When it comes to women’s health, two conditions often mentioned together are Polycystic Ovary Syndrome (PCOS) and Endometriosis. While both can impact fertility and overall well-being, they are distinct conditions with different causes, symptoms, and treatments. The pelvic health physiotherapists at Triangle Physiotherapy help us break down the key differences to help you better understand them.
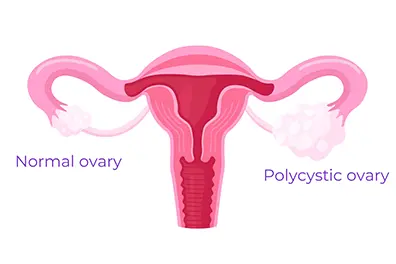
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects how the ovaries function. It is one of the most common endocrine disorders among women of reproductive age.
Common Symptoms of PCOS:
- Irregular or Absent Periods: Due to hormonal imbalances, women with PCOS often experience infrequent or prolonged menstrual cycles.
- Excess Hair Growth and Acne: Elevated levels of androgens (male hormones) can lead to hirsutism (excess facial and body hair), acne, and even hair thinning on the scalp.
- Insulin Resistance: Many women with PCOS struggle with insulin resistance, which can increase the risk of type 2 diabetes.
- Ovarian Cysts: Despite its name, not all women with PCOS have cysts on their ovaries, but some may develop multiple small fluid-filled sacs.
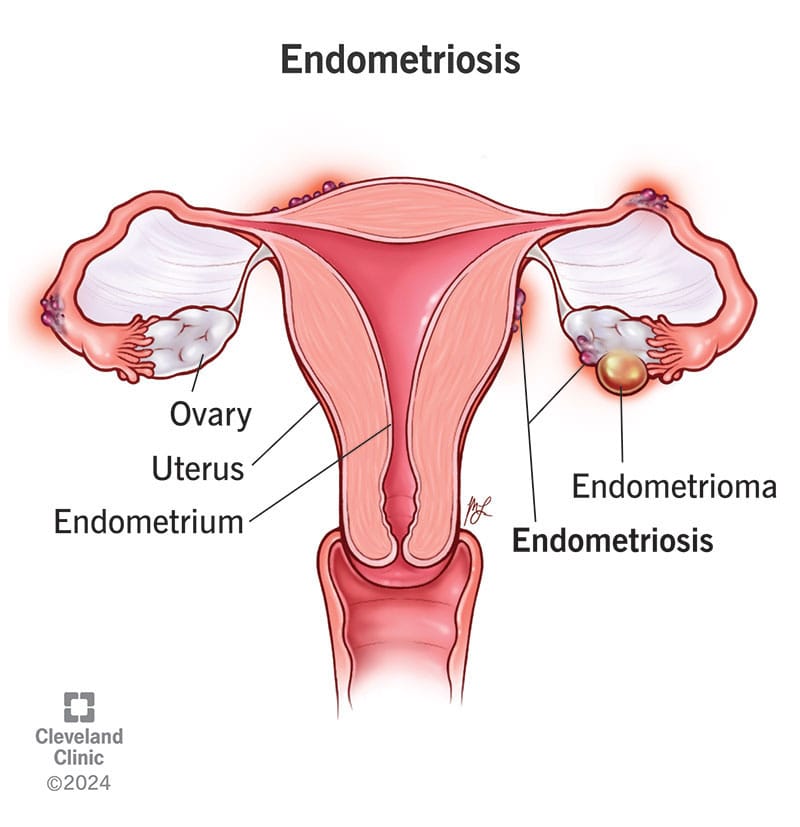
What is Endometriosis?
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside of it, leading to inflammation, scarring, and pain.
Common Symptoms of Endometriosis:
- Severe Menstrual Cramps: One of the hallmark symptoms of endometriosis is intense pelvic pain that can start before and last beyond the menstrual cycle.
- Heavy Periods: Women with endometriosis often experience unusually heavy menstrual bleeding.
- Pain During Intercourse: Pain during or after sex is a common complaint due to the presence of endometrial-like tissue outside the uterus.
- Chronic Pelvic Pain: Many women with endometriosis experience ongoing pelvic discomfort, even outside their periods.
Key Differences Between PCOS and Endometriosis
| Feature | PCOS | Endometriosis |
|---|---|---|
| Cause | Hormonal imbalance | Endometrial-like tissue growing outside the uterus |
| Periods | Irregular or absent | Heavy and painful |
| Pain | Not always present | Severe pelvic pain |
| Fertility Impact | May cause ovulation issues | May lead to scarring and blockages |
| Hormonal Symptoms | Excess androgens (acne, hair growth) | Usually no androgen-related issues |
How Are PCOS and Endometriosis Treated?
Since these conditions have different causes, their treatments also vary:
- PCOS Treatment: May involve hormonal birth control, lifestyle changes, insulin-sensitizing medications (like Metformin), and fertility treatments if pregnancy is desired.
- Endometriosis Treatment: Can include pain management (NSAIDs), hormonal therapy (such as birth control or GnRH agonists), and in severe cases, surgery to remove endometrial-like tissue.
The Bottom Line
Both PCOS (Polycystic Ovary Syndrome) and Endometriosis are complex conditions that need personalized treatment. If you notice symptoms of either, it’s important to talk to a healthcare provider to get the right diagnosis and treatment plan.
Along with medical care, adding Physiotherapy Oakville can also help. Physiotherapy can ease pelvic pain, improve movement, and reduce muscle tension caused by these conditions. It supports your overall well-being and helps you feel better over time.
By combining medical advice and physiotherapy, you can manage symptoms more effectively and improve your quality of life.
💬 Do you or someone you know struggle with these conditions? Let’s continue raising awareness and supporting women’s health! 💙
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Pelvic pain is discomfort or pain experienced in the lower part of the abdomen, below the belly button and between the hips. This type of pain can affect both men and women and can arise from various conditions. The nature of pelvic pain can vary; it might be sharp, dull, intermittent, or constant, and can be acute (short-term) or chronic (lasting longer than six months).
What causes pelvic pain?

Common Causes of Pelvic Pain
In Women:
- Menstrual Cramps: Pain associated with menstruation (dysmenorrhea).
- Endometriosis: A condition where tissue similar to the lining inside the uterus grows outside of it.
- Ovarian Cysts: Fluid-filled sacs on the ovaries.
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs.
- Fibroids: Noncancerous growths in the uterus.
- Ectopic Pregnancy: A pregnancy occurring outside the uterus.
- Interstitial Cystitis: Chronic inflammation of the bladder.
In Men:
- Prostatitis: Inflammation of the prostate gland.
- Hernia: When an organ pushes through an opening in the muscle or tissue.
- Chronic Pelvic Pain Syndrome (CPPS): Persistent pain in the pelvic region.
Both Genders:
- Urinary Tract Infections (UTIs): Infections in any part of the urinary system.
- Appendicitis: Inflammation of the appendix.
- Gastrointestinal Issues: Conditions such as irritable bowel syndrome (IBS) or diverticulitis.
- Musculoskeletal Issues: Problems with muscles, ligaments, or joints in the pelvic area.
What are the symptoms related to pelvic pain?
Symptoms of pelvic pain can vary widely depending on the underlying cause and the individual. Here are common symptoms associated with pelvic pain:
General Symptoms of Pelvic Pain
- Aching or Discomfort: Persistent or intermittent pain in the lower abdomen or pelvis.
- Sharp or Stabbing Pain: Sudden, severe pain that can come and go.
- Cramping: Muscle cramps or spasms in the pelvic region.
- Pressure: A feeling of heaviness or pressure in the pelvis.
- Burning or Stinging Sensation: Particularly during urination or bowel movements.
- Pain During Physical Activity: Pain that worsens with movement, exercise, or sexual intercourse.
Additional Symptoms in Women
- Menstrual Irregularities: Pain associated with periods (dysmenorrhea), heavy bleeding, or spotting between periods.
- Pain During Ovulation: Mid-cycle pain known as mittelschmerz.
- Pain During Sexual Intercourse: Discomfort or pain during or after sex (dyspareunia).
- Vaginal Discharge: Unusual discharge that might indicate infection.
- Pain with Urination: Particularly if associated with urinary tract infections or interstitial cystitis.
Additional Symptoms in Men
- Pain in the Testicles or Scrotum: Discomfort that can radiate to the pelvic region.
- Urinary Symptoms: Difficulty urinating, frequent urination, or pain during urination.
- Pain with Ejaculation: Discomfort during or after ejaculation.
Symptoms Related to Specific Conditions
- Endometriosis: Severe menstrual cramps, pain during intercourse, and infertility.
- Pelvic Inflammatory Disease (PID): Fever, unusual vaginal discharge, and pain during sex.
- Ovarian Cysts: Sudden, severe pain if a cyst ruptures or causes twisting of the ovary (torsion).
- Ectopic Pregnancy: Sharp, stabbing pain, vaginal bleeding, dizziness, or fainting.
- Interstitial Cystitis: Chronic pelvic pain, urinary urgency and frequency, and pain during intercourse.
- Prostatitis: Pain in the pelvis, genitals, or lower back; difficulty urinating; flu-like symptoms.
- Appendicitis: Sudden, sharp pain that starts near the belly button and moves to the lower right abdomen, accompanied by fever, nausea, and vomiting.
- Hernia: A noticeable bulge in the groin or abdomen, pain that worsens with lifting or bending.
How is pelvic pain diagnosed?
Diagnosing the cause of pelvic pain typically involves:
- Medical History and Physical Examination: Initial evaluation by a healthcare provider.
- Imaging Tests: Ultrasound, CT scans, or MRI to visualize internal structures.
- Laboratory Tests: Blood tests, urine tests, or cultures to check for infections.
- Laparoscopy: A minimally invasive surgical procedure to look inside the pelvic cavity.
How is pelvic pain treated?
Treatment depends on the underlying cause and may include:
- Medications: Pain relievers, antibiotics (for infections), or hormonal treatments.
- Physiotherapy: A pelvic health physiotherapist can help with pelvic pain and related symptoms.
- Surgery: In some cases, surgical intervention may be necessary.
- Lifestyle Changes: Dietary adjustments, stress management, and other modifications.
If you or someone you know is experiencing persistent or severe pelvic pain, it’s important to seek medical attention to determine the underlying cause and appropriate treatment.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Pelvic pain can significantly impact daily life, but targeted physiotherapy can help alleviate discomfort and improve quality of life. If you are looking for professional physiotherapy services to manage pelvic pain, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and personalized treatment plans to support your pelvic health and overall well-being.
March 8th marks International Women’s Day and Triangle Physiotherapy is proud to be able to empower women to advocate for themselves and their health needs.
Our goal is to encourage women to focus on their health, both, physical and mental. Build your healthcare team and schedule regular visits, in addition to exercising regularly and eating healthy.
Women’s Health and the Pelvic Floor
Women’s health is intricately connected to the well-being of the pelvic floor, a group of muscles, ligaments, and tissues supporting the uterus, bladder, and rectum. Maintaining a healthy pelvic floor is crucial for various functions, including urinary and bowel control, sexual function, and providing support during pregnancy. Pregnancy, childbirth, hormonal changes, and aging can impact the pelvic floor, leading to issues like incontinence, pelvic organ prolapse, and sexual dysfunction.
Maintaining a healthy lifestyle, proper posture, and seeking guidance from a pelvic health physiotherapist are essential for women’s pelvic floor health. Awareness and proactive care contribute to overall well-being, enabling women to lead active and fulfilling lives while addressing potential pelvic floor challenges.
What are the symptoms of Pelvic Floor Dysfunction?
Pelvic Floor Dysfunction (PFD) can manifest through various symptoms, which may vary in intensity and duration. Common signs of PFD include:
- Urinary Issues:
- Urinary incontinence: Involuntary leakage of urine.
- Frequent urination: The need to urinate more often than usual.
- Difficulty emptying the bladder: Struggling to fully release urine.
- Bowel Issues:
- Constipation: Difficulty passing stools or infrequent bowel movements.
- Straining during bowel movements: Experiencing difficulty while trying to have a bowel movement.
- Pelvic Pain:
- Pelvic pain or discomfort: Discomfort in the pelvic region, which may be persistent or intermittent.
- Pain during sexual intercourse: Discomfort or pain during sexual activity.
- Muscle Tension:
- Tight or spasming pelvic muscles: Increased muscle tension in the pelvic floor.
- Pelvic Organ Prolapse:
- The feeling of pressure or fullness in the pelvic area: Sensation of something bulging or descending into the vagina.
- Lower Back Pain:
- Chronic lower back pain: Discomfort or pain in the lower back region.
- Changes in Posture:
- Altered posture: Changes in the alignment of the spine and pelvis.
How a Pelvic Health Physiotherapist can help and what to expect?
A Pelvic Health Physiotherapist specializes in assessing and treating conditions related to the pelvic floor and surrounding areas. Here’s how they can help and what to expect during a session:
- Assessment:
- A thorough assessment of your medical history, pelvic health, and relevant symptoms.
- Physical examination, which may include internal and external assessments to evaluate the strength, flexibility, and coordination of the pelvic floor muscles.
- Education:
- Detailed explanation of pelvic anatomy and the role of pelvic floor muscles in various functions.
- Guidance on lifestyle factors, posture, and habits that may contribute to pelvic health issues.
- Pelvic Floor Exercises:
- Prescribing personalized pelvic floor exercises, to strengthen or relax specific muscles based on the assessment findings.
- Teaching proper technique and ensuring exercises are performed correctly.
- Manual Therapy:
- Hands-on techniques to release tension in the pelvic floor muscles or surrounding tissues.
- Myofascial release and trigger point therapy to address muscle knots or tightness.
- Biofeedback:
- Using biofeedback tools to provide real-time information about pelvic floor muscle activity.
- Assisting individuals in learning how to control and coordinate their pelvic floor muscles.
- Behavioral Strategies:
- Implementing behavioral strategies for managing and improving bladder and bowel function.
- Developing strategies for optimizing pelvic health during daily activities.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
On International Women’s Day, let’s celebrate the strength and resilience of women everywhere. For those seeking expert support for their health and wellness, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas are committed to empowering women through personalized care and treatment plans.