Pelvic health is something most of us don’t think about – until something starts to feel off. Whether it’s leaking during a laugh or a dull ache you’ve learned to live with, subtle signs of pelvic floor dysfunction often go unnoticed or are shrugged off as “normal.” But they don’t have to be.
At Triangle Physiotherapy Toronto, we specialize in pelvic floor physiotherapy to help people of all genders take control of their health and live without discomfort, shame, or limitations. Not sure if you need to see a pelvic physiotherapist? Here are five clinical (and very human) signs it might be time.
1. You Leak When You Cough, Laugh, or Work Out
If you’ve ever peed a little while sneezing, lifting weights, or jumping, you’re not alone. Stress incontinence is incredibly common – especially after childbirth or during menopause – but it’s not something you just have to accept. Pelvic floor physiotherapy helps retrain those muscles so you can move freely without worrying about leaks.
2. You Experience Pelvic Pain or Pressure
That constant feeling of heaviness in your lower belly or pelvis? Or sharp pain during your period, intercourse, or even when sitting? These are often signs of a tense, imbalanced, or weakened pelvic floor. A proper assessment can help pinpoint the cause – and pelvic physiotherapy can relieve the pain without the need for invasive treatment.
3. You’re Recovering from or Preparing for Birth or Surgery
If you’ve had a vaginal or C-section delivery, or surgery like a hysterectomy or prostate procedure, your pelvic muscles have gone through a lot. Even if everything “looks fine,” rebuilding strength, alignment, and control post-recovery is key. Pelvic physiotherapy can help improve bladder and bowel control, reduce pain, and make everyday movements feel normal again. Pelvic floor strengthening is crucial during pregnancy, allow us to help you build the skill and strength for it!
4. You’re Always Rushing to the Washroom
Are you constantly on edge, planning your day around bathroom breaks? Do you sometimes not make it in time? Urinary urgency and frequency can be related to pelvic floor dysfunction. With guided techniques and muscle retraining, a physiotherapist can help calm that sense of urgency and restore your confidence.
5. You’re Constipated or Struggling with Bowel Movements
Pelvic floor issues don’t only affect the bladder – they impact bowel health too. If you’re straining, feeling incomplete relief, or experiencing pain during bowel movements, it could be related to pelvic muscle coordination. Pelvic physiotherapy works with your body – not against it – to improve regularity and ease.
When to Reach Out

If any of these signs sound familiar, don’t wait. You deserve answers and a plan that makes sense. At Triangle Physiotherapy Toronto, we offer private, personalized pelvic floor physiotherapy in a safe and supportive environment. Our experienced team is here to help you regain control, feel stronger, and live with more ease – one session at a time.
Book a confidential consultation today and take the first step toward healing.
Your body will thank you.
An episiotomy is a surgical incision made in the perineum (the patch of skin between the vaginal opening and the anus) during childbirth, is a common procedure to aid in a smoother delivery. Despite its benefits, an episiotomy can lead to discomfort, pain, and complications in postpartum recovery. This blog explores how a pelvic health physiotherapist can play a crucial role in managing and alleviating post-episiotomy issues, ensuring a healthier recovery for new mothers.
Our trained and experienced Pelvic Health Physiotherapists in Mississauga can make a significant difference to your recovery after child-birth.

Why is an episiotomy performed during delivery?
An episiotomy may be performed by the obstetrician during delivery for various reasons:
1. Prevent Severe Tearing
2. Facilitate a Faster Delivery
In situations where a rapid delivery is required for the safety of the baby or mother, an episiotomy can speed up the process. This is particularly crucial in cases of:
- Fetal Distress: If the baby shows signs of distress, such as an abnormal heart rate, a quick delivery becomes essential. An episiotomy can help expedite the birth, reducing the risk of complications for the baby.
- Prolonged Labor: When labor is not progressing, and the baby is not moving down the birth canal as expected, an episiotomy can aid in accelerating the delivery.
3. Assisted Deliveries
Episiotomies are more commonly performed during assisted deliveries involving instruments like forceps or vacuum extractors.
