate it’s experienced by 30% to 50% of patients who receive these types of chemotherapy.
The drugs most likely to cause CIPN are used to treat the most common types of cancer, including breast cancer, colon cancer, lung cancer, and prostate cancer.
Where can I find a physiotherapist that can help me with CIPN?
Triangle Physiotherapy has physiotherapists that are trained in helping you navigate the side effects caused by cancer treatments.
Breast cancer and pelvic health are two significant aspects of women’s health that can intersect in various ways. Breast cancer treatment can affect your bladder, sexual and/or pelvic function. Anywhere between 50 to 70 per cent of women will experience these kinds of issues after treatment.1
What are the known risk factors for Breast Cancer?
Risk Factors:
- Genetics: Family history, BRCA1 and BRCA2 gene mutations.
- Hormonal factors: Early menstruation, late menopause, hormone replacement therapy.
- Lifestyle factors: Alcohol consumption, obesity, lack of physical activity.
- Age: Risk increases with age.
What are the most common symptoms of Breast Cancer?
Symptoms:
- Lumps in the breast or underarm
- Changes in breast shape or size
- Skin dimpling or irritation
- Nipple discharge
How is Pelvic Health connected to Breast Cancer?

Many types of breast cancer are estrogen-positive, which means higher estrogen levels in the blood can increase cancer risk. Treatment for these cancers often involves medication that blocks estrogen reception to slow or delay cancer growth. Although this approach is effective against estrogen-positive breast cancer, it can impact pelvic floor health. One common side effect is vaginal dryness, which can adversely
affect the health of the vulvar and vaginal tissues. Incontinence, pelvic pain, sexual dysfunction can occur as a side effect of cancer treatments and these are conditions a pelvic health physiotherapist can help with.
How does estrogen affect the pelvic floor?
Breast cancer treatments that lead to lower levels of estrogen in the body which can induce symptoms similar to menopause. Estrogen is important for vaginal health because it keeps the tissues plump, pliable and lubricated. Hormone treatment, chemotherapy and/or ovary suppression or removal can all decrease estrogen levels in the body. Lower estrogen levels can lead to the thinning of vaginal tissues, vaginal dryness, burning, itching, an increased urge to urinate, the leakage of urine, recurring urinary tract infections, pelvic pressure, discomfort and pain with sexual activity.
How can I relieve pelvic pain during breast cancer treatment?
If you experience pelvic pain or pressure during treatment, consider these strategies to alleviate the discomfort:
- Engage in an exercise routine, provided your healthcare provider approves. Physical activity, such as walking, jogging, or yoga, can be beneficial.
- Use cold or hot compresses to help ease the pain.
- Take over-the-counter medications, but only if they are approved by your doctor.
- Perform pelvic floor exercises as recommended by your pelvic floor physiotherapist.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Understanding the connection between breast cancer and pelvic health is crucial for comprehensive care. If you’re looking for expert support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can help address pelvic health concerns and support you through every step of your recovery journey.
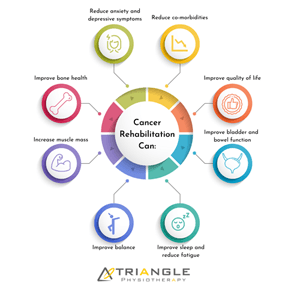
Introduction to Cancer Rehab
Cancer rehabilitation physiotherapy is a form of physiotherapy for people who have been diagnosed with cancer or for those who are undergoing cancer treatment. The goal of cancer rehab physiotherapy is to help manage and treat the side effects of cancer treatment.
Our cancer rehab physiotherapist will conduct a thorough assessment of your physical condition and medical history.
What are some conditions that cancer rehab can help with?
Common cancer rehab conditions our registered physiotherapists can help with are:
- Balance problems
- Pain
- Breathing difficulties
- Neuropathy
- Muscle weakness
- Fatigue
- Lymphedema
- Range of motion and mobility issues
- Pelvic health issues
What are some tips to prepare for my cancer rehab appointment?
Some tips for preparing for your cancer rehab physiotherapy appointment are:
- We recommend you drink plenty of water and have a light meal before your appointment.
- Complete the necessary forms before your appointment.
- Remember to bring your doctor’s note to your appointment if your insurance requires one for billing.
- Wear comfortable clothing that allows easy movement.
- Gather any relevant medical information and documentation and bring it to your appointment.
- Make a list of any medications you’re taking.
- Try to get enough rest before the appointment.
How to find a cancer rehab physiotherapy service in Oakville?
Triangle Physiotherapy Oakville is located at 2501 Prince Michael Drive, unit 2 and it’s in the same plaza as Shoppers Drug Mart and Starbucks. The main intersection is Trafalgar and Dundas. There is free parking available
How to find a cancer rehab physiotherapy service in Mississauga?
Triangle Physiotherapy Erin Mills is located at 2520 Eglinton Ave W, Unit 205 across from the Credit Valley Hospital. The main intersection is Eglinton and Erin Mills. Parking is available in the building at $1.00 for 30 minutes.
FAQ
Who can benefit from cancer rehab physiotherapy?
Individuals who have undergone or are currently undergoing cancer treatment can benefit from cancer rehab physiotherapy.
Would cancer rehab physiotherapy help during all stages of cancer treatment?
Cancer rehab physiotherapy can be helpful during all stages of cancer treatment, including before, during, and after treatment.
What kind of treatment is included in a cancer rehab physiotherapy session?
It may include some exercises, modalities, and manual therapy. Your physiotherapist will assess you and create a personalized treatment plan for you.
Is cancer rehab physiotherapy safe?
Yes, cancer rehab physiotherapy is designed to be safe, effective, and beneficial to cancer patients. It has been known to significantly improve the quality of life of Cancer Survivors.
What are the 4 stages of Cancer Rehab?
According to the Dietz Classification of Cancer Rehabilitation, there are 4 Stages in Cancer Rehabilitation.
- Preventative Rehabilitation: Early intervention and exercise to identify potential impairments and prevent or delay complications related to cancer or therapies.
- Restorative Rehabilitation: For cancer patients with the potential to attain full functional recovery, restorative rehabilitation offers comprehensive therapy to regain function to return to work or school.
- Supportive Rehabilitation: For patients with temporary or permanent deficits from cancer and/or treatments, and patients with slowly progressive or chronic cancer, supportive rehabilitation can give the opportunity to re-establish and maintain functional independence.
- Palliative Rehabilitation: For patients with treatment-refractory cancer or advanced disease, less intense palliative rehabilitation may play a role in assisting the patient and their family by maximizing patient comfort and reducing caregiver burden,
Click HERE to book an appointment with a cancer rehab physiotherapist near you.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
The article discusses rehabilitation programs for cancer patients, focusing on improving quality of life during and after treatment. These programs are tailored to address the physical and emotional challenges faced by cancer patients, including pain management, mobility improvement, and emotional support. Triangle Physiotherapy offers specialized services to help patients regain strength and functionality across various locations in the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village.
How do I choose the Best Physiotherapist Near Me?

When choosing a physiotherapist, it’s essential to find someone who meets your specific needs and can provide high-quality care. Here are some steps you can take to help you pick the best physiotherapist:
- Ask for recommendations: Ask your friends, family, or colleagues for recommendations. Personal referrals can be valuable as they come from people you trust.
- Research their experience and specialization: Look for a physiotherapist with experience and expertise in treating your specific condition or injury. Physiotherapy covers a broad range of areas, such as sports injuries, post-surgery rehabilitation, back pain, or neurological disorders. Choosing someone who specializes in your area of concern can increase the chances of effective treatment.
- Check credentials and qualifications: Ensure that the physiotherapist you’re considering is licensed and registered to practice in Ontario. You can usually verify their credentials through the College of Physiotherapists of Ontario.
- Read reviews and testimonials: Search online for reviews or testimonials from previous patients. Although individual experiences may vary, reading about others’ experiences can give you an idea of the physiotherapist’s reputation and patient satisfaction.
- Assess communication and rapport: A good physiotherapist should listen and communicate well. They should be able to understand your concerns, explain your condition or treatment plan clearly, and answer any questions you may have. It’s important to feel comfortable and have a good rapport with your physiotherapist to ensure a positive therapeutic relationship.
- Consider practical factors: Take into account the location of the physiotherapy clinic or practice. It’s generally more convenient to choose a clinic that is easily accessible to you, whether it’s close to your home or workplace. Additionally, check their availability and scheduling options to see if they can accommodate your needs.
- Insurance coverage: If you have health insurance, check if the clinic provides direct billing to your insurance. This way you only have to pay a copayment or deductible if required by your plan.
- Initial Assessment: Schedule an initial assessment with the physiotherapist to discuss your condition, treatment options, and their approach. This can give you a sense of their knowledge, professionalism, and whether their treatment philosophy aligns with your goals.
What are the types of specializations that physiotherapists can have?

Physiotherapists have training in assessing, diagnosing, and treating a wide range of physical conditions and injuries. Physiotherapists can specialize in various areas of practice based on their interests, expertise, and advanced training. Some common specializations that our physiotherapists in Toronto have include:
- FCAMPT – The highest level of training in orthopedic manual therapy
- McKenzie Certification
- Cancer Rehab
- Pelvic Health – Assessing and treating pelvic floor conditions in men and women
- Vestibular Rehab & Concussion Therapy
- Running Assessments
- Sports Physiotherapy
These are just a few examples of the specializations within physiotherapy. It’s worth noting that some physiotherapists may have expertise in multiple areas or choose to focus on specific sub-specialties within these broader categories.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Choosing the best physiotherapist near you is crucial for effective treatment and recovery. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team is dedicated to providing personalized care tailored to your needs, helping you achieve your health goals.”
After a breast cancer diagnosis, many women are left to face new challenges caused by the side effects of their cancer treatments. While some side effects tend to disappear on their own over time, many side effects can have long-lasting physical and emotional consequences.
What are the common side effects of breast cancer treatment?
Breast surgery, such as a mastectomy, lumpectomy, or reconstruction, can cause many women to experience pain and physical limitations such as difficulty moving their arm, weakness, swelling, and scar tightness. In addition, some women may also develop pathologies such as post-mastectomy pain syndrome and axillary web syndrome following surgery.
Furthermore, both chemotherapy and radiation therapy also have their side effects, including fatigue, tingling, numbness in the hands/feet (chemotherapy-induced peripheral neuropathy), and radiation fibrosis, among many others.
These physical and psychological side effects of breast cancer treatments can significantly impact your daily functioning and independence both at home and at work. Research shows that both physiotherapy and exercise can help to alleviate many of these side effects and play an essential role in your recovery during and after breast cancer.
What are the benefits of breast cancer rehabilitation?
Physiotherapy interventions can help you to:
- Restore your arm movement
- Improve your shoulder, trunk, and abdominal strength
- Decrease your pain
- Improve your flexibility
- Improve your energy and endurance
- Reduce your risk of developing lymphedema
- Improve your posture and body awareness
In addition, exercise is also known to address many side effects, such as bone density issues related to hormonal medication, reducing your risk of developing lymphedema, and improving cancer-related fatigue in addition to also reducing your risk of reoccurrence. Physiotherapists are exercise specialists who will work with you to provide a safe and effective exercise program.
At Triangle, we are committed to helping women improve their health and well-being during each stage of their cancer recovery.
What are the components of breast cancer rehabilitation?
Every woman undergoing breast cancer treatment is different and hence will have unique rehabilitation needs. Your physiotherapist will use a combination of treatment techniques best suited for your condition. Interventions may include:
- Manual (hands-on) techniques such as soft-tissue mobilization and myofascial release to improve your flexibility and manage conditions such as radiation fibrosis and axillary web syndrome.
- Scar Massage
- Exercises to improve your shoulder movement and strength
- Exercises to improve your endurance and overall energy levels
- Individualized education regarding risk reduction and early detection of lymphedema
- Energy conservation techniques
- Education on how to return to physical activity
- Home exercise program
What are the most common misconceptions about Breast Cancer Rehabilitation?
There is a common misconception that for months or years after breast cancer surgery or radiation therapy, women should not use the arm on the affected side for lifting or working because they might get lymphedema or other problems. Research tells us this is FALSE, in fact with a proper physiotherapy program most women can achieve greater strength and function in the affected arm than what they had before surgery; with no increase in the chances of getting lymphedema.
Another misconception is that Breast Cancer Physiotherapy is the same as an exercise program. Physiotherapists are highly trained professionals able to independently diagnose and treat problems with pain or movement using a wide range of assessment methods and treatments, of which a specialized exercise program is one piece.
What does a typical session at Triangle Physiotherapy look like?
Your Physiotherapist will conduct a thorough assessment of the issue. This will include asking questions about your cancer treatment and the problems you’re having, other relevant medical information, and questions about your goals for therapy. They will do a physical assessment of the problem which could include assessing movements, strength and fitness, scar tissue, nerve function, and/or injuries from radiation or surgery. Your Physiotherapist will then clearly communicate all of their findings to you and describe their proposed treatment plan.
How many sessions will I need?
There is no one recipe for the number of treatment sessions or the length of time required for full recovery. Some conditions will require only a few sessions while others may require more intensive treatments and several sessions. Whatever your prognosis, your physiotherapist at Physiotherapy Oakville will clearly communicate expected timelines with you.
Joining Physiotherapy Oakville ensures you receive a personalized treatment plan based on scientific assessment and evidence-based practices. Research has shown that tailored physiotherapy programs can significantly enhance recovery outcomes. By understanding your specific needs and providing clear communication about your progress, the team at Physiotherapy Oakville helps you achieve optimal recovery in the most efficient timeframe.
What types of healthcare professionals can be involved in breast cancer rehabilitation at Triangle Physiotherapy?
Breast cancer rehabilitation is typically delivered by a multidisciplinary team of healthcare professionals. This team may include physiotherapists, acupuncturists, pelvic health physiotherapists, exercise specialists, nutritionists, and massage therapists.
Click HERE to book an appointment with a cancer rehab physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Rehabilitation after breast cancer treatment is crucial for regaining strength and improving quality of life. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists provide personalized care to help you recover and thrive after breast cancer treatment.”







