When it comes to women’s health, two conditions often mentioned together are Polycystic Ovary Syndrome (PCOS) and Endometriosis. While both can impact fertility and overall well-being, they are distinct conditions with different causes, symptoms, and treatments. The pelvic health physiotherapists at Triangle Physiotherapy help us break down the key differences to help you better understand them.
What is PCOS?
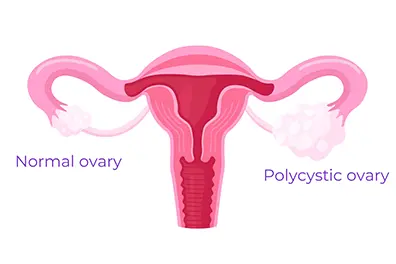
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects how the ovaries function. It is one of the most common endocrine disorders among women of reproductive age.
Common Symptoms of PCOS:
- Irregular or Absent Periods: Due to hormonal imbalances, women with PCOS often experience infrequent or prolonged menstrual cycles.
- Excess Hair Growth and Acne: Elevated levels of androgens (male hormones) can lead to hirsutism (excess facial and body hair), acne, and even hair thinning on the scalp.
- Insulin Resistance: Many women with PCOS struggle with insulin resistance, which can increase the risk of type 2 diabetes.
- Ovarian Cysts: Despite its name, not all women with PCOS have cysts on their ovaries, but some may develop multiple small fluid-filled sacs.
What is Endometriosis?
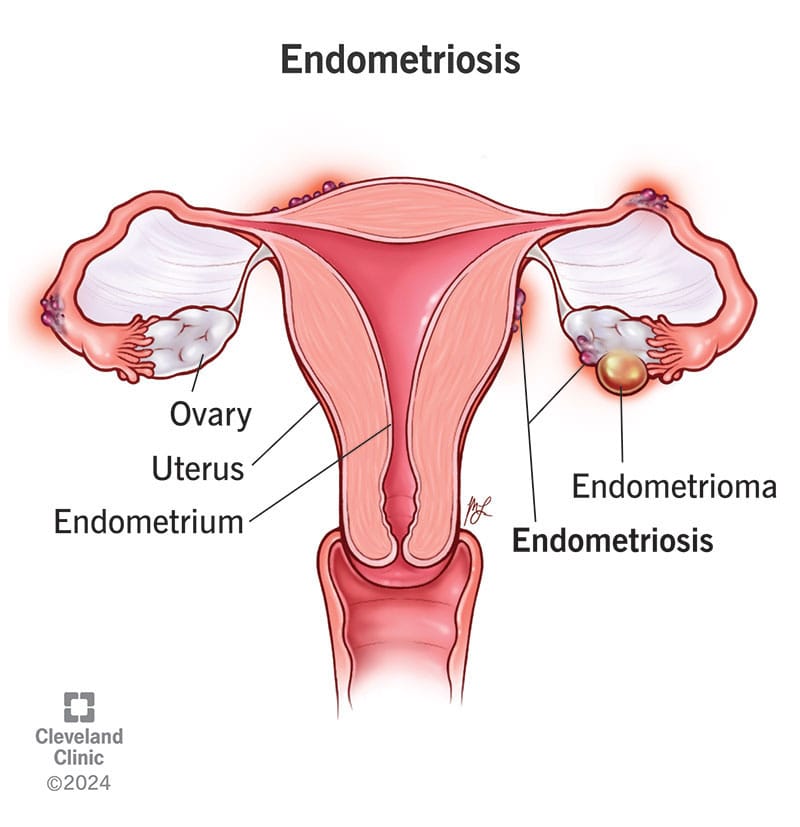
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside of it, leading to inflammation, scarring, and pain.
Common Symptoms of Endometriosis:
- Severe Menstrual Cramps: One of the hallmark symptoms of endometriosis is intense pelvic pain that can start before and last beyond the menstrual cycle.
- Heavy Periods: Women with endometriosis often experience unusually heavy menstrual bleeding.
- Pain During Intercourse: Pain during or after sex is a common complaint due to the presence of endometrial-like tissue outside the uterus.
- Chronic Pelvic Pain: Many women with endometriosis experience ongoing pelvic discomfort, even outside their periods.
Key Differences Between PCOS and Endometriosis
| Feature | PCOS | Endometriosis |
|---|---|---|
| Cause | Hormonal imbalance | Endometrial-like tissue growing outside the uterus |
| Periods | Irregular or absent | Heavy and painful |
| Pain | Not always present | Severe pelvic pain |
| Fertility Impact | May cause ovulation issues | May lead to scarring and blockages |
| Hormonal Symptoms | Excess androgens (acne, hair growth) | Usually no androgen-related issues |
How Are PCOS and Endometriosis Treated?
Since these conditions have different causes, their treatments also vary:
- PCOS Treatment: May involve hormonal birth control, lifestyle changes, insulin-sensitizing medications (like Metformin), and fertility treatments if pregnancy is desired.
- Endometriosis Treatment: Can include pain management (NSAIDs), hormonal therapy (such as birth control or GnRH agonists), and in severe cases, surgery to remove endometrial-like tissue.
The Bottom Line
Both PCOS (Polycystic Ovary Syndrome) and Endometriosis are complex conditions that need personalized treatment. If you notice symptoms of either, it’s important to talk to a healthcare provider to get the right diagnosis and treatment plan.
Along with medical care, adding Physiotherapy Oakville can also help. Physiotherapy can ease pelvic pain, improve movement, and reduce muscle tension caused by these conditions. It supports your overall well-being and helps you feel better over time.
By combining medical advice and physiotherapy, you can manage symptoms more effectively and improve your quality of life.
💬 Do you or someone you know struggle with these conditions? Let’s continue raising awareness and supporting women’s health! 💙
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Pelvic Health – Menstrual cups and menstrual discs are reusable feminine hygiene products designed to collect menstrual fluid.

What is a Menstrual Cup?
Menstrual cups are generally crafted from silicone or rubber.
Unlike tampons, which absorb blood, these cups collect it, reducing the risk of infection.
One advantage of the menstrual cup is its larger capacity compared to a tampon’s absorbency, allowing for less frequent changes. Most cups can be worn for up to 12 hours, depending on your flow.
What is a Menstrual Disc?
Unlike menstrual cups, menstrual discs sit higher in the vaginal canal, tucked behind the pubic bone. Here are some key features and benefits of menstrual discs:
- Design and Use:
- Shape: Menstrual discs are flat and round, resembling a small diaphragm, with a flexible rim and a thin, flexible body.
- Insertion: The disc is pinched and inserted into the vagina, where it is positioned horizontally and covers the cervix.
- Capacity: Like menstrual cups, discs can hold a significant amount of fluid and can be worn for up to 12 hours.
What are the benefits of a Menstrual Cup?
Benefits:
- Cost-Effective: While the initial purchase price may be higher than disposable products, menstrual cups can be reused for several years, saving money over time.
- Eco-Friendly: Reusable nature reduces waste compared to disposable tampons and pads.
- Health: Made from medical-grade materials that are safe and reduce the risk of Toxic Shock Syndrome (TSS) associated with tampons.
What are the benefits of a Menstrual Disc?
Benefits:
- Comfort: Positioned differently than cups, discs can be more comfortable for some users, especially during physical activities or sex.
- Mess-Free Intercourse: Many menstrual discs can be worn during intercourse without obstructing the vaginal canal, offering a mess-free experience.
- Eco-Friendly: Reusable menstrual discs reduce waste compared to disposable products. However, there are also single-use disposable options available.
Using a Menstrual Cup Vs. a Menstrual Disc
Using a menstrual cup involves a few steps to ensure proper insertion, positioning, and removal. Here’s a detailed guide on how to use a menstrual cup:Insertion
Wash Your Hands:
- C-fold: Press the sides of the cup together and then fold it in half to form a “C” shape.Punch-down fold: Push the rim of the cup down into the base, creating a narrower point for insertion.
Duration:
Wash Your Hands:
Sterilization:
Using a menstrual disc involves a few steps to ensure proper insertion, positioning, and removal. Here is a detailed guide on how to use a menstrual disc:Insertion
Wash Your Hands:
Duration:
Wash Your Hands:
Sterilization:
Menstrual discs and cups are both effective options for period management. Choose the one that suits you best based on factors like comfort, lifestyle, and size preference. Ultimately, neither a disc nor a cup might be the right choice for you, but they are both excellent alternatives to tampons for those seeking different options.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Choosing between a menstrual cup and a menstrual disc can depend on individual comfort and pelvic health needs. For expert advice on pelvic health and guidance on using these products, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these locations can provide personalized care and support for all your pelvic health concerns.
Pelvic pain is discomfort or pain experienced in the lower part of the abdomen, below the belly button and between the hips. This type of pain can affect both men and women and can arise from various conditions. The nature of pelvic pain can vary; it might be sharp, dull, intermittent, or constant, and can be acute (short-term) or chronic (lasting longer than six months).
What causes pelvic pain?

Common Causes of Pelvic Pain
In Women:
- Menstrual Cramps: Pain associated with menstruation (dysmenorrhea).
- Endometriosis: A condition where tissue similar to the lining inside the uterus grows outside of it.
- Ovarian Cysts: Fluid-filled sacs on the ovaries.
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs.
- Fibroids: Noncancerous growths in the uterus.
- Ectopic Pregnancy: A pregnancy occurring outside the uterus.
- Interstitial Cystitis: Chronic inflammation of the bladder.
In Men:
- Prostatitis: Inflammation of the prostate gland.
- Hernia: When an organ pushes through an opening in the muscle or tissue.
- Chronic Pelvic Pain Syndrome (CPPS): Persistent pain in the pelvic region.
Both Genders:
- Urinary Tract Infections (UTIs): Infections in any part of the urinary system.
- Appendicitis: Inflammation of the appendix.
- Gastrointestinal Issues: Conditions such as irritable bowel syndrome (IBS) or diverticulitis.
- Musculoskeletal Issues: Problems with muscles, ligaments, or joints in the pelvic area.
What are the symptoms related to pelvic pain?
Symptoms of pelvic pain can vary widely depending on the underlying cause and the individual. Here are common symptoms associated with pelvic pain:
General Symptoms of Pelvic Pain
- Aching or Discomfort: Persistent or intermittent pain in the lower abdomen or pelvis.
- Sharp or Stabbing Pain: Sudden, severe pain that can come and go.
- Cramping: Muscle cramps or spasms in the pelvic region.
- Pressure: A feeling of heaviness or pressure in the pelvis.
- Burning or Stinging Sensation: Particularly during urination or bowel movements.
- Pain During Physical Activity: Pain that worsens with movement, exercise, or sexual intercourse.
Additional Symptoms in Women
- Menstrual Irregularities: Pain associated with periods (dysmenorrhea), heavy bleeding, or spotting between periods.
- Pain During Ovulation: Mid-cycle pain known as mittelschmerz.
- Pain During Sexual Intercourse: Discomfort or pain during or after sex (dyspareunia).
- Vaginal Discharge: Unusual discharge that might indicate infection.
- Pain with Urination: Particularly if associated with urinary tract infections or interstitial cystitis.
Additional Symptoms in Men
- Pain in the Testicles or Scrotum: Discomfort that can radiate to the pelvic region.
- Urinary Symptoms: Difficulty urinating, frequent urination, or pain during urination.
- Pain with Ejaculation: Discomfort during or after ejaculation.
Symptoms Related to Specific Conditions
- Endometriosis: Severe menstrual cramps, pain during intercourse, and infertility.
- Pelvic Inflammatory Disease (PID): Fever, unusual vaginal discharge, and pain during sex.
- Ovarian Cysts: Sudden, severe pain if a cyst ruptures or causes twisting of the ovary (torsion).
- Ectopic Pregnancy: Sharp, stabbing pain, vaginal bleeding, dizziness, or fainting.
- Interstitial Cystitis: Chronic pelvic pain, urinary urgency and frequency, and pain during intercourse.
- Prostatitis: Pain in the pelvis, genitals, or lower back; difficulty urinating; flu-like symptoms.
- Appendicitis: Sudden, sharp pain that starts near the belly button and moves to the lower right abdomen, accompanied by fever, nausea, and vomiting.
- Hernia: A noticeable bulge in the groin or abdomen, pain that worsens with lifting or bending.
How is pelvic pain diagnosed?
Diagnosing the cause of pelvic pain typically involves:
- Medical History and Physical Examination: Initial evaluation by a healthcare provider.
- Imaging Tests: Ultrasound, CT scans, or MRI to visualize internal structures.
- Laboratory Tests: Blood tests, urine tests, or cultures to check for infections.
- Laparoscopy: A minimally invasive surgical procedure to look inside the pelvic cavity.
How is pelvic pain treated?
Treatment depends on the underlying cause and may include:
- Medications: Pain relievers, antibiotics (for infections), or hormonal treatments.
- Physiotherapy: A pelvic health physiotherapist can help with pelvic pain and related symptoms.
- Surgery: In some cases, surgical intervention may be necessary.
- Lifestyle Changes: Dietary adjustments, stress management, and other modifications.
If you or someone you know is experiencing persistent or severe pelvic pain, it’s important to seek medical attention to determine the underlying cause and appropriate treatment.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Pelvic pain can significantly impact daily life, but targeted physiotherapy can help alleviate discomfort and improve quality of life. If you are looking for professional physiotherapy services to manage pelvic pain, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and personalized treatment plans to support your pelvic health and overall well-being.
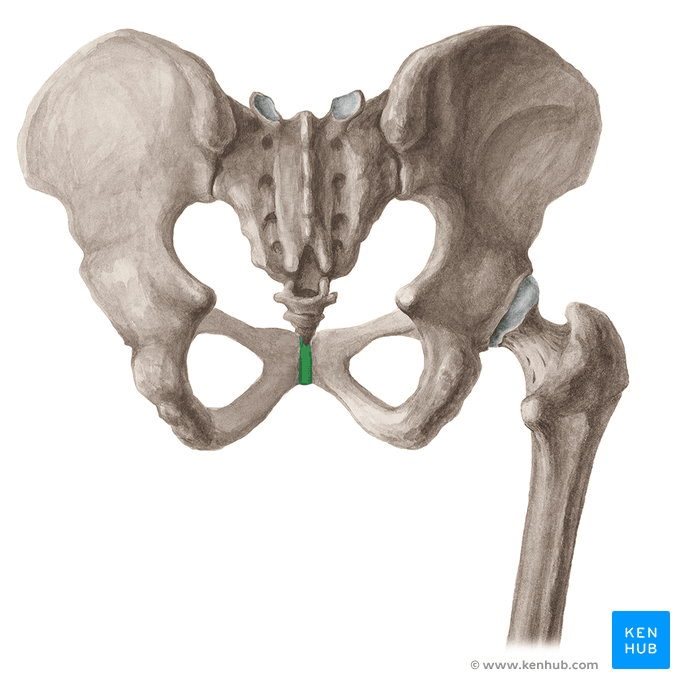
Pubic bone pain after giving birth, also known as postpartum pubic symphysis diastasis or symphysis pubis dysfunction (SPD), is a condition that affects some women following childbirth. This pain is usually centered around the pubic symphysis, the joint at the front of the pelvis where the two halves of the pelvic bone meet.
What are the causes of post-partum pubic bone pain?
- Hormonal Changes: During pregnancy, the body releases the hormone relaxin, which loosens the ligaments in the pelvis to prepare for childbirth. This can sometimes lead to instability or separation of the pubic symphysis.
- Physical Stress: The process of labor and delivery can put significant strain on the pelvic area, particularly if the baby is large, labor is prolonged, or delivery involves interventions such as forceps or vacuum extraction.
- Pre-existing Conditions: Women who had SPD or pelvic girdle pain during pregnancy are more likely to experience pubic bone pain postpartum.
What are the symptoms of symphysis pubis dysfunction (SPD)?
Pain:
- Burning, shooting, grinding or stabbing
- Mild or prolonged
- Usually relieved by rest
- Radiating to the back, abdomen, groin, perineum and legs
- Disappears commonly after giving birth (not in every case)
- Discomfort sense onto the front of the joint
- Clicking of the lower back, hip joints and sacroiliac joints when changing position
- Difficulty in movements like abduction and adduction
Locomotor difficulty:
- Walking
- Ascending or descending stairs
- Rising from a chair
- Weight-bearing activities
- Standing on one leg
- Turning in bed
- Depression, possibly due to the discomfort
How is pubic bone pain treated?
- Rest and Activity Modification: Reducing activities that exacerbate pain, such as standing for long periods, lifting heavy objects, or walking long distances.
- Pelvic Physiotherapy: A physiotherapist can provide exercises to strengthen the pelvic floor, abdominal, and hip muscles, and help stabilize the pelvic area. Manual therapy may also be used to realign the pelvis.
- Pain Relief: Over-the-counter pain medications such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) may be recommended. Always consult with a healthcare provider before taking any medication, especially if breastfeeding.
- Supportive Devices: Wearing a pelvic support belt can help stabilize the pelvis and reduce pain.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce pain and inflammation.
How can a pelvic health physiotherapist help with pubic bone pain?
A pelvic health physiotherapist can be of immense help with symphysis pubis dysfunction (SPD). A pelvic health physiotherapist can provide:
- Guidance on movement techniques for daily activities such as climbing stairs, bending, lifting, and feeding the baby.
- Education on gradually advancing exercises aimed at neuromuscular re-education, core stability, and proper posture.
- Hands-on therapy, including pelvic evaluations and muscle energy techniques to correct pelvic alignment.
- Evaluations to identify tissue dysfunction or lack of coordination.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Recovering from pubic bone pain after giving birth can be supported through targeted physiotherapy. If you’re looking for specialized care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can help you manage pain and regain strength and mobility through personalized treatment plans.
Let’s talk about stretches to do when pregnant. Engaging in stretching exercises during pregnancy can contribute to the elongation of your muscles and overall body flexibility, providing increased comfort whether you’re strolling through the grocery store, engaging in a workout, or simply relaxing. The soothing effects of stretching are particularly helpful during pregnancy, offering significant benefits to your body. Moreover, incorporating stretching into your routine at this stage can aid in preparing your muscles and joints for the challenges of labor in the future.

What are the benefits of stretching during pregnancy?
Stretching during pregnancy can offer several benefits for expectant mothers. However, it’s crucial to consult with a healthcare provider before starting any new exercise routine during pregnancy. Assuming that the healthcare provider gives the green light, here are some potential benefits of stretching during pregnancy:
- Improved Flexibility
- Reduced Muscle Tension
- Enhanced Circulation
- Relief from Discomfort
- Prevention of Muscle Strain
- Promotion of Relaxation
- Preparation for Labor
- Posture Improvement
- Emotional Well-being
- Better Sleep
What can I do to stretch safely when I am pregnant?
- First and foremost, check with your doctor or midwife to ensure that it is safe for your pregnancy.
- Warm-up
- Do gentle and controlled movements
- Avoid over-doing it
- Listen to your body
- Maintain good posture
- Use the right breathing techniques
- Hydrate
What are some of the stretches I can do when pregnant?




Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Performing safe stretches during pregnancy can help manage discomfort and improve flexibility. For personalized prenatal care and guidance, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can create tailored exercise plans to support your comfort and well-being throughout pregnancy.
March 8th marks International Women’s Day and Triangle Physiotherapy is proud to be able to empower women to advocate for themselves and their health needs.
Our goal is to encourage women to focus on their health, both, physical and mental. Build your healthcare team and schedule regular visits, in addition to exercising regularly and eating healthy.
Women’s Health and the Pelvic Floor
Women’s health is intricately connected to the well-being of the pelvic floor, a group of muscles, ligaments, and tissues supporting the uterus, bladder, and rectum. Maintaining a healthy pelvic floor is crucial for various functions, including urinary and bowel control, sexual function, and providing support during pregnancy. Pregnancy, childbirth, hormonal changes, and aging can impact the pelvic floor, leading to issues like incontinence, pelvic organ prolapse, and sexual dysfunction.
Maintaining a healthy lifestyle, proper posture, and seeking guidance from a pelvic health physiotherapist are essential for women’s pelvic floor health. Awareness and proactive care contribute to overall well-being, enabling women to lead active and fulfilling lives while addressing potential pelvic floor challenges.
What are the symptoms of Pelvic Floor Dysfunction?
Pelvic Floor Dysfunction (PFD) can manifest through various symptoms, which may vary in intensity and duration. Common signs of PFD include:
- Urinary Issues:
- Urinary incontinence: Involuntary leakage of urine.
- Frequent urination: The need to urinate more often than usual.
- Difficulty emptying the bladder: Struggling to fully release urine.
- Bowel Issues:
- Constipation: Difficulty passing stools or infrequent bowel movements.
- Straining during bowel movements: Experiencing difficulty while trying to have a bowel movement.
- Pelvic Pain:
- Pelvic pain or discomfort: Discomfort in the pelvic region, which may be persistent or intermittent.
- Pain during sexual intercourse: Discomfort or pain during sexual activity.
- Muscle Tension:
- Tight or spasming pelvic muscles: Increased muscle tension in the pelvic floor.
- Pelvic Organ Prolapse:
- The feeling of pressure or fullness in the pelvic area: Sensation of something bulging or descending into the vagina.
- Lower Back Pain:
- Chronic lower back pain: Discomfort or pain in the lower back region.
- Changes in Posture:
- Altered posture: Changes in the alignment of the spine and pelvis.
How a Pelvic Health Physiotherapist can help and what to expect?
A Pelvic Health Physiotherapist specializes in assessing and treating conditions related to the pelvic floor and surrounding areas. Here’s how they can help and what to expect during a session:
- Assessment:
- A thorough assessment of your medical history, pelvic health, and relevant symptoms.
- Physical examination, which may include internal and external assessments to evaluate the strength, flexibility, and coordination of the pelvic floor muscles.
- Education:
- Detailed explanation of pelvic anatomy and the role of pelvic floor muscles in various functions.
- Guidance on lifestyle factors, posture, and habits that may contribute to pelvic health issues.
- Pelvic Floor Exercises:
- Prescribing personalized pelvic floor exercises, to strengthen or relax specific muscles based on the assessment findings.
- Teaching proper technique and ensuring exercises are performed correctly.
- Manual Therapy:
- Hands-on techniques to release tension in the pelvic floor muscles or surrounding tissues.
- Myofascial release and trigger point therapy to address muscle knots or tightness.
- Biofeedback:
- Using biofeedback tools to provide real-time information about pelvic floor muscle activity.
- Assisting individuals in learning how to control and coordinate their pelvic floor muscles.
- Behavioral Strategies:
- Implementing behavioral strategies for managing and improving bladder and bowel function.
- Developing strategies for optimizing pelvic health during daily activities.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
On International Women’s Day, let’s celebrate the strength and resilience of women everywhere. For those seeking expert support for their health and wellness, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas are committed to empowering women through personalized care and treatment plans.
There are a lot of unknowns when going into labour and delivery. Whether it’s your first, second, or third child, every birth is very different, and daunting in its way. Some women hope to have a vaginal delivery, while others schedule or have emergency C-sections. Both forms of delivery are viable options however they can have different effects on your body postpartum. A cesarean section (C-section) can be life-saving for both the baby and mom. A common misconception is that a C-section is somehow “easier” but that is far from the truth. A C-section is a major surgery, that not only affects your abdominal muscles but also your pelvic floor. In this blog post, we will explore what C-sections are, their impact on the pelvic floor, and the benefits of pelvic floor physiotherapy for women who have had C-sections.
What is a C-section?
A C-section is a surgical procedure that involves delivering a baby through an incision made in the mother’s abdomen and uterus. It is usually performed either if the mother schedules a C-section, which may be for a variety of reasons, or in the case of an emergency. This may be done to save and protect the mother and baby. Some reasons for a C-section include a large baby, breech position, multiple pregnancies, maternal health conditions such as high blood pressure (preeclampsia), or labor not progressing as expected (dilation plateauing).
What impact does a C-Section have on the pelvic floor?
Many people assume that a C-section does not have any impact on the pelvic floor because the baby does not pass through the vagina. However, the pelvic floor can still be affected during a C-section. During the procedure, the surgeon may need to move the bladder and intestines to access the uterus, which can cause temporary weakness and stretching of the pelvic floor muscles. The stretching can also occur due to the weight of the baby pushing down on the pelvic floor during pregnancy. The procedure can also impact the nerves supplying the bladder and bowel, thereby reducing or completely removing your urge to pee. This altered sensation can improve over time, but may sometimes linger for years postpartum. In some cases, the sensation never comes back.
After the C-section, some women may experience pain and discomfort in the pelvic area, which can be exacerbated by activities such as lifting and carrying their newborn. This can lead to muscle tension and tightness, which can cause further issues down the line.
What are the benefits of pelvic floor physiotherapy after a C-section?
Pelvic floor physiotherapy is a specialized form of physical therapy that focuses on strengthening the pelvic floor muscles, improving their function and flexibility, and treating any pain or discomfort in the pelvic area. It can be very beneficial for women who have had a C-section, as it can help to address any issues that may have arisen due to the surgery.

How can healing and recovery be improved after a C-Section?
Pelvic floor physiotherapy can help to speed up the healing process after a C-section. It can help to reduce pain and swelling in the pelvic area, improve circulation, and promote tissue regeneration. It can also help to prevent the formation of scar tissue, which can cause discomfort and pain in the pelvic area. Keloid scarring is a type of scarring at the C section where the tissue raises and forms adhesions. This can be painful in some cases or uncomfortable and can impact sensation in the region.
- Address bladder and bowel issues
After a C-section, some women may experience bladder and bowel issues such as incontinence, urgency, or difficulty emptying their bladder or bowel. This may be a product of the nerves being impacted during the surgery or other factors. Pelvic floor physiotherapy can help to address these issues by strengthening the pelvic floor muscles and improving their function. It can also help to retrain the bladder and bowel to function properly and reduce incontinence.
- Improve sexual function
Many women may experience a decrease in sexual function after a C-section due to pain and discomfort in the pelvic area. This may be due to feelings of pelvic heaviness, perineum discomfort, or scar tissue. Pelvic floor physiotherapy can help to address these issues by reducing pain and discomfort and improving the function of the pelvic floor muscles. This can lead to an improvement in sexual function and overall sexual satisfaction.
Seeing a pelvic therapist post-C-section can also get you back to activities you love doing! This can include running, weight lifting, etc. There is no timeline for how quickly you should be recovering. Our bodies take time to heal postpartum. Your body is not broken, but working with a pelvic therapist can help you feel more like yourself again.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Seeing a pelvic floor physiotherapist after a C-section can be crucial for recovery and regaining strength. If you’re looking for specialized care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these locations can provide personalized post-C-section care to support your healing journey.
Triangle Physiotherapy in Mississauga is a full-service clinic that offers specialized services like Pelvic Health Physiotherapy. Our pelvic health physiotherapists are trained professionals who, apart from being experts in their field, are also empathetic individuals who understand the sensitive nature of the conditions that make people seek pelvic health physiotherapy.
Tell me more about your Mississauga Pelvic Health physiotherapists.

Our Mississauga Pelvic Health physiotherapists have training in the field of pelvic health physiotherapy and are committed to providing the best care to the community in Mississauga, be it new moms, women with prolapse or incontinence issues, pessary fittings, labour and delivery support, and more. We also have a pelvic health physiotherapist who is trained to help children. Our pelvic health physiotherapists are also able to help men with their pelvic health issues.
What type of conditions can a pelvic floor physiotherapist treat?
Some of the conditions treated by our Mississauga Pelvic Health physiotherapists are:
- Incontinence (urinary and fecal)
- Pelvic organ prolapse and pessary fittings
- Constipation
- Diastasis recti
- Vaginismus
- Pelvic pain
- Pelvic girdle pain during pregnancy and postpartum)
- Coccydynia (tailbone pain)
- Pudendal neuralgia
- Interstitial cystitis
- Female and Male Sexual dysfunction
- Prostatitis
- Rectal pain and dysfunction
- Irritable bowel syndrome
- Anal incontinence
- Anal fissures and fistulas
- Anal neuralgia
- Rectal prolapse
I just gave birth recently. How soon should I see a pelvic health physiotherapist
The pelvic floor muscles may get stretched or damaged during delivery, whether by C-Section or vaginal. This may cause issues of the pelvic floor that manifest as urinary or fecal incontinence, urinary urgency or frequency, pain during sexual activity, pelvic organ prolapse, pelvic pain, lower back pain, diastasis recti, or scar pain. Many of these issues can be addresed by pelvic health physiotherapy, however, our pelvic physiotherapists in Mississauga recommend waiting at least six weeks after delivery to allow the body time to heal from childbirth.
Can I speak to a pelvic health physiotherapist in Mississauga prior to booking a consultation?
We can certainly connect you with the best pelvic floor physiotherapist in Mississauga that can answer any questions you may have. Click here to book a discovery call.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Finding the right pelvic health physiotherapist is crucial for effective treatment and recovery. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists specialize in pelvic health, providing personalized treatment plans to help you achieve the best possible outcomes.”
What is vaginismus?
Vaginismus is a condition where the muscles around the vagina involuntarily contract, making it difficult or impossible to have vaginal penetration.
Do I have vaginismus?
If you answer yes to one or more of the following questions, you must book an appointment with a pelvic health physiotherapist to find out if you have vaginismus.
“Sex is so uncomfortable for me.”
“Why does it hurt to have sex? My doctor cannot find anything wrong with me.”
“Internal pelvic exams are a no for me – they are so painful.”
“My vagina feels like a fort that is impenetrable. I never realized it was vaginismus.”
“I used to have great sex, but now I close up—it burns and stings.”
“When my partner starts to move inside me, it hurts and we have to stop.”
“I don’t wear tampons because they don’t go in.”
What are the symptoms of vaginismus?
The symptoms may differ between younger and older women, emphasizing the significance of an accurate diagnosis and effective treatment for vaginismus.
The primary symptoms of vaginismus are:
- Sexual penetration seems physically impossible despite repeated attempts
- Difficulty inserting tampons from youth even after repeated attempts.
- Difficulty undergoing internal pelvic/gynecological exam
What are the causes of Vaginismus?

The exact causes of vaginismus can vary from person to person, and in many cases, the condition is multifactorial, meaning that multiple factors may contribute to its development. Here are some potential causes and contributing factors:
- Psychological factors: Emotional or psychological factors can play a significant role in vaginismus. Past traumatic experiences, such as sexual abuse, rape, or a history of painful intercourse, can contribute to the development of vaginismus. Anxiety, fear, guilt, or negative beliefs about sex can also trigger involuntary muscle contractions.
- Fear of pain or discomfort: Some individuals may develop vaginismus due to a fear of pain or discomfort during sexual intercourse. This fear can be based on previous painful experiences, cultural or religious beliefs, or misinformation about sex.
- Relationship issues: Difficulties in the relationship, such as poor communication, lack of trust, unresolved conflicts, or sexual problems, can contribute to the development or persistence of vaginismus. Emotional or physical distance between partners can create tension and anxiety during sexual activity.
- Cultural or religious factors: Cultural or religious beliefs and practices surrounding sex can influence a person’s perception of sexuality and contribute to the development of vaginismus. Upbringing that emphasizes guilt, shame, or negative attitudes towards sex can lead to involuntary muscle contractions during attempts at vaginal penetration.
- Lack of sexual education: Insufficient knowledge or understanding about sexual anatomy, arousal, and relaxation techniques can contribute to vaginismus. Inadequate sexual education may lead to misconceptions, anxiety, and fear surrounding sexual activity.
- Medical conditions or infections: Certain medical conditions, such as vaginal infections, urinary tract infections, endometriosis, or pelvic inflammatory disease, can cause pain during sex, leading to the development of vaginismus. Vaginal dryness or atrophy, often associated with menopause, can also contribute to discomfort and muscle tightness.
- Traumatic childbirth experiences: Some women may develop vaginismus after experiencing a traumatic childbirth, especially if they had a difficult or painful delivery. The association of vaginal penetration with the traumatic event can trigger involuntary muscle contractions.
What are the treatment options for vaginismus?
Pelvic health physiotherapy is a common treatment option for vaginismus. It involves a physical therapist working with the patient to help relax and strengthen the pelvic floor muscles.
Possible treatments include:
- Progressive pelvic floor muscle relaxation
- Biofeedback or muscle stimulation
- Yoga-based therapy
- Hip mobility work
- Lumbar spine mobility work
What can I expect during an assessment and treatment for vaginismus at Triangle Physiotherapy?
Assessment
The first step in pelvic health physiotherapy for vaginismus is usually an assessment of the patient’s pelvic floor muscles. This may involve an internal examination, but the therapist will always seek the patient’s consent and respect their comfort level.
Treatment
Once the assessment is complete, the therapist will develop a treatment plan tailored to the patient’s needs. This may involve exercises to strengthen the pelvic floor muscles or techniques to help the patient relax those muscles.
Techniques
One common technique used in pelvic health physiotherapy for vaginismus is called progressive muscle relaxation. This involves tensing and then releasing the pelvic floor muscles in a controlled way to help the patient become more aware of them and learn how to control them.
Another technique that may be used is biofeedback. This involves using sensors to monitor the activity of the pelvic floor muscles, which can help the patient learn to control them more effectively.
Overall, pelvic health physiotherapy can be an effective treatment for vaginismus, but it is important to work with a qualified physical therapist who has experience in this area. With patience, persistence, and the right guidance, many people with vaginismus can overcome their condition and enjoy fulfilling sexual relationships.
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you. Book an Appointment today!
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Managing vaginismus and improving intimacy is possible with the right physiotherapy care. Triangle Physiotherapy offers specialized pelvic health services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you overcome pain and enhance your intimate relationships through personalized treatment plans.”
Written by Roshni Ravi, Pelvic Health Physiotherapist.
Sexual health is an important aspect of overall health and well-being, but it’s not always an easy topic to talk about. Many women experience sexual health dysfunctions at some point in their lives, but they may feel embarrassed or ashamed to seek help by way of pelvic floor physiotherapy. There are currently large gaps in the sexual education provided at the elementary school level. Many sex ed classes are focused on birth control and how terrible periods are.
But there is not enough information, if any, on sexual health conditions and how to seek help. We’ve had a lot of conversations with patients about what they wish they had learned in sex-ed. In this blog post, we’ll explore some of the most commonly asked questions about sexual health dysfunctions in women and offer some tips for managing them.
What is pelvic floor physiotherapy?

Pelvic floor physiotherapy focuses on treating the muscles, ligaments, and connective tissues of the pelvic floor which is a group of muscles that form a supportive hammock-like structure at the base of the pelvis. They play a key role in maintaining continence, supporting the pelvic organs, and providing stability to the spine and hips.
Pelvic floor physiotherapy involves a range of exercises, manual therapy techniques, and education to help individuals with pelvic floor dysfunction. Common conditions that may benefit from pelvic floor physiotherapy include:
- urinary and fecal incontinence,
- pelvic pain,
- pelvic organ prolapse, and
- sexual dysfunction.
Why am I suffering from a low libido? Can pelvic floor physiotherapy help?
Many women experience a decrease in sexual desire at some point in their lives. This can be caused by a variety of factors, including stress, hormonal imbalances, and relationship issues. To manage low libido, it’s important to address any underlying issues and make self-care a priority. This can include:
- practicing stress-management techniques,
- getting enough sleep, and
- engaging in regular exercise.
Why does it hurt to have sex?
Painful intercourse, also known as dyspareunia, is a common sexual health dysfunction in women. It can be caused by a variety of factors, including vaginal dryness, infections, and hormonal imbalances. To manage painful intercourse, it’s important to work with a healthcare provider to identify the underlying cause and develop a treatment plan. This may include using:
- lubricants,
- treating infections,
- or using hormonal therapy.
I struggle to orgasm during sex, why does that happen?
Many women struggle to achieve orgasm during sexual activity which can be caused by a variety of factors, including, stress, relationship issues, and hormonal imbalances. To manage orgasmic dysfunction, it’s important to work with a healthcare provider or therapist to address any underlying issues and develop strategies for improving sexual function. This may include:
- practicing mindfulness or
- engaging in self-exploration techniques.
My vagina feels like a fort that is impenetrable. Why can I not have sexual intercourse?
Vaginismus is a condition in which the muscles of the vaginal wall contract involuntarily, making intercourse difficult or impossible. It can be caused by a variety of factors, including past trauma and anxiety. To manage vaginismus, it’s important to work with a healthcare provider or therapist to address any underlying issues and develop strategies for managing anxiety and relaxing the pelvic floor muscles.
What is vulvodynia? Do I need pelvic floor physiotherapy?
Vulvodynia is a chronic pain condition that affects the vulva, or external genitalia. It can cause burning, stinging, or itching sensations, and can make sexual activity painful or uncomfortable. To manage vulvodynia, it’s important to work with a healthcare provider to identify the underlying cause and develop a treatment plan. This may include:
- using topical creams or medications,
- practicing relaxation techniques, or
- seeing a pelvic health physiotherapist.
Help! I pee my pants!

Urinary incontinence is a common condition in which urine leaks from the bladder involuntarily. It can be caused by a variety of factors, including hormonal changes, pregnancy, and pelvic floor dysfunction. To manage urinary incontinence, it’s important to work with a healthcare provider or pelvic floor physiotherapist to develop a treatment plan. This may include:
- pelvic floor exercises,
- bladder training, or
- medications.
What are the signs of menopause?
Menopause can cause a variety of changes in sexual function, including vaginal dryness, decreased libido, and painful intercourse. To manage these changes, it’s important to work with a healthcare provider to develop a treatment plan. This may include:
- using hormonal therapy,
- vaginal moisturizers, or
- engaging in regular sexual activity to maintain pelvic floor health.
Where can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
In conclusion…
Many women experience sexual health dysfunctions at some point in their lives, but they may feel embarrassed or ashamed to seek help. It’s important to remember that sexual health is an important aspect of overall health and well-being, and it’s important to prioritize it in your self-care routine. If you’re experiencing any issues related to sexual function, don’t hesitate to talk to your healthcare provider or a therapist about your options. Remember, there is help!
Click here to book your consultation with one of our knowledgeable and compassionate pelvic health physiotherapists.
“Pelvic floor physiotherapy is essential for improving sexual health and overall well-being. Triangle Physiotherapy offers specialized pelvic health services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can help you address pelvic floor issues and enhance your sexual health through personalized treatment plans.”