4. Shoulder Dystocia
Shoulder dystocia occurs when the baby’s shoulder becomes lodged behind the mother’s pelvic bone during delivery. This can be a critical situation requiring immediate intervention. An episiotomy can provide additional room for the baby’s shoulder to be maneuvered and delivered safely.
5. Large Baby
When a baby is larger than average, delivering them vaginally can be challenging. An episiotomy may be performed to create more space, reducing the risk of severe tearing and facilitating a smoother delivery.
6. Previous Pelvic Surgery or Scarring
What is the role of a pelvic health physiotherapist in recovering from an Episiotomy?
A pelvic health physiotherapist specializes in the rehabilitation of pelvic floor muscles. They are trained to address issues related to childbirth, including those arising from an episiotomy. At Triangle Physiotherapy Mississauga, our pelvic health physiotherapists are highly trained in helping new mothers navigate their post-partum recovery.
- Pain Management and Scar Tissue Mobilization
- Pelvic Floor Rehabilitation
- Bladder and Bowel Function Improvement
- Addressing Incontinence: Many women experience urinary or fecal incontinence after an episiotomy. Pelvic health physiotherapists can help manage these issues through targeted exercises and lifestyle modifications.
- Diet and Hydration Advice: Proper diet and hydration are essential for optimal bladder and bowel function. Physiotherapists offer valuable advice on nutrition that supports recovery.
- Posture and Mobility
- Improving Posture: Poor posture can exacerbate pelvic pain. Physiotherapists help new mothers correct their posture, reducing strain on the pelvic floor and aiding in overall recovery.
- Safe Return to Activity: Guiding new mothers on safely returning to physical activities is vital. Physiotherapists create gradual exercise plans to ensure a safe and effective return to daily activities and fitness routines.
- Emotional Support and Counseling
- Addressing Psychological Aspects: The postpartum period can be emotionally challenging. Physiotherapists provide emotional support and can refer patients to mental health professionals if needed, ensuring a holistic approach to recovery.
- Building Confidence: Encouraging words and positive reinforcement from physiotherapists can boost new mothers’ confidence in their recovery journey.
If you have had an episiotomy during delivery, contact us to book an appointment to see one of our pelvic health physiotherapists in Mississauga to get started on the road to recovery.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 2 convenient locations in Mississauga that offer pelvic health:
Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Recovering from an episiotomy can be challenging, but with the help of a pelvic health physiotherapist, you can regain your strength and confidence. Triangle Physiotherapy offers specialized care at multiple locations across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team is here to support you every step of the way.”
When we think about pelvic health, we often think of women’s issues, but did you know that men also have a pelvic floor? That’s right! The male pelvic floor is a group of muscles that support the bladder, bowel, and sexual organs.
However, just like any other muscle group, the male pelvic floor can become weakened or tense, leading to a variety of issues. For example, pelvic pain, urinary or fecal incontinence, and erectile dysfunction can all be caused by pelvic floor dysfunction.

What are the Causes of Pelvic Floor Dysfunction in Men?
When we think about pelvic health, we often think of women’s issues, but did you know that men also have a pelvic floor? That’s right! The male pelvic floor is a group of muscles that support the bladder, bowel, and sexual organs.
However, just like any other muscle group, the male pelvic floor can become weakened or tense, leading to a variety of issues. For example, pelvic pain, urinary or fecal incontinence, and erectile dysfunction can all be caused by pelvic floor dysfunction.
The pelvic floor conditions we see in men are:
- Post-Prostatectomy Incontinence
- Post-prostatectomy Erectile dysfunction
- Pelvic Pain – Testicular & Penile pain, Chronic Prostatitis
How is Pelvic Floor Dysfunction diagnosed in Men?
Once you come in for an initial assessment, a qualified pelvic health physiotherapist will begin by taking a detailed medical history and a review of your symptoms, followed by an assessment of your symptoms and pelvis.
Once the cause of your pain or dysfunction has been diagnosed, your pelvic health physiotherapist will discuss the findings with you, as well as explain treatment options and expected outcomes.
What to Expect During Pelvic Floor Physiotherapy for Men?
Your pelvic floor physiotherapist will design an individual treatment plan that would aim to meet your goals, which may include one or more of the following; pelvic floor and pelvic muscle exercises, education, mindfulness and relaxation techniques, and bladder and bowel training.
Where can I find a men’s pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Pelvic Health physiotherapists advocate the importance of educating individuals about their pelvic health. They are often asked by patients if an internal exam is necessary. Many patients refrain from seeking help for pelvic health issues because of the fear of internal examination. While internal exams are not a must, they can be very helpful to pelvic health physiotherapists in determining the condition of the pelvic floor.
What is an Internal Pelvic Exam?
A pelvic floor assessment, which may or may not include an internal pelvic exam, entails a pelvic health physiotherapist examining the pelvic floor muscles, tissues, and organs by inserting a gloved hand into the vagina or rectum. This examination is crucial for assessing the well-being and performance of the pelvic floor, allowing for the detection of any possible problems or issues.
Why is an internal pelvic exam important?
- Detailed Assessment of Pelvic Floor Muscles: An internal pelvic exam allows the physiotherapist to assess the tone, strength, flexibility, and coordination of the pelvic floor muscles. This information is crucial in developing an accurate understanding of the patient’s pelvic health.
- Identification of Muscle Imbalances: Through internal palpation, a physiotherapist can identify any muscle imbalances or asymmetries in the pelvic floor. This helps in tailoring the treatment plan to address specific issues, such as hypertonic (overactive) or hypotonic (underactive) muscles.
- Assessment of Pelvic Organ Function: Internal examination enables the physiotherapist to assess the function of pelvic organs, such as the bladder, uterus, and rectum. This is important in cases where dysfunction or weakness in the pelvic floor muscles may be contributing to issues such as urinary incontinence or pelvic organ prolapse.
- Evaluation of Connective Tissues and Nerves: The internal exam allows the physiotherapist to assess the condition of connective tissues, ligaments, and nerves in the pelvic region. Dysfunction in these structures can contribute to pelvic pain and other symptoms, and the internal exam helps in identifying such issues.
- Assessment of Trigger Points and Tenderness: The physiotherapist can identify trigger points and areas of tenderness within the pelvic floor muscles. This information is crucial in designing a targeted treatment plan, which may include manual therapy techniques to release muscle tension.
- Feedback on Exercise Performance: During an internal pelvic exam, the physiotherapist may guide the patient through specific exercises to assess the effectiveness of pelvic floor muscle contractions. Real-time feedback helps the patient learn proper muscle engagement and control.
- Patient Education and Empowerment: The internal exam provides an opportunity for the physiotherapist to educate the patient about their pelvic floor anatomy, function, and any specific issues identified during the assessment. This empowers the patient to actively participate in their treatment plan and make lifestyle changes that support pelvic health.

Do I have to have an internal exam during a pelvic health assessment?
It’s important to note that internal pelvic exams are conducted with the patient’s informed consent, and physiotherapists ensure a comfortable and respectful environment during the assessment. The goal is to provide comprehensive care and address the specific needs of individuals experiencing pelvic health issues. That being said, if you are not comfortable being internally examined, please let your physiotherapist know before the start of your assessment.
How do I prepare for an internal pelvic exam?
Preparing for an internal pelvic exam involves a combination of physical and mental preparation. It’s essential to communicate openly with your pelvic health physiotherapist and follow their instructions. Here are some general guidelines to help you prepare:
Comfortable Clothing: Wear comfortable, easy-to-remove clothing. You may be asked to undress from the waist down, so wearing a skirt or loose pants can be convenient.
Relaxation Techniques: Practice relaxation techniques such as deep breathing to help ease anxiety and tension. Relaxing your pelvic muscles can make the exam more comfortable.
Communicate with your Physiotherapist: Inform your pelvic health physiotherapist about any concerns, fears, or past traumatic experiences related to pelvic exams. They can adjust their approach and provide additional support.
Ask Questions: Feel free to ask any questions you may have about the procedure. Knowing what to expect can help alleviate anxiety.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Understanding the need for an internal exam during a pelvic health assessment can help you make informed decisions about your care. If you’re looking for specialized support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can provide comprehensive pelvic health assessments tailored to your comfort and needs.
Triangle Physiotherapy in Mississauga is a full-service clinic that offers specialized services like Pelvic Health Physiotherapy. Our pelvic health physiotherapists are trained professionals who, apart from being experts in their field, are also empathetic individuals who understand the sensitive nature of the conditions that make people seek pelvic health physiotherapy.
Tell me more about your Mississauga Pelvic Health physiotherapists.

Our Mississauga Pelvic Health physiotherapists have training in the field of pelvic health physiotherapy and are committed to providing the best care to the community in Mississauga, be it new moms, women with prolapse or incontinence issues, pessary fittings, labour and delivery support, and more. We also have a pelvic health physiotherapist who is trained to help children. Our pelvic health physiotherapists are also able to help men with their pelvic health issues.
What type of conditions can a pelvic floor physiotherapist treat?
Some of the conditions treated by our Mississauga Pelvic Health physiotherapists are:
- Incontinence (urinary and fecal)
- Pelvic organ prolapse and pessary fittings
- Constipation
- Diastasis recti
- Vaginismus
- Pelvic pain
- Pelvic girdle pain during pregnancy and postpartum)
- Coccydynia (tailbone pain)
- Pudendal neuralgia
- Interstitial cystitis
- Female and Male Sexual dysfunction
- Prostatitis
- Rectal pain and dysfunction
- Irritable bowel syndrome
- Anal incontinence
- Anal fissures and fistulas
- Anal neuralgia
- Rectal prolapse
I just gave birth recently. How soon should I see a pelvic health physiotherapist
The pelvic floor muscles may get stretched or damaged during delivery, whether by C-Section or vaginal. This may cause issues of the pelvic floor that manifest as urinary or fecal incontinence, urinary urgency or frequency, pain during sexual activity, pelvic organ prolapse, pelvic pain, lower back pain, diastasis recti, or scar pain. Many of these issues can be addresed by pelvic health physiotherapy, however, our pelvic physiotherapists in Mississauga recommend waiting at least six weeks after delivery to allow the body time to heal from childbirth.
Can I speak to a pelvic health physiotherapist in Mississauga prior to booking a consultation?
We can certainly connect you with the best pelvic floor physiotherapist in Mississauga that can answer any questions you may have. Click here to book a discovery call.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Finding the right pelvic health physiotherapist is crucial for effective treatment and recovery. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists specialize in pelvic health, providing personalized treatment plans to help you achieve the best possible outcomes.”
Introduction to Cancer Rehab
Cancer rehabilitation physiotherapy is a form of physiotherapy for people who have been diagnosed with cancer or for those who are undergoing cancer treatment. The goal of cancer rehab physiotherapy is to help manage and treat the side effects of cancer treatment.
Our cancer rehab physiotherapist will conduct a thorough assessment of your physical condition and medical history.
What are some conditions that cancer rehab can help with?
Common cancer rehab conditions our registered physiotherapists can help with are:
- Balance problems
- Pain
- Breathing difficulties
- Neuropathy
- Muscle weakness
- Fatigue
- Lymphedema
- Range of motion and mobility issues
- Pelvic health issues
What are some tips to prepare for my cancer rehab appointment?
Some tips for preparing for your cancer rehab physiotherapy appointment are:
- We recommend you drink plenty of water and have a light meal before your appointment.
- Complete the necessary forms before your appointment.
- Remember to bring your doctor’s note to your appointment if your insurance requires one for billing.
- Wear comfortable clothing that allows easy movement.
- Gather any relevant medical information and documentation and bring it to your appointment.
- Make a list of any medications you’re taking.
- Try to get enough rest before the appointment.
How to find a cancer rehab physiotherapy service in Oakville?
Triangle Physiotherapy Oakville is located at 2501 Prince Michael Drive, unit 2 and it’s in the same plaza as Shoppers Drug Mart and Starbucks. The main intersection is Trafalgar and Dundas. There is free parking available
How to find a cancer rehab physiotherapy service in Mississauga?
Triangle Physiotherapy Erin Mills is located at 2520 Eglinton Ave W, Unit 205 across from the Credit Valley Hospital. The main intersection is Eglinton and Erin Mills. Parking is available in the building at $1.00 for 30 minutes.
FAQ
Who can benefit from cancer rehab physiotherapy?
Individuals who have undergone or are currently undergoing cancer treatment can benefit from cancer rehab physiotherapy.
Would cancer rehab physiotherapy help during all stages of cancer treatment?
Cancer rehab physiotherapy can be helpful during all stages of cancer treatment, including before, during, and after treatment.
What kind of treatment is included in a cancer rehab physiotherapy session?
It may include some exercises, modalities, and manual therapy. Your physiotherapist will assess you and create a personalized treatment plan for you.
Is cancer rehab physiotherapy safe?
Yes, cancer rehab physiotherapy is designed to be safe, effective, and beneficial to cancer patients. It has been known to significantly improve the quality of life of Cancer Survivors.
What are the 4 stages of Cancer Rehab?
According to the Dietz Classification of Cancer Rehabilitation, there are 4 Stages in Cancer Rehabilitation.
- Preventative Rehabilitation: Early intervention and exercise to identify potential impairments and prevent or delay complications related to cancer or therapies.
- Restorative Rehabilitation: For cancer patients with the potential to attain full functional recovery, restorative rehabilitation offers comprehensive therapy to regain function to return to work or school.
- Supportive Rehabilitation: For patients with temporary or permanent deficits from cancer and/or treatments, and patients with slowly progressive or chronic cancer, supportive rehabilitation can give the opportunity to re-establish and maintain functional independence.
- Palliative Rehabilitation: For patients with treatment-refractory cancer or advanced disease, less intense palliative rehabilitation may play a role in assisting the patient and their family by maximizing patient comfort and reducing caregiver burden,
Click HERE to book an appointment with a cancer rehab physiotherapist near you.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
The article discusses rehabilitation programs for cancer patients, focusing on improving quality of life during and after treatment. These programs are tailored to address the physical and emotional challenges faced by cancer patients, including pain management, mobility improvement, and emotional support. Triangle Physiotherapy offers specialized services to help patients regain strength and functionality across various locations in the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village.
Menopause can be a very overwhelming time for a lot of women. During this period, there are a lot of hormonal changes that can influence the way you feel in your body. Menopause tends to start between the ages of 45 to 55. This can include a range of symptoms such as hot flashes and mood swings to vaginal dryness and changes in pelvic health.

How does Menopause affect pelvic health?
Many women don’t realize that menopause can affect pelvic health. As estrogen levels decline, tissues in the vagina, urethra, and bladder can become thinner, drier, and less elastic, leading to a condition called vaginal atrophy. This can cause uncomfortable symptoms such as vaginal dryness, itching, burning, and pain during sex. In addition, menopause can also increase the risk of pelvic floor disorders, such as incontinence and prolapse. But don’t worry, many of these conditions can be improved through pelvic physiotherapy!
What is pelvic floor physiotherapy?
Pelvic floor physiotherapy is a specialized form of physiotherapy that focuses on the pelvic floor muscles, which support the pelvic organs (bladder, uterus, and rectum) and control bladder and bowel function. Pelvic physiotherapy can help to improve pelvic health during menopause and beyond, providing relief from uncomfortable symptoms and reducing the risk of pelvic floor disorders.
What does Pelvic Health Physiotherapy Involve?
Pelvic floor physiotherapy involves a range of techniques designed to improve the strength, coordination, and function of the pelvic floor muscles. These techniques may include pelvic floor exercises, biofeedback, electrical stimulation, manual therapy, and education on lifestyle modifications. It is an effective alternative to drug based therapy and surgery, and allows for you to take your health into your own hands.
How Can Pelvic Physiotherapy Help During Menopause?
- Pelvic physiotherapy can help to address a range of pelvic health issues that can arise during menopause, including:
- Vaginal Dryness: Pelvic physiotherapy can help to improve blood flow to the vaginal area, which can increase lubrication and reduce discomfort during intercourse. Additionally, exercises to strengthen the pelvic floor muscles can help to improve vaginal tone and elasticity.
- Urinary Incontinence: Pelvic physiotherapy can help to strengthen the pelvic floor muscles that support the bladder, which can improve bladder control and reduce urinary incontinence.
- Prolapse: Pelvic physiotherapy can help with prolapse symptoms or post-hysterectomy. With a prolapse, there is commonly increased muscle tone causing the organ to descend. This can be improved with exercise and treatment. Post hysterectomy, there can be pelvic floor weakness or altered sensation internally which can also be treated through strengthening and sensitization work.
- Painful Intercourse: Pelvic physiotherapy can help to improve vaginal tone and elasticity, which can reduce pain and discomfort during intercourse.
How can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“While menopause symptoms can be challenging, they are not inevitable for everyone and can be managed with the right care. Triangle Physiotherapy offers specialized services to help you navigate this stage of life across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can provide personalized treatment plans to alleviate symptoms and improve your quality of life.”
What is vaginismus?
Vaginismus is a condition where the muscles around the vagina involuntarily contract, making it difficult or impossible to have vaginal penetration.
Do I have vaginismus?
If you answer yes to one or more of the following questions, you must book an appointment with a pelvic health physiotherapist to find out if you have vaginismus.
“Sex is so uncomfortable for me.”
“Why does it hurt to have sex? My doctor cannot find anything wrong with me.”
“Internal pelvic exams are a no for me – they are so painful.”
“My vagina feels like a fort that is impenetrable. I never realized it was vaginismus.”
“I used to have great sex, but now I close up—it burns and stings.”
“When my partner starts to move inside me, it hurts and we have to stop.”
“I don’t wear tampons because they don’t go in.”
What are the symptoms of vaginismus?
The symptoms may differ between younger and older women, emphasizing the significance of an accurate diagnosis and effective treatment for vaginismus.
The primary symptoms of vaginismus are:
- Sexual penetration seems physically impossible despite repeated attempts
- Difficulty inserting tampons from youth even after repeated attempts.
- Difficulty undergoing internal pelvic/gynecological exam
What are the causes of Vaginismus?

The exact causes of vaginismus can vary from person to person, and in many cases, the condition is multifactorial, meaning that multiple factors may contribute to its development. Here are some potential causes and contributing factors:
- Psychological factors: Emotional or psychological factors can play a significant role in vaginismus. Past traumatic experiences, such as sexual abuse, rape, or a history of painful intercourse, can contribute to the development of vaginismus. Anxiety, fear, guilt, or negative beliefs about sex can also trigger involuntary muscle contractions.
- Fear of pain or discomfort: Some individuals may develop vaginismus due to a fear of pain or discomfort during sexual intercourse. This fear can be based on previous painful experiences, cultural or religious beliefs, or misinformation about sex.
- Relationship issues: Difficulties in the relationship, such as poor communication, lack of trust, unresolved conflicts, or sexual problems, can contribute to the development or persistence of vaginismus. Emotional or physical distance between partners can create tension and anxiety during sexual activity.
- Cultural or religious factors: Cultural or religious beliefs and practices surrounding sex can influence a person’s perception of sexuality and contribute to the development of vaginismus. Upbringing that emphasizes guilt, shame, or negative attitudes towards sex can lead to involuntary muscle contractions during attempts at vaginal penetration.
- Lack of sexual education: Insufficient knowledge or understanding about sexual anatomy, arousal, and relaxation techniques can contribute to vaginismus. Inadequate sexual education may lead to misconceptions, anxiety, and fear surrounding sexual activity.
- Medical conditions or infections: Certain medical conditions, such as vaginal infections, urinary tract infections, endometriosis, or pelvic inflammatory disease, can cause pain during sex, leading to the development of vaginismus. Vaginal dryness or atrophy, often associated with menopause, can also contribute to discomfort and muscle tightness.
- Traumatic childbirth experiences: Some women may develop vaginismus after experiencing a traumatic childbirth, especially if they had a difficult or painful delivery. The association of vaginal penetration with the traumatic event can trigger involuntary muscle contractions.
What are the treatment options for vaginismus?
Pelvic health physiotherapy is a common treatment option for vaginismus. It involves a physical therapist working with the patient to help relax and strengthen the pelvic floor muscles.
Possible treatments include:
- Progressive pelvic floor muscle relaxation
- Biofeedback or muscle stimulation
- Yoga-based therapy
- Hip mobility work
- Lumbar spine mobility work
What can I expect during an assessment and treatment for vaginismus at Triangle Physiotherapy?
Assessment
The first step in pelvic health physiotherapy for vaginismus is usually an assessment of the patient’s pelvic floor muscles. This may involve an internal examination, but the therapist will always seek the patient’s consent and respect their comfort level.
Treatment
Once the assessment is complete, the therapist will develop a treatment plan tailored to the patient’s needs. This may involve exercises to strengthen the pelvic floor muscles or techniques to help the patient relax those muscles.
Techniques
One common technique used in pelvic health physiotherapy for vaginismus is called progressive muscle relaxation. This involves tensing and then releasing the pelvic floor muscles in a controlled way to help the patient become more aware of them and learn how to control them.
Another technique that may be used is biofeedback. This involves using sensors to monitor the activity of the pelvic floor muscles, which can help the patient learn to control them more effectively.
Overall, pelvic health physiotherapy can be an effective treatment for vaginismus, but it is important to work with a qualified physical therapist who has experience in this area. With patience, persistence, and the right guidance, many people with vaginismus can overcome their condition and enjoy fulfilling sexual relationships.
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you. Book an Appointment today!
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Managing vaginismus and improving intimacy is possible with the right physiotherapy care. Triangle Physiotherapy offers specialized pelvic health services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you overcome pain and enhance your intimate relationships through personalized treatment plans.”
Written by Roshni Ravi, Pelvic Health Physiotherapist.
Sexual health is an important aspect of overall health and well-being, but it’s not always an easy topic to talk about. Many women experience sexual health dysfunctions at some point in their lives, but they may feel embarrassed or ashamed to seek help by way of pelvic floor physiotherapy. There are currently large gaps in the sexual education provided at the elementary school level. Many sex ed classes are focused on birth control and how terrible periods are.
But there is not enough information, if any, on sexual health conditions and how to seek help. We’ve had a lot of conversations with patients about what they wish they had learned in sex-ed. In this blog post, we’ll explore some of the most commonly asked questions about sexual health dysfunctions in women and offer some tips for managing them.
What is pelvic floor physiotherapy?

Pelvic floor physiotherapy focuses on treating the muscles, ligaments, and connective tissues of the pelvic floor which is a group of muscles that form a supportive hammock-like structure at the base of the pelvis. They play a key role in maintaining continence, supporting the pelvic organs, and providing stability to the spine and hips.
Pelvic floor physiotherapy involves a range of exercises, manual therapy techniques, and education to help individuals with pelvic floor dysfunction. Common conditions that may benefit from pelvic floor physiotherapy include:
- urinary and fecal incontinence,
- pelvic pain,
- pelvic organ prolapse, and
- sexual dysfunction.
Why am I suffering from a low libido? Can pelvic floor physiotherapy help?
Many women experience a decrease in sexual desire at some point in their lives. This can be caused by a variety of factors, including stress, hormonal imbalances, and relationship issues. To manage low libido, it’s important to address any underlying issues and make self-care a priority. This can include:
- practicing stress-management techniques,
- getting enough sleep, and
- engaging in regular exercise.
Why does it hurt to have sex?
Painful intercourse, also known as dyspareunia, is a common sexual health dysfunction in women. It can be caused by a variety of factors, including vaginal dryness, infections, and hormonal imbalances. To manage painful intercourse, it’s important to work with a healthcare provider to identify the underlying cause and develop a treatment plan. This may include using:
- lubricants,
- treating infections,
- or using hormonal therapy.
I struggle to orgasm during sex, why does that happen?
Many women struggle to achieve orgasm during sexual activity which can be caused by a variety of factors, including, stress, relationship issues, and hormonal imbalances. To manage orgasmic dysfunction, it’s important to work with a healthcare provider or therapist to address any underlying issues and develop strategies for improving sexual function. This may include:
- practicing mindfulness or
- engaging in self-exploration techniques.
My vagina feels like a fort that is impenetrable. Why can I not have sexual intercourse?
Vaginismus is a condition in which the muscles of the vaginal wall contract involuntarily, making intercourse difficult or impossible. It can be caused by a variety of factors, including past trauma and anxiety. To manage vaginismus, it’s important to work with a healthcare provider or therapist to address any underlying issues and develop strategies for managing anxiety and relaxing the pelvic floor muscles.
What is vulvodynia? Do I need pelvic floor physiotherapy?
Vulvodynia is a chronic pain condition that affects the vulva, or external genitalia. It can cause burning, stinging, or itching sensations, and can make sexual activity painful or uncomfortable. To manage vulvodynia, it’s important to work with a healthcare provider to identify the underlying cause and develop a treatment plan. This may include:
- using topical creams or medications,
- practicing relaxation techniques, or
- seeing a pelvic health physiotherapist.
Help! I pee my pants!

Urinary incontinence is a common condition in which urine leaks from the bladder involuntarily. It can be caused by a variety of factors, including hormonal changes, pregnancy, and pelvic floor dysfunction. To manage urinary incontinence, it’s important to work with a healthcare provider or pelvic floor physiotherapist to develop a treatment plan. This may include:
- pelvic floor exercises,
- bladder training, or
- medications.
What are the signs of menopause?
Menopause can cause a variety of changes in sexual function, including vaginal dryness, decreased libido, and painful intercourse. To manage these changes, it’s important to work with a healthcare provider to develop a treatment plan. This may include:
- using hormonal therapy,
- vaginal moisturizers, or
- engaging in regular sexual activity to maintain pelvic floor health.
Where can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
In conclusion…
Many women experience sexual health dysfunctions at some point in their lives, but they may feel embarrassed or ashamed to seek help. It’s important to remember that sexual health is an important aspect of overall health and well-being, and it’s important to prioritize it in your self-care routine. If you’re experiencing any issues related to sexual function, don’t hesitate to talk to your healthcare provider or a therapist about your options. Remember, there is help!
Click here to book your consultation with one of our knowledgeable and compassionate pelvic health physiotherapists.
“Pelvic floor physiotherapy is essential for improving sexual health and overall well-being. Triangle Physiotherapy offers specialized pelvic health services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can help you address pelvic floor issues and enhance your sexual health through personalized treatment plans.”
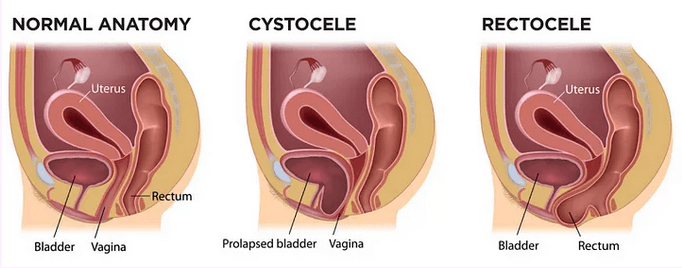
Pelvic organ prolapse (POP) is a condition in which there is a descent of the pelvic organs into or through the vaginal or anal canal. This can present as:
- a visible bulge in the above openings,
- pressure felt in the pelvic area,
- incomplete emptying of bladder or bowels,
- discomfort during intercourse.
The main reason for prolapse is increased pressure on the pelvic floor due to:
– Chronic constipation
– Bearing children
– Pelvic floor weakness due to hormonal imbalance
Conservative non-surgical management is the first line of treatment for POP.
Your pelvic floor physiotherapist will assess the severity of your symptoms, the strength of your pelvic floor and your ability to manage pressure and stresses to your pelvic floor. Treatment would include strengthening exercises for the core and pelvic floor muscles and coordination techniques for all the inner unit muscles.
The types of pelvic organ prolapse are:
- Anterior Wall Prolapse
- Posterior Wall Prolapse
- Rectal Prolapse
Depending on the grade and type of prolapse, you might be a candidate for a pessary fitting.

A pessary is a medical grade silicone device that is inserted into the vaginal canal in order to support the vaginal walls. If you are a candidate for a pessary, it must be fitted for you by a trained professional such as gynaecologists, nurses that have a certification in fittings or pelvic health physios that are specialized to do so.
We currently have 3 practitioners at Triangle Physiotherapy who are certified in pessary fittings.
Your pelvic floor deserves more than just kegels. Speak to a pelvic health physiotherapist today to get started!
Where can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills










