Pelvic Health physiotherapists advocate the importance of educating individuals about their pelvic health. They are often asked by patients if an internal exam is necessary. Many patients refrain from seeking help for pelvic health issues because of the fear of internal examination. While internal exams are not a must, they can be very helpful to pelvic health physiotherapists in determining the condition of the pelvic floor.
What is an Internal Pelvic Exam?
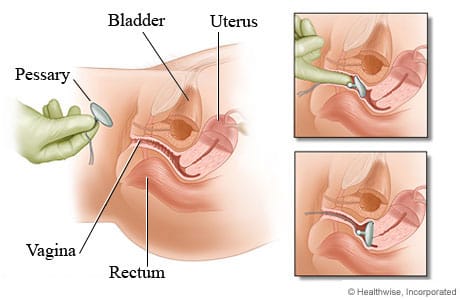
A pelvic floor assessment, which may or may not include an internal pelvic exam, entails a pelvic health physiotherapist examining the pelvic floor muscles, tissues, and organs by inserting a gloved hand into the vagina or rectum. This examination is crucial for assessing the well-being and performance of the pelvic floor, allowing for the detection of any possible problems or issues.
Why is an internal pelvic exam important?
- Detailed Assessment of Pelvic Floor Muscles: An internal pelvic exam allows the physiotherapist to assess the tone, strength, flexibility, and coordination of the pelvic floor muscles. This information is crucial in developing an accurate understanding of the patient’s pelvic health.
- Identification of Muscle Imbalances: Through internal palpation, a physiotherapist can identify any muscle imbalances or asymmetries in the pelvic floor. This helps in tailoring the treatment plan to address specific issues, such as hypertonic (overactive) or hypotonic (underactive) muscles.
- Assessment of Pelvic Organ Function: Internal examination enables the physiotherapist to assess the function of pelvic organs, such as the bladder, uterus, and rectum. This is important in cases where dysfunction or weakness in the pelvic floor muscles may be contributing to issues such as urinary incontinence or pelvic organ prolapse.
- Evaluation of Connective Tissues and Nerves: The internal exam allows the physiotherapist to assess the condition of connective tissues, ligaments, and nerves in the pelvic region. Dysfunction in these structures can contribute to pelvic pain and other symptoms, and the internal exam helps in identifying such issues.
- Assessment of Trigger Points and Tenderness: The physiotherapist can identify trigger points and areas of tenderness within the pelvic floor muscles. This information is crucial in designing a targeted treatment plan, which may include manual therapy techniques to release muscle tension.
- Feedback on Exercise Performance: During an internal pelvic exam, the physiotherapist may guide the patient through specific exercises to assess the effectiveness of pelvic floor muscle contractions. Real-time feedback helps the patient learn proper muscle engagement and control.
- Patient Education and Empowerment: The internal exam provides an opportunity for the physiotherapist to educate the patient about their pelvic floor anatomy, function, and any specific issues identified during the assessment. This empowers the patient to actively participate in their treatment plan and make lifestyle changes that support pelvic health.

Do I have to have an internal exam during a pelvic health assessment?
It’s important to note that internal pelvic exams are conducted with the patient’s informed consent, and physiotherapists ensure a comfortable and respectful environment during the assessment. The goal is to provide comprehensive care and address the specific needs of individuals experiencing pelvic health issues. That being said, if you are not comfortable being internally examined, please let your physiotherapist know before the start of your assessment.
How do I prepare for an internal pelvic exam?
Preparing for an internal pelvic exam involves a combination of physical and mental preparation. It’s essential to communicate openly with your pelvic health physiotherapist and follow their instructions. Here are some general guidelines to help you prepare:
Comfortable Clothing: Wear comfortable, easy-to-remove clothing. You may be asked to undress from the waist down, so wearing a skirt or loose pants can be convenient.
Relaxation Techniques: Practice relaxation techniques such as deep breathing to help ease anxiety and tension. Relaxing your pelvic muscles can make the exam more comfortable.
Communicate with your Physiotherapist: Inform your pelvic health physiotherapist about any concerns, fears, or past traumatic experiences related to pelvic exams. They can adjust their approach and provide additional support.
Ask Questions: Feel free to ask any questions you may have about the procedure. Knowing what to expect can help alleviate anxiety.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Understanding the need for an internal exam during a pelvic health assessment can help you make informed decisions about your care. If you’re looking for specialized support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can provide comprehensive pelvic health assessments tailored to your comfort and needs.
There are a lot of unknowns when going into labour and delivery. Whether it’s your first, second, or third child, every birth is very different, and daunting in its way. Some women hope to have a vaginal delivery, while others schedule or have emergency C-sections. Both forms of delivery are viable options however they can have different effects on your body postpartum. A cesarean section (C-section) can be life-saving for both the baby and mom. A common misconception is that a C-section is somehow “easier” but that is far from the truth. A C-section is a major surgery, that not only affects your abdominal muscles but also your pelvic floor. In this blog post, we will explore what C-sections are, their impact on the pelvic floor, and the benefits of pelvic floor physiotherapy for women who have had C-sections.
What is a C-section?
A C-section is a surgical procedure that involves delivering a baby through an incision made in the mother’s abdomen and uterus. It is usually performed either if the mother schedules a C-section, which may be for a variety of reasons, or in the case of an emergency. This may be done to save and protect the mother and baby. Some reasons for a C-section include a large baby, breech position, multiple pregnancies, maternal health conditions such as high blood pressure (preeclampsia), or labor not progressing as expected (dilation plateauing).
What impact does a C-Section have on the pelvic floor?
Many people assume that a C-section does not have any impact on the pelvic floor because the baby does not pass through the vagina. However, the pelvic floor can still be affected during a C-section. During the procedure, the surgeon may need to move the bladder and intestines to access the uterus, which can cause temporary weakness and stretching of the pelvic floor muscles. The stretching can also occur due to the weight of the baby pushing down on the pelvic floor during pregnancy. The procedure can also impact the nerves supplying the bladder and bowel, thereby reducing or completely removing your urge to pee. This altered sensation can improve over time, but may sometimes linger for years postpartum. In some cases, the sensation never comes back.
After the C-section, some women may experience pain and discomfort in the pelvic area, which can be exacerbated by activities such as lifting and carrying their newborn. This can lead to muscle tension and tightness, which can cause further issues down the line.
What are the benefits of pelvic floor physiotherapy after a C-section?
Pelvic floor physiotherapy is a specialized form of physical therapy that focuses on strengthening the pelvic floor muscles, improving their function and flexibility, and treating any pain or discomfort in the pelvic area. It can be very beneficial for women who have had a C-section, as it can help to address any issues that may have arisen due to the surgery.

How can healing and recovery be improved after a C-Section?
Pelvic floor physiotherapy can help to speed up the healing process after a C-section. It can help to reduce pain and swelling in the pelvic area, improve circulation, and promote tissue regeneration. It can also help to prevent the formation of scar tissue, which can cause discomfort and pain in the pelvic area. Keloid scarring is a type of scarring at the C section where the tissue raises and forms adhesions. This can be painful in some cases or uncomfortable and can impact sensation in the region.
- Address bladder and bowel issues
After a C-section, some women may experience bladder and bowel issues such as incontinence, urgency, or difficulty emptying their bladder or bowel. This may be a product of the nerves being impacted during the surgery or other factors. Pelvic floor physiotherapy can help to address these issues by strengthening the pelvic floor muscles and improving their function. It can also help to retrain the bladder and bowel to function properly and reduce incontinence.
- Improve sexual function
Many women may experience a decrease in sexual function after a C-section due to pain and discomfort in the pelvic area. This may be due to feelings of pelvic heaviness, perineum discomfort, or scar tissue. Pelvic floor physiotherapy can help to address these issues by reducing pain and discomfort and improving the function of the pelvic floor muscles. This can lead to an improvement in sexual function and overall sexual satisfaction.
Seeing a pelvic therapist post-C-section can also get you back to activities you love doing! This can include running, weight lifting, etc. There is no timeline for how quickly you should be recovering. Our bodies take time to heal postpartum. Your body is not broken, but working with a pelvic therapist can help you feel more like yourself again.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Seeing a pelvic floor physiotherapist after a C-section can be crucial for recovery and regaining strength. If you’re looking for specialized care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these locations can provide personalized post-C-section care to support your healing journey.
Triangle Physiotherapy in Mississauga is a full-service clinic that offers specialized services like Pelvic Health Physiotherapy. Our pelvic health physiotherapists are trained professionals who, apart from being experts in their field, are also empathetic individuals who understand the sensitive nature of the conditions that make people seek pelvic health physiotherapy.
Tell me more about your Mississauga Pelvic Health physiotherapists.

Our Mississauga Pelvic Health physiotherapists have training in the field of pelvic health physiotherapy and are committed to providing the best care to the community in Mississauga, be it new moms, women with prolapse or incontinence issues, pessary fittings, labour and delivery support, and more. We also have a pelvic health physiotherapist who is trained to help children. Our pelvic health physiotherapists are also able to help men with their pelvic health issues.
What type of conditions can a pelvic floor physiotherapist treat?
Some of the conditions treated by our Mississauga Pelvic Health physiotherapists are:
- Incontinence (urinary and fecal)
- Pelvic organ prolapse and pessary fittings
- Constipation
- Diastasis recti
- Vaginismus
- Pelvic pain
- Pelvic girdle pain during pregnancy and postpartum)
- Coccydynia (tailbone pain)
- Pudendal neuralgia
- Interstitial cystitis
- Female and Male Sexual dysfunction
- Prostatitis
- Rectal pain and dysfunction
- Irritable bowel syndrome
- Anal incontinence
- Anal fissures and fistulas
- Anal neuralgia
- Rectal prolapse
I just gave birth recently. How soon should I see a pelvic health physiotherapist
The pelvic floor muscles may get stretched or damaged during delivery, whether by C-Section or vaginal. This may cause issues of the pelvic floor that manifest as urinary or fecal incontinence, urinary urgency or frequency, pain during sexual activity, pelvic organ prolapse, pelvic pain, lower back pain, diastasis recti, or scar pain. Many of these issues can be addresed by pelvic health physiotherapy, however, our pelvic physiotherapists in Mississauga recommend waiting at least six weeks after delivery to allow the body time to heal from childbirth.
Can I speak to a pelvic health physiotherapist in Mississauga prior to booking a consultation?
We can certainly connect you with the best pelvic floor physiotherapist in Mississauga that can answer any questions you may have. Click here to book a discovery call.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Finding the right pelvic health physiotherapist is crucial for effective treatment and recovery. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists specialize in pelvic health, providing personalized treatment plans to help you achieve the best possible outcomes.”
Getting the most out of your physiotherapy appointment involves effective communication, preparation, and active participation.

Here are some tips to help you make the most of your physiotherapy session:
- Be Prepared:
- Write down your symptoms, concerns, and questions beforehand.
- Note any changes in your condition since your last appointment.
- Bring relevant medical reports, imaging results, or a list of medications you’re taking.
- Arrive Early:
- Arriving a few minutes early will give you time to complete any necessary paperwork and relax before your session.
- Effective Communication:
- Clearly describe your symptoms, their onset, severity, and any factors that worsen or alleviate them.
- Be honest about your lifestyle, activities, and habits that could impact your condition.
- Ask questions if you don’t understand something. Your physiotherapist is there to help you.
- Set Clear Goals:
- Discuss your goals with your physiotherapist. What do you want to achieve through physiotherapy? This could be pain relief, improved mobility, or functional goals.
- Follow Instructions:
- Listen carefully to the advice and instructions provided by your physiotherapist.
- Follow the recommended exercises, stretches, or home-care routines diligently.
- Ask Questions:
- Don’t hesitate to ask questions about your condition, treatment plan, exercises, or any concerns you might have.
- Understand Your Treatment Plan:
- Make sure you understand your treatment plan, including the goals, expected outcomes, and duration of treatment.
- Take Notes:
- Jot down key points, exercises, or recommendations during the session so you can refer back to them later.
- Feedback:
- Provide feedback to your physiotherapist about your progress and any changes you’ve noticed.
- Be Patient:
- Understand that progress may take time. Don’t get discouraged if you don’t see immediate results.
- Follow Up:
- Schedule follow-up appointments as recommended by your physiotherapist to monitor your progress and make adjustments to your treatment plan.
- Hygiene and Attire:
- Wear comfortable clothing that allows easy access to the area being treated.
- Maintain good hygiene, especially if your session involves physical contact.
- Engage Actively:
- Participate actively during the session. Follow your physiotherapist’s instructions and give your best effort during exercises.
Remember, your physiotherapist is there to help you achieve your goals and improve your health and well-being. By being proactive, engaged, and open in your communication, you can maximize the benefits of your physiotherapy appointments.
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Maximizing the benefits of your physiotherapy appointment is essential for a successful recovery. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists are committed to helping you achieve your health goals with personalized care and guidance.”
Physiotherapy is an evidence-based regulated healthcare profession that aims to maintain, restore and improve your function after disease or injury, so you can get back to doing what you love and enjoy an injury-free lifestyle that doesn’t hold you back.
Physiotherapists are primary healthcare professionals with a significant role in health promotion and treatment of injury and disease.
They combine their in-depth knowledge of the body and how it works with specialized hands-on clinical skills to assess, diagnose and treat symptoms of illness, injury, or disability.

What is the average cost of physiotherapy near me?
The cost of physiotherapy depends on the appointment type and setting.
An initial assessment at a private practice typically costs between $120 to $150 in the Greater Toronto Area. Follow-ups at a private practice may cost between $80 and $110 per session. The numbers will vary based on the location of the clinics and various other factors.
What are the contributing factors to the cost of physiotherapy near me?
The cost of physiotherapy services is driven by factors such as:
- Type of service provided
- Length of session
- Physiotherapist’s specialty (Pelvic Health, Vestibular, and Concussion Rehab)
- The geographical location of the clinic
- Insurance reimbursement rates
Does insurance cover Physiotherapy?
Insurance plans may cover physiotherapy but every insurance plan is different, so, it may be prudent to check the details of your plan. Some questions to ask your insurance provider are:
- What is the annual coverage limit for physiotherapy?
- Is there a per-visit maximum, if any?
- Are there any required co-payments?
- Is the fee covered 100%?
- Is there a deductible?
How much will my physiotherapy treatments cost in total?
The cost of physiotherapy depends on the type and complexity of your injury or condition that is being treated as well as the treatment plan that your physiotherapist designs for you while keeping in mind your goals for recovery.
Why do I need to be treated by a registered physiotherapist?
It is of utmost importance to ensure that you are being seen by a registered Physiotherapist because behind every registered Physiotherapist are years of academic and clinical training as well as extensive knowledge of all the systems of the human body. At our physiotherapy center, we guarantee that every single physiotherapist we have is registered with the College of Physiotherapists of Ontario and will take excellent care of you.
Who do I speak to about the cost of physiotherapy near me?
Contact our patient care coordinator team at any of our eight locations. They will help you with any insurance-related questions you may have as well as match you with a physiotherapist best suited for your injury or condition.
Is it worth it to see a physiotherapist?
Seeing a physiotherapist can be very beneficial in many situations. Physiotherapy is a healthcare profession that focuses on improving and restoring physical function and mobility. Whether it’s addressing a specific injury, managing chronic pain, or enhancing overall physical well-being, a physiotherapist can provide valuable guidance and treatment.
Joining Physiotherapy Oakville offers you access to a team of skilled professionals who utilize evidence-based practices to tailor treatments to your specific needs. Scientific studies have shown that physiotherapy can significantly improve recovery times and physical outcomes. By becoming a part of Physiotherapy Oakville, you benefit from personalized care plans that enhance your physical health, help manage pain effectively, and support your overall well-being, ensuring you achieve the best possible outcomes.
Seein a physiotherapist costs less than what you would pay in terms of compromising your quality of life and being in pain.
Seeing a physiotherapist can help you:
- Get back to your favourite activity or sport
- Recover from an injury or surgery
- Get educated on how to exercise safely, manage painful episodes, improve your posture and more.
- Return to work after an injury
- Rehabilitate after an automobile accident
- Recover after childbirth
- and more.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Understanding the cost of physiotherapy is important for planning your treatment. Triangle Physiotherapy offers high-quality care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our clinics provide transparent pricing and personalized treatment plans to ensure you receive the best care at a cost that works for you.”
Our physiotherapy center in Mississauga is located at 4188 Living Arts Drive, Unit 3, Mississauga L5B0H7. The closest intersection is Living Arts Drive and Burnhamthorpe Road, in the Square One Mall area.

My health is very important to me so I would like to choose the best physiotherapy clinic near me. I have heard great things about you. What makes you the best physiotherapy clinic in Mississauga?
Our patients have told us many times that we offer the best physiotherapy service in Mississauga because from the second they step inside our physio clinic in Mississauga until the end of every session, our physiotherapists at our Mississauga clinic provide them with a one-on-one quality service they deserve.
I went to a physiotherapy clinic near me which I was told was the best physiotherapy clinic in Mississauga but I found out the physiotherapist who was treating me was not registered. Are all the physiotherapists at your Mississauga clinic registered?
Yes, all the physiotherapists at our Mississauga clinic are registered. We go through a rigorous vetting process for applicants when we hire our professionals, as we want to provide the best expertise and service to our patients.
I recently moved to Mississauga and am in search of a physiotherapist near me who could provide me with excellent care like my previous physiotherapist. Which physiotherapist in Mississauga would you recommend I see?
Our physiotherapists in Mississauga are all registered, highly qualified and will provide you with quality care that will exceed your expectations. We have all their profiles on our website for your review. You may also call us and we can discuss your condition further so we may recommend the physiotherapist at our physiotherapy centre in Mississauga, who we feel would best fit your condition.
What kind of services do you offer at your physio clinic in Mississauga and what makes you different from all the other clinics that offer physiotherapy services near me?
Our physiotherapy center in Mississauga offers:
- Physiotherapy,
- Pelvic Health,
- Pediatric Pelvic Health,
- Vestibular Rehab,
- Massage therapy,
- Naturopathy,
- Acupuncture, Dry Needling
- Chiropractic services.
The physio clinic near me does not provide direct billing. I would only like to go to a clinic that can do direct billing for me. Does your physiotherapy center do direct billing or do I need to pay upfront for the physiotherapy services?
Yes, our physio clinic in Mississauga offers direct billing to most insurance companies to save you time and provide you with a stress free experience.
I have vertigo and am in search of a Vestibular physiotherapist near me. Do you have a Vestibular physiotherapist in your Mississauga location?
Yes, we have a Vestibular physiotherapist at our Mississauga location. Here at the physiotherapy clinic in Mississauga, our vestibular physiotherapist will conduct a thorough assessment to establish the root of your problem and design a customised program of balance exercises to help resolve your symptoms.
If you have Vertigo (BPPV) this can be treated with a simple head maneuver called the Epley’s maneuver.
Your treatment will include exercises and education about your condition.
Who would benefit from pelvic floor physiotherapy?
Pelvic health physiotherapy is the therapeutic treatment of all disorders affecting the pelvis and pelvic floor. From incontinence to prolapse, pelvic pain, or constipation, there is growing evidence that physiotherapy can alleviate, and in many cases cure these symptoms. Pelvic physiotherapists are experienced in treating men and women.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Finding the closest physiotherapy clinic in Mississauga is essential for convenient access to care. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy Etobicoke, Physiotherapy Oakville, Physiotherapy North York, Physiotherapy Toronto, Physiotherapy Lawrence Park, Physiotherapy Queens Quay, Physiotherapy Erin Mills, Physiotherapy Mississauga, and Liberty Village. Our clinics are strategically located to provide you with the highest quality physiotherapy services close to home.”
When choosing a physiotherapy clinic, it’s essential to find a clinic that has physiotherapists that meet your specific needs and can provide high-quality care.
Which is the closest Physiotherapy clinic near me in the Erin Mills area of Mississauga?
Our physiotherapy center at Erin Mills in Mississauga is located in the Arc Condominiums at 2520 Eglinton Avenue, W, on the SECOND Floor. The closest intersection is Erin Mills Parkway & Eglinton Ave W across from Erin Mills Town Center and Credit Valley Hospital.
Is there a highly qualified physiotherapist at your physio clinic in Mississauga who you would recommend I see?
Our physiotherapy center in Mississauga has highly qualified professional physiotherapists with many years of experience. We have physiotherapists with FCAMPT designation, which is the highest certification in manual therapy. Our physiotherapists are also trained in specialties like dry needling, pelvic health and cancer rehab.
We also have a team of highly skilled professionals including physiotherapists, massage therapists, acupuncturists, chiropractic doctors as well as naturopathic doctors. You are welcome to read their profiles on our website or call us for more information.
Do all your physiotherapy centers offer physiotherapy services, massage services, and chiropractic services?
Yes, all of our clinics offer the following services:
- Physiotherapy
- Pelvic Floor Physiotherapy
- Acupuncture and Dry Needling
- Vestibular Rehab Therapy
- Chiropractic
- Massage therapy
- Naturopathic Medicine
Are the fees for all physiotherapy services, massage services and chiropractic services the same in all your physiotherapy centers?
Yes, our fees at all eight locations are the same for all physiotherapy services.
I have tried a physio clinic near me but I wasn’t satisfied with the service they have provided me and I would like to try another physio clinic near me. How many clinics do you have in Mississauga?
We have two locations in Mississauga, Triangle Physiotherapy by Erin Mills Mall and Triangle Physiotherapy by the Square One Shopping Centre.
I have been searching for physiotherapy clinics near me that offer Shockwave physiotherapy service, does your clinic offer this?
Yes, our physiotherapy clinic in Erin Mills has shockwave therapy as well as other Physiotherapy modalities available to provide the best treatment possible for our patients.
I recently found out that the physiotherapy clinic near me has registered physiotherapists at their physiotherapy clinic. I would like to move to a physio clinic near me, are all your physiotherapists in Erin Mills registered?
Yes, all our physiotherapists at the Erin Mills clinic are registered physiotherapists and highly qualified.
I have seen many physiotherapists in Erin Mills but I have yet to see improvement in my condition. Are all your physiotherapists in your Physiotherapy clinic in Mississauga registered and am I able to choose which registered physiotherapist I would like to book with?
All our physiotherapists will take excellent care of you, but you’re more than welcome to choose which physiotherapist you would like to book with. You may check their profiles on our website and inform us who you would like to book with when you request an appointment.
Many Physiotherapy centers claim to be the best physiotherapy clinic in Mississauga but I have personally heard from a friend who I trust that you are indeed the best physiotherapy clinic in Mississauga. How do I book an appointment?
You may call, email, or send us a message on the chat feature on our website, and we will gladly help you book an appointment at a time that is most convenient for you. You may also submit a booking request by clicking here.
What is physiotherapy?

Orthopaedic Physiotherapy is the assessment and treatment of all musculoskeletal conditions (including back and neck pain, fractures, and sprains) caused by repetitive “wear and tear,” sports injuries, falls, car accidents, or surgeries. The problem can be acute or chronic. Manual therapy, education, active exercise therapy, soft tissue release, and joint mobilizations are the focus of treatments at Triangle Physiotherapy in Erin Mills, to allow you to regain strength, flexibility, balance, and full movement and function.
Our physio clinic Erin Mills, Mississauga has qualified and expert physiotherapists to help you with any musculoskeletal, vestibular, or pelvic health issues.
How is physiotherapy beneficial and what conditions can it treat?
Physiotherapists apply their extensive scientific knowledge of anatomy and physiology to:
- Assess, diagnose, and treat injuries & conditions that affect people of all ages and social groups
- Assist a patient to prevent injury in the workplace or on the sports field
- Promote healthier lifestyles for all
By choosing Triangle Physiotherapy in Mississauga you can rest assured that your physiotherapist is a registered professional with the highest qualifications. This means that they have undergone rigorous scientific training and that they continue to stay up to date with current practices.
Physiotherapy can help a wide variety of conditions including the following:
- Sports injuries
- Posture & movement correction
- Low back pain
- Neck pain & Whiplