When it comes to women’s health, two conditions often mentioned together are Polycystic Ovary Syndrome (PCOS) and Endometriosis. While both can impact fertility and overall well-being, they are distinct conditions with different causes, symptoms, and treatments. The pelvic health physiotherapists at Triangle Physiotherapy help us break down the key differences to help you better understand them.
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects how the ovaries function. It is one of the most common endocrine disorders among women of reproductive age.
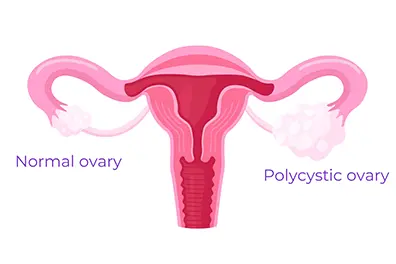
Common Symptoms of PCOS:
- Irregular or Absent Periods: Due to hormonal imbalances, women with PCOS often experience infrequent or prolonged menstrual cycles.
- Excess Hair Growth and Acne: Elevated levels of androgens (male hormones) can lead to hirsutism (excess facial and body hair), acne, and even hair thinning on the scalp.
- Insulin Resistance: Many women with PCOS struggle with insulin resistance, which can increase the risk of type 2 diabetes.
- Ovarian Cysts: Despite its name, not all women with PCOS have cysts on their ovaries, but some may develop multiple small fluid-filled sacs.
What is Endometriosis?
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside of it, leading to inflammation, scarring, and pain.
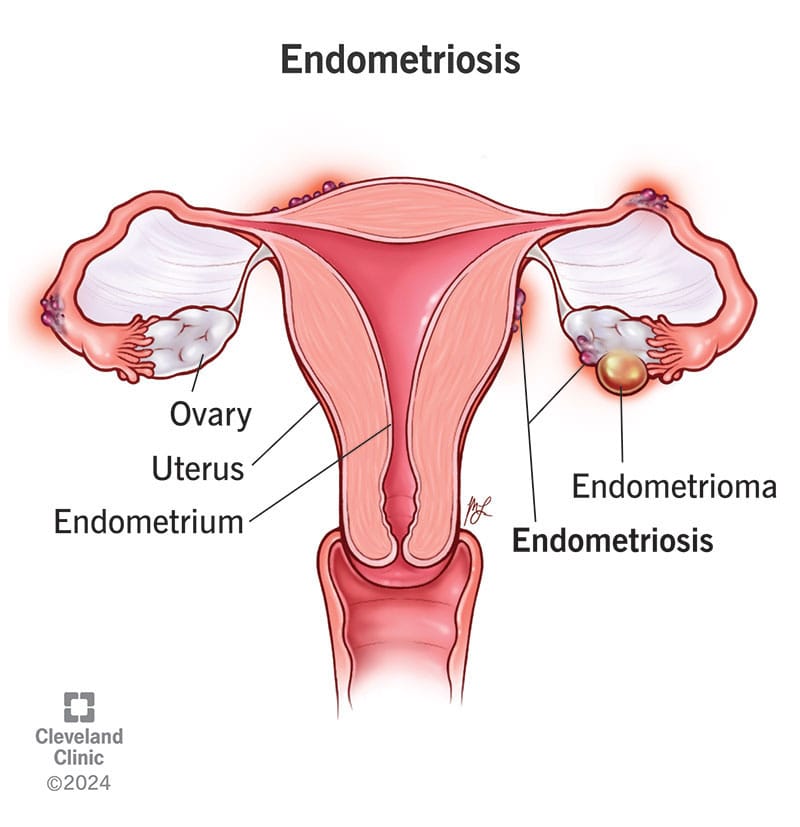
Common Symptoms of Endometriosis:
- Severe Menstrual Cramps: One of the hallmark symptoms of endometriosis is intense pelvic pain that can start before and last beyond the menstrual cycle.
- Heavy Periods: Women with endometriosis often experience unusually heavy menstrual bleeding.
- Pain During Intercourse: Pain during or after sex is a common complaint due to the presence of endometrial-like tissue outside the uterus.
- Chronic Pelvic Pain: Many women with endometriosis experience ongoing pelvic discomfort, even outside their periods.
Key Differences Between PCOS and Endometriosis
| Feature | PCOS | Endometriosis |
|---|---|---|
| Cause | Hormonal imbalance | Endometrial-like tissue growing outside the uterus |
| Periods | Irregular or absent | Heavy and painful |
| Pain | Not always present | Severe pelvic pain |
| Fertility Impact | May cause ovulation issues | May lead to scarring and blockages |
| Hormonal Symptoms | Excess androgens (acne, hair growth) | Usually no androgen-related issues |
How Are PCOS and Endometriosis Treated?
Since these conditions have different causes, their treatments also vary:
- PCOS Treatment: May involve hormonal birth control, lifestyle changes, insulin-sensitizing medications (like Metformin), and fertility treatments if pregnancy is desired.
- Endometriosis Treatment: Can include pain management (NSAIDs), hormonal therapy (such as birth control or GnRH agonists), and in severe cases, surgery to remove endometrial-like tissue.
The Bottom Line
Both PCOS (Polycystic Ovary Syndrome) and Endometriosis are complex conditions that need personalized treatment. If you notice symptoms of either, it’s important to talk to a healthcare provider to get the right diagnosis and treatment plan.
Along with medical care, adding Physiotherapy Oakville can also help. Physiotherapy can ease pelvic pain, improve movement, and reduce muscle tension caused by these conditions. It supports your overall well-being and helps you feel better over time.
By combining medical advice and physiotherapy, you can manage symptoms more effectively and improve your quality of life.
💬 Do you or someone you know struggle with these conditions? Let’s continue raising awareness and supporting women’s health! 💙
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Menopause is a fact of life for people who menstruate – periods need to stop eventually! So why don’t we talk about menopause more often? Even when we do talk about it, there seem to be a lot of misconceptions and myths. It’s time to bust them wide open!
1. Menopause symptoms are mostly hot flashes and mood swings
Though it may be true that hot flashes and mood swings are common symptoms of menopause, it is so much more than that! In fact, comprehensive lists of menopausal symptoms have over 100 different symptoms! Our naturopathic doctor and pelvic health physiotherapists at Triangle Physiotherapy can help educate you on the symptoms and their natural management.
2. Menopausal symptoms are unpreventable and a fact of life for all women

Some women have their periods stop without experiencing any symptoms at all! But even if you’re not one of those lucky people, there are things you can do to help this transitional time in your life to be more manageable. Talk to your naturopathic doctor to find out what you can do!
3. During peri-menopause, your periods always get lighter and farther apart
Though this may be true that eventually your periods become lighter and farther apart, it often doesn’t start that way. Many women find that when menopause begins, it’s actually the exact opposite of this. Periods can become more frequent and heavier before they eventually peter out.
4. The only mood changes that happen during menopause are irritability and mood swings
This is one of the most important myths for us to clarify. Yes, it’s true that irritability, anger, and mood swings are all potential symptoms of menopause. But anxiety and depression are part of what can happen during menopause, too. Instead of thinking of a menopausal woman as “cranky and short-tempered”, keep in mind that they may be going through anxiety and depression. Check up on menopausal women, and ensure they have the mental health support they often need at this time.
5. Menopause only happens after age 50
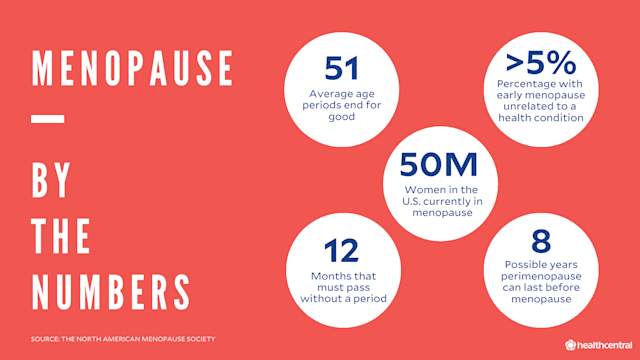
The most common age for menopause to happen is 50, but there is a lot of variance with this. In fact, some women can even go into menopause in their 30’s!
6. A hysterectomy always causes menopause
If you have a total hysterectomy, it is true that you will enter menopause post-surgery. But if your ovaries are not removed, then this isn’t the case. You would go through menopause naturally, and this could happen many years after your hysterectomy.
7. An IUD can cause you to skip over menopause
IUD’s have no impact on when you will go through menopause. What they can do, however, is help to manage some of the bleeding symptoms that can occur along with menopause.
8. Menopause marks the end of a woman’s sex life
Absolutely not! Women can have healthy sex lives well beyond menopause! Some symptoms of declining estrogen levels, such as lower libido and vaginal dryness, may make intercourse more difficult. However, there are natural options that can help to manage these symptoms to make intercourse more pleasurable for you. Be sure to speak to a naturopathic doctor if you would like to explore more of these options. Our pelvic health physiotherapists can also help you navigate the effects menopause can have on your sex life.
9. Menopause lasts a couple of years
It’s usually much longer than this. In fact, menopausal symptoms can begin up to 10 years before your periods actually stop!
10. Men go through menopause too
Nope. You may have heard of “andropause” or “manopause”, which refer to when testosterone levels decline in men. However, this testosterone decline happens very slowly, over several years. In menopause, the hormonal fluctuations are more drastic and happen much more quickly. This is why menopause can cause uncomfortable symptoms.
We hope this helped to clear up some of the common myths out there about menopause. If you have any further questions about menopause or women’s health, reach out to our naturopathic doctor at Triangle Physiotherapy and book an appointment today!
Pelvic girdle pain (PGP) is a common condition that affects the joints and ligaments in the pelvic area, often leading to discomfort in the lower back, hips, and pelvic region. It can occur during pregnancy, after childbirth, or as a result of injury or underlying musculoskeletal issues. PGP can significantly impact daily activities and overall well-being.
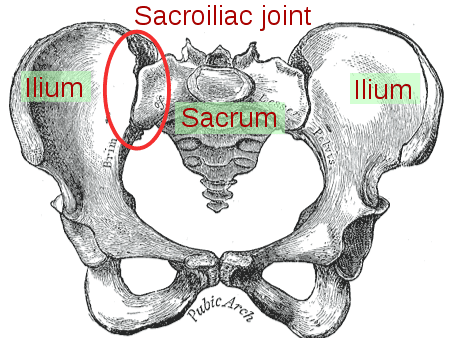
The pelvic health physiotherapists at Triangle Physiotherapy can help with pelvic girdle pain by doing a thorough assessment and designing a treatment plan to help with your recovery.
Symptoms of Pelvic Girdle Pain
- Pain in the lower back, hips, or pelvic area
- Discomfort that worsens with movement or weight-bearing activities
- Stiffness in the pelvis, especially after sitting or resting
- Difficulty with activities like walking, climbing stairs, or turning in bed
- Sensations of instability or “wobbliness” in the pelvic region
Treatment for Pelvic Girdle Pain at Triangle Physiotherapy Mississauga
At Triangle Physiotherapy, our experienced physiotherapists are dedicated to helping you manage pelvic girdle pain through a tailored treatment plan that may include:
Comprehensive Assessment
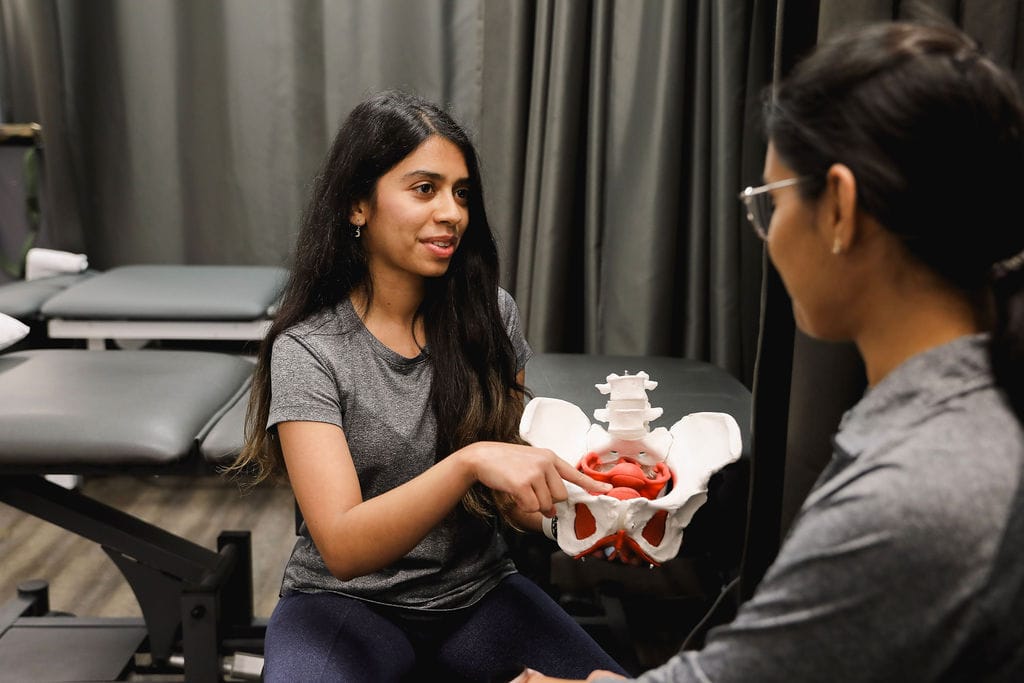
A detailed evaluation of your symptoms, medical history, and physical condition to create a personalized treatment approach.
Pain Management
Effective strategies for pain relief, including manual therapy, soft tissue techniques, and modalities like heat or ice therapy.
Targeted Exercises

A program of gentle exercises to strengthen the pelvic floor and core muscles, improve stability, and enhance flexibility.
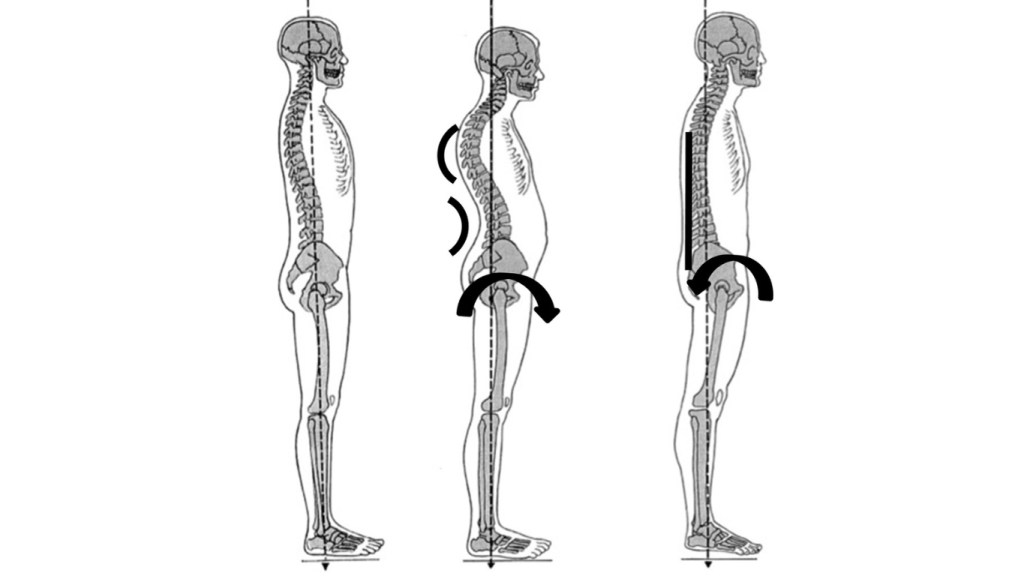
Postural and Movement Education for Pelvic Girdle Pain
Guidance on proper body mechanics and techniques to reduce strain on the pelvis during daily activities.
Supportive Devices
Recommendations for supportive belts or braces to help stabilize the pelvic area and alleviate discomfort.
Lifestyle Modifications
Advice on activity adjustments and ergonomics to help manage pain and prevent flare-ups, including strategies for safe movement and positioning.
FAQs
Can pelvic girdle pain be cured?
While pelvic girdle pain may not have a definitive cure, our goal at Triangle Physiotherapy is to help you manage your symptoms effectively and improve your quality of life.
Is surgery necessary for pelvic girdle pain?
Surgery is rarely needed for PGP. Most cases can be successfully managed with non-surgical treatments and lifestyle modifications.
How can I prevent pelvic girdle pain from worsening?
Maintaining good posture, avoiding excessive strain, and practicing gentle stretching can help prevent symptoms from worsening.
If you are experiencing pelvic girdle pain, don’t hesitate to contact Triangle Physiotherapy for a consultation. Our team is committed to helping you find relief and regain your comfort in daily life.
Pelvic Physiotherapy, a specialized form of physiotherapy, plays a vital role in helping men regain control, improve function, and enhance their quality of life after prostate cancer treatment.
Prostate cancer is one of the most common cancers affecting men worldwide. While advances in medical treatments like surgery, radiation, and chemotherapy have improved survival rates, the recovery process can often come with a range of physical challenges. One area that is often overlooked is the pelvic health of men post-prostate cancer treatment.
Get in touch with us at Triangle Physiotherapy, we have physiotherapists that are trained in cancer rehabilitation as well as pelvic health. We can help you recover from the side effects of cancer treatment and regain your quality of life.
Prostate Cancer and Its Impact
Prostate cancer typically develops in the prostate gland, a small organ located below the bladder. Treatment options can include surgery (prostatectomy), radiation therapy, hormone therapy, or chemotherapy. While these treatments are effective in managing cancer, they often lead to side effects, particularly in the pelvic region. Common issues that arise after prostate cancer treatment include urinary incontinence, erectile dysfunction, pelvic pain, and difficulty with bowel control.
These conditions can significantly affect a man’s physical and emotional well-being, leading to decreased quality of life, social withdrawal, and even depression. This is where pelvic rehabilitation comes in.
What Is Pelvic Rehabilitation?
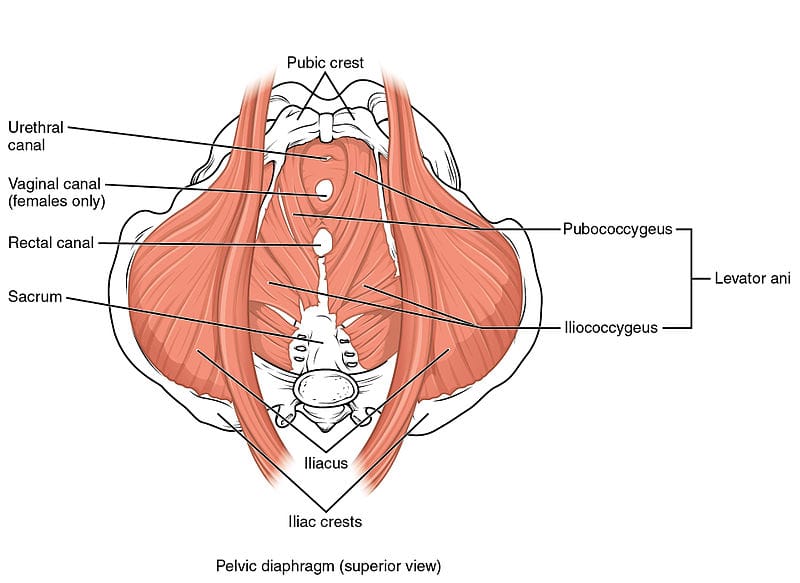
Pelvic rehabilitation is a specialized form of physical therapy that focuses on restoring function to the pelvic floor muscles and addressing issues related to the pelvic organs. These muscles support the bladder, bowel, and reproductive organs. For men recovering from prostate cancer, pelvic rehabilitation can help restore strength, control, and coordination in the pelvic region, leading to improvements in urinary control, sexual function, and overall pelvic health.
A trained pelvic health physiotherapist will assess the patient’s specific symptoms and develop a personalized treatment plan. The goal is to reduce discomfort, improve mobility, and enhance the patient’s ability to resume normal daily activities.
How Pelvic Health Physiotherapy Helps After Prostate Cancer Treatment
1. Improving Urinary Control
Urinary incontinence is a common side effect after prostate cancer surgery or radiation. The pelvic floor muscles, which help control urine flow, can become weakened or damaged during treatment. Pelvic rehabilitation techniques, including exercises to strengthen these muscles, can help men regain bladder control and reduce the frequency of leaks. Kegel exercises and electrical stimulation are often used to retrain the pelvic floor muscles and improve urinary continence.
2. Enhancing Sexual Function
Erectile dysfunction (ED) is another common concern after prostate cancer treatment. Pelvic rehabilitation can help address ED by improving blood flow to the penis and strengthening the pelvic floor muscles that contribute to sexual function. Manual therapy, muscle retraining, and pelvic exercises can also help men regain confidence and improve their sexual health.
3. Relieving Pelvic Pain
Pelvic pain or discomfort can persist after treatment, especially if nerve tissue was affected during surgery or radiation. Manual therapy techniques such as myofascial release, soft tissue mobilization, and gentle stretching can help relieve pain, improve flexibility, and reduce tension in the pelvic area.
4. Improving Bowel Function
For some men, prostate cancer treatment can lead to bowel dysfunction, such as constipation or fecal incontinence. Pelvic rehabilitation techniques can help restore normal bowel function by strengthening the muscles involved in bowel control and improving coordination between the pelvic floor and the digestive system.
The Importance of Early Intervention
The sooner men begin pelvic rehabilitation after prostate cancer treatment, the better the outcomes. Early intervention can help prevent long-term complications, reduce recovery time, and improve overall quality of life. It’s important to consult a pelvic health physiotherapist who specializes in post-cancer recovery for a personalized treatment plan.
Call us today to book an appointment and learn about how we can help you.
Vaginismus is a condition often misunderstood and sometimes left undiagnosed due to lack of awareness or stigma. Lets demystify vaginismus by addressing the most frequently asked questions, including symptoms, causes, diagnosis, and effective treatments. Whether you’re seeking help for yourself or someone you know, understanding vaginismus is the first step toward finding relief and support. The pelvic health physiotherapists at Triangle Physiotherapy can help you overcome this condition and regain your quality of life.
1. What Is Vaginismus?
Vaginismus is a condition where involuntary muscle contractions occur around the vaginal opening, making penetration painful or even impossible. This muscle response can be triggered by physical or psychological factors and often interferes with intimate activities, tampon use, and even gynecological exams.
2. What Are the Symptoms?
- Pain or discomfort during penetration
- Burning, stinging, or tightness in the pelvic area
- Difficulty with vaginal penetration, such as tampon use or gynecological exams
- Anticipation of pain before intimacy due to past experiences
3. What Causes Vaginismus?
Previous painful intercourse or other experiences that create a conditioned response in the muscles
- Anxiety or fear of pain
- Trauma or past experiences, such as sexual abuse
- Certain medical conditions, infections, or hormonal imbalances
- Lack of awareness or knowledge about the condition
4. How common is it?
Although exact prevalence is hard to determine, vaginismus is not uncommon. Many people don’t seek help due to embarrassment or misconceptions, but it is estimated that a significant number of people with vaginas experience some form of pelvic pain or vaginismus at some point.
5. What is the difference between primary and secondary Vaginismus?
Primary Vaginismus
• sexually inexperienced
• penetration problem apparent at first attempt
• sexual penetration may seem physically impossible
• unconsummated couples
• sometimes difficulty inserting tampons/undergoing pelvic exam
Secondary Vaginismus
• sexually experienced
• previously normal sex life
• ongoing vaginal tightness, discomfort, pain with intercourse
• usually precipitated by medical condition, menopause, traumatic event, childbirth, surgery, etc.
• sometimes difficulty with pelvic exam
6. Is there a treatment for Vaginismus?
Vaginismus can be a challenging condition to manage. While exercises and stretches done at home are helpful, additional support may be necessary.
That’s where pelvic floor physiotherapy comes in.
A pelvic health physiotherapist can help you to:
- Offer personalized guidance on pelvic floor exercises for managing vaginismus.
- Identify any pelvic floor dysfunctions.
- Learn specific exercises to strengthen the pelvic floor muscles.
- Practice targeted stretches to relax essential areas.
- Address symptoms such as incontinence, constipation, pelvic pain, prolapse, and others.

While vaginismus can be a challenging condition, there is hope and help available. Seeking support from qualified professionals and understanding treatment options can lead to meaningful improvement. Remember, vaginismus is a common issue, and addressing it openly is the first step toward reclaiming comfort and confidence. Book an appointment with one of our pelvic health physiotherapists in Mississauga, Oakville or Toronto to get help today!
Here are links to studies and articles that discuss the prevalence of vaginismus and the effectiveness of pelvic floor therapy as a treatment:
- Reissing et al.’s study on pelvic floor physical therapy in lifelong vaginismus, which provides insights into patient experiences and therapy outcomes, including reductions in pain and improved quality of life. This research suggests that pelvic floor therapy can be effective, particularly with a tailored approach involving manual techniques and education. You can access it hereRead by QxMD.
- For further context on the prevalence of vaginismus and other sexual dysfunctions, look into studies by Miller et al., which highlight pelvic floor disorders in U.S. women and treatment options.
Pregnancy is an incredible journey, but it can also bring a variety of physical changes and challenges. One of the best ways to support your body during this time is by seeing a pelvic health physiotherapist.
The good news is that the pelvic health physiotherapists at Triangle Physiotherapy are experienced and trained to help you to smoothly navigate your pregnancy journey.
Here are eight compelling reasons to consider this specialized care throughout your pregnancy.
1. Alleviate Discomfort and Pain

Pregnancy can lead to discomfort and pain in various areas, particularly the lower back, hips, and pelvis. A pelvic health physiotherapist can assess your posture, movement patterns, and muscle imbalances. They can provide targeted exercises and techniques to relieve pain, helping you feel more comfortable as your body changes.
2. Improve Core and Pelvic Floor Strength
Strong core and pelvic floor muscles are essential during pregnancy. A pelvic health physiotherapist can guide you through safe exercises that strengthen these areas, preparing your body for the physical demands of labor and delivery. This foundation can also help reduce the risk of complications during childbirth.
3. Enhance Posture and Body Mechanics
As your pregnancy progresses, your center of gravity shifts, often leading to changes in posture. Poor posture can contribute to discomfort and pain. A pelvic health physiotherapist can teach you proper body mechanics and alignment strategies, helping you maintain good posture throughout your pregnancy and beyond.
4. Manage Incontinence Issues
Many pregnant women experience urinary incontinence due to the added pressure on the bladder and hormonal changes. A pelvic health physiotherapist specializes in pelvic floor dysfunction and can provide exercises to strengthen the pelvic floor, helping to manage and reduce incontinence issues during and after pregnancy.
5. Prepare for Labor and Delivery
A pelvic health physiotherapist can help you prepare your body for labor and delivery through specific exercises and techniques. They can teach you breathing strategies, positions for labor, and relaxation techniques, empowering you with tools to facilitate a smoother birthing experience.
6. Support Postpartum Recovery
While the focus is often on pregnancy, the postpartum period is equally important. A pelvic health physiotherapist can help you transition back to your pre-pregnancy activities by addressing any lingering pain, pelvic floor dysfunction, or core weakness. Early intervention can lead to better recovery and long-term health.
7. Educate on Body Changes
Understanding the physical changes your body undergoes during pregnancy can be incredibly empowering. A pelvic health physiotherapist provides education on what to expect, including changes to your pelvic floor and core muscles. This knowledge can help alleviate fears and build confidence as you navigate your pregnancy and postpartum recovery.
8. Personalized Care and Support
Every pregnancy is unique, and a pelvic health physiotherapist offers personalized care tailored to your specific needs. They take the time to understand your individual concerns, lifestyle, and goals, ensuring that you receive the most effective treatment. This supportive environment fosters trust and encourages open communication about any issues you may encounter.
Book Your Appointment Today!
Seeing a pelvic health physiotherapist is a very important part of your pregnancy journey. Book your appointment as soon as you have confirmation of your pregnancy to make sure you have a supportive healthcare practitioner alongside you to guide you through this new and exciting phase in your life.
Triangle Physiotherapy has eight locations in the GTA offering pelvic health physiotherapy. Call us today!
Ref: https://pelvichealthsolutions.ca/knowledge-base/pregnancy
Understanding the Pelvic Floor and Bladder Health
The pelvic floor consists of a group of muscles that support the bladder, bowel, and uterus (in women). These muscles are responsible for controlling urination, bowel movements, and sexual function. When weakened, common issues such as incontinence, pelvic organ prolapse, and sexual dysfunction can arise. Understanding the role of these muscles is the first step toward strengthening them.
Strengthening you pelvic floor can lead to a stress-free lifestyle. Schedule an appointment with one of the pelvic health physiotherapists at Triangle Physiotherapy.
Key functions of the Pelvic Floor:
- Support of pelvic organs
- Control of bladder and bowel movements
- Sexual health and satisfaction
Benefits of Strengthening the Pelvic Floor
By keeping your pelvic floor muscles strong, you can experience several benefits beyond preventing common issues like incontinence. Some of these include:
- Enhanced bladder control: Strong muscles prevent leakage during activities like sneezing, laughing, or exercising.
- Better posture: The pelvic floor is connected to core muscles, and strengthening it can improve your overall posture.
- Improved sexual function: Strengthening the pelvic muscles can lead to better sexual sensations and enhanced satisfaction.
- Postpartum recovery: New mothers can benefit from a stronger pelvic floor to regain muscle strength after childbirth.
Lifestyle Changes for Pelvic Health

Incorporating small but impactful changes in your daily routine can go a long way in improving pelvic floor and bladder health. Here are a few simple yet effective lifestyle adjustments:
- Stay hydrated but mindful of fluids: Drink plenty of water throughout the day, but reduce intake of caffeinated or carbonated drinks that can irritate the bladder.
- Maintain a healthy weight: Excess weight puts pressure on the pelvic floor, weakening it over time. Maintaining a healthy BMI can reduce strain.
- Eat a fiber-rich diet: Consuming enough fiber prevents constipation, which can stress the pelvic floor.
- Quit smoking: Chronic coughing caused by smoking weakens the pelvic floor muscles over time.
Strengthening your pelvic floor and bladder is a journey that requires consistency and dedication. By incorporating simple exercises, making mindful lifestyle changes, and considering professional or holistic support, you can enjoy better control, confidence, and overall well-being. Remember, prevention is always better than cure, so taking steps to support your pelvic health now will benefit you in the long run.
This lifestyle guide offers a comprehensive approach to strengthening your pelvic floor and bladder. By following these tips and making small adjustments, you’ll be well on your way to a healthier and stronger pelvic floor.
Contact us today to book an appointment with one of our pelvic health physiotherapists at either of our 8 locations and get your recovery journey started.
Pregnancy is a beautiful journey, but it can come with its fair share of discomforts, one of which is pelvic pain. For many expectant mothers, pelvic pain is a common issue that can impact their daily lives. Understanding the causes and exploring effective treatments can help manage this discomfort and ensure a smoother pregnancy experience. At Triangle Physiotherapy, our trained and experienced pelvic health physiotherapists are committed to helping you with your pelvic pain so that you can get back your quality of life and do the things you love.

Here’s a detailed look at the causes of pelvic pain during pregnancy and the available treatment options.
Causes of Pelvic Pain During Pregnancy
1. Hormonal Changes
During pregnancy, the body undergoes significant hormonal changes, particularly with the increase in relaxin—a hormone that helps the pelvis become more flexible in preparation for childbirth. While this is necessary for delivery, it can also lead to joint instability and pelvic pain as the ligaments and joints become looser and less stable.
2. Growing Uterus
As the pregnancy progresses, the growing uterus exerts pressure on the pelvic region. This pressure can cause discomfort and pain, especially as the uterus expands and shifts its position. The added weight can also put strain on the pelvic joints and muscles.
3. Pelvic Girdle Pain (PGP)
Pelvic Girdle Pain, also known as Symphysis Pubis Dysfunction (SPD), is a condition where the pelvic joints become painful and unstable. This can occur when the ligaments that support the pelvic bones become too relaxed and unable to support the growing weight. PGP can cause pain in the pelvic region, hips, and lower back.
4. Round Ligament Pain
Round ligament pain is another common cause of pelvic discomfort during pregnancy. The round ligaments, which support the uterus, stretch as the uterus grows. This stretching can cause sharp or aching pain in the lower abdomen or groin area, especially with sudden movements.
5. Previous Injuries or Conditions
Women with a history of pelvic injuries or pre-existing conditions like endometriosis or fibroids may experience exacerbated pelvic pain during pregnancy. The added physical changes can aggravate these pre-existing issues.
Schedule an appointment with one of the pelvic health physiotherapists at Triangle Physiotherapy and get your recovery journey started.
Prevention
Preventing pelvic pain during pregnancy involves a combination of lifestyle adjustments and self-care practices:
- Exercise Regularly: Engage in low-impact exercises like walking, swimming, or prenatal yoga to strengthen the muscles around the pelvis and improve flexibility.
- Maintain Good Posture: Pay attention to your posture, especially when sitting or standing for extended periods. Proper posture can alleviate unnecessary strain on the pelvic region.
- Use Supportive Gear: Consider using a maternity support belt or pelvic support belt to help stabilize the pelvis and reduce pain.
- Avoid High-Risk Movements: Try to avoid activities that involve sudden movements or heavy lifting, which can exacerbate pelvic pain.
Progressive Resistance
Progressive resistance training involves gradually increasing the intensity of exercises to build strength and stability. For pregnant women experiencing pelvic pain, this approach can be adapted to:
- Strengthen Core Muscles: Exercises that target the core, such as modified planks or gentle pelvic tilts, can help support the pelvic region and reduce pain.
- Strengthen Pelvic Floor Muscles: Kegel exercises can help strengthen the pelvic floor muscles, providing better support to the pelvic organs and reducing pain.
Neuromuscular Exercises
Neuromuscular exercises focus on improving coordination and muscle control, which can be beneficial for managing pelvic pain:
- Balance Training: Exercises that enhance balance and stability, such as gentle balance exercises on a stability ball, can help reduce the risk of falls and support the pelvic region.
- Proprioceptive Exercises: Activities that improve body awareness and spatial orientation can help in managing pelvic discomfort and improving overall function.
Mobility Exercises
Mobility exercises aim to enhance the range of motion and flexibility of the pelvic joints and surrounding muscles:
- Hip Flexor Stretches: Gentle stretching of the hip flexors can help alleviate tension and discomfort in the pelvic area.
- Pelvic Rocking: Performing gentle pelvic rocking exercises can help relieve pressure on the pelvis and improve comfort.
Safety Tips
Consult a Healthcare Provider: Always consult with your healthcare provider before starting any new exercise or treatment regimen to ensure it is safe for your specific situation.
- Listen to Your Body: Pay attention to your body’s signals and avoid pushing through pain. Modify or stop activities that exacerbate discomfort.
- Seek Professional Help: If pelvic pain becomes severe or persistent, consider seeking help from a physiotherapist who specializes in prenatal care.
Pelvic pain during pregnancy can be challenging, but understanding its causes and exploring effective treatments can provide significant relief. By incorporating preventative measures, progressive resistance training, neuromuscular exercises, and mobility exercises, expectant mothers can manage pelvic pain more effectively. Always prioritize safety and consult with healthcare professionals to tailor an approach that suits your individual needs. With the right care and support, you can navigate the journey of pregnancy with greater comfort and ease.
Pregnancy is a remarkable journey filled with joy and anticipation. However, it also brings various physical challenges, one of the most common being back pain. This blog explores the causes of pregnancy back pain and how physiotherapy can provide relief. We’ll delve into the benefits of pelvic health physiotherapy in Mississauga and the holistic approach it offers to expecting mothers.

Causes of Pregnancy Back Pain
Hormonal Changes
During pregnancy, the body produces a hormone called relaxin, which helps to loosen the ligaments in the pelvic area to prepare for childbirth. While necessary, this increased flexibility can lead to instability and back pain.
Weight Gain
The additional weight gained during pregnancy puts extra strain on the spine. This added pressure can cause discomfort and pain, particularly in the lower back.
Postural Changes
As the baby grows, the center of gravity shifts forward, leading to changes in posture. This can result in muscle strain and back pain as the body adjusts to the new alignment.
Stress
Emotional stress can cause muscle tension in the back, leading to pain. It’s essential to manage stress effectively during pregnancy to minimize its impact on physical health.
How Physiotherapy Can Help with Pregnancy Back Pain
Personalized Treatment Plans
Physiotherapy in Mississauga offers personalized treatment plans tailored to the specific needs of pregnant women. These plans focus on alleviating back pain through targeted exercises and techniques.
Pain Relief Techniques
Physiotherapists use a variety of techniques to relieve pregnancy back pain, including manual therapy, massage, and specific exercises designed to strengthen the back and core muscles.
Pelvic Health Physio in Mississauga
Pelvic health physiotherapy is a specialized branch of physiotherapy that focuses on the pelvic floor muscles, which play a crucial role during pregnancy and childbirth. Pelvic health physiotherapists in Mississauga helps in:
- Strengthening Pelvic Floor Muscles: Exercises to enhance the strength and function of these muscles.
- Improving Posture: Guidance on maintaining proper posture to reduce back strain.
- Breathing Techniques: Techniques to manage pain and improve overall comfort during pregnancy.
Benefits of Physiotherapy for Pregnancy Back Pain
Reducing Pain and Discomfort
Regular physiotherapy sessions can significantly reduce back pain and discomfort, improving the quality of life for expecting mothers.
Enhancing Mobility
Physiotherapy helps maintain and improve mobility, making daily activities easier and more comfortable.
Preparing for Childbirth
Pelvic physio in Mississauga not only alleviates back pain but also prepares the body for childbirth by strengthening the pelvic floor muscles and improving overall physical readiness.
Postpartum Recovery
Physiotherapy continues to be beneficial postpartum, aiding in the recovery process and helping new mothers regain their strength and mobility.
What do I do next?
Find the Right Physiotherapist in Mississauga

When looking for physiotherapy in Mississauga, it’s essential to find a qualified and experienced physiotherapist who specializes in pregnancy and pelvic health. Our Locations in Mississauga have trained and experienced pelvic health physiotherapists with advanced training in pelvic health including Labour and Delivery Prep.
Pregnancy back pain is a common but manageable condition. With the right approach, such as physiotherapy in Mississauga, expecting mothers can find relief and improve their overall well-being. Pelvic health physiotherapists at Triangle Physiotherapy in Mississauga offers specialized care that addresses the unique challenges of pregnancy, providing a holistic approach to pain management and preparation for childbirth. By incorporating physiotherapy into their prenatal care routine, pregnant women can enjoy a more comfortable and healthy pregnancy journey.
Triangle Physiotherapy has 2 locations in Mississauga to help you with your pregnancy-related back pain:
Triangle Physiotherapy Square One
Triangle Physiotherapy Erin Mills
“At Triangle Physiotherapy, we have multiple locations across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our clinics are dedicated to providing specialized care for pregnancy-related back pain, ensuring that every expecting mother receives the best possible treatment.”
An episiotomy is a surgical incision made in the perineum (the patch of skin between the vaginal opening and the anus) during childbirth, is a common procedure to aid in a smoother delivery. Despite its benefits, an episiotomy can lead to discomfort, pain, and complications in postpartum recovery. This blog explores how a pelvic health physiotherapist can play a crucial role in managing and alleviating post-episiotomy issues, ensuring a healthier recovery for new mothers.
Our trained and experienced Pelvic Health Physiotherapists in Mississauga can make a significant difference to your recovery after child-birth.

Why is an episiotomy performed during delivery?
An episiotomy may be performed by the obstetrician during delivery for various reasons:
1. Prevent Severe Tearing
2. Facilitate a Faster Delivery
In situations where a rapid delivery is required for the safety of the baby or mother, an episiotomy can speed up the process. This is particularly crucial in cases of:
- Fetal Distress: If the baby shows signs of distress, such as an abnormal heart rate, a quick delivery becomes essential. An episiotomy can help expedite the birth, reducing the risk of complications for the baby.
- Prolonged Labor: When labor is not progressing, and the baby is not moving down the birth canal as expected, an episiotomy can aid in accelerating the delivery.
3. Assisted Deliveries
Episiotomies are more commonly performed during assisted deliveries involving instruments like forceps or vacuum extractors.
4. Shoulder Dystocia
Shoulder dystocia occurs when the baby’s shoulder becomes lodged behind the mother’s pelvic bone during delivery. This can be a critical situation requiring immediate intervention. An episiotomy can provide additional room for the baby’s shoulder to be maneuvered and delivered safely.
5. Large Baby
When a baby is larger than average, delivering them vaginally can be challenging. An episiotomy may be performed to create more space, reducing the risk of severe tearing and facilitating a smoother delivery.
6. Previous Pelvic Surgery or Scarring
What is the role of a pelvic health physiotherapist in recovering from an Episiotomy?
A pelvic health physiotherapist specializes in the rehabilitation of pelvic floor muscles. They are trained to address issues related to childbirth, including those arising from an episiotomy. At Triangle Physiotherapy Mississauga, our pelvic health physiotherapists are highly trained in helping new mothers navigate their post-partum recovery.
- Pain Management and Scar Tissue Mobilization
- Pelvic Floor Rehabilitation
- Bladder and Bowel Function Improvement
- Addressing Incontinence: Many women experience urinary or fecal incontinence after an episiotomy. Pelvic health physiotherapists can help manage these issues through targeted exercises and lifestyle modifications.
- Diet and Hydration Advice: Proper diet and hydration are essential for optimal bladder and bowel function. Physiotherapists offer valuable advice on nutrition that supports recovery.
- Posture and Mobility
- Improving Posture: Poor posture can exacerbate pelvic pain. Physiotherapists help new mothers correct their posture, reducing strain on the pelvic floor and aiding in overall recovery.
- Safe Return to Activity: Guiding new mothers on safely returning to physical activities is vital. Physiotherapists create gradual exercise plans to ensure a safe and effective return to daily activities and fitness routines.
- Emotional Support and Counseling
- Addressing Psychological Aspects: The postpartum period can be emotionally challenging. Physiotherapists provide emotional support and can refer patients to mental health professionals if needed, ensuring a holistic approach to recovery.
- Building Confidence: Encouraging words and positive reinforcement from physiotherapists can boost new mothers’ confidence in their recovery journey.
If you have had an episiotomy during delivery, contact us to book an appointment to see one of our pelvic health physiotherapists in Mississauga to get started on the road to recovery.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 2 convenient locations in Mississauga that offer pelvic health:
Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Recovering from an episiotomy can be challenging, but with the help of a pelvic health physiotherapist, you can regain your strength and confidence. Triangle Physiotherapy offers specialized care at multiple locations across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team is here to support you every step of the way.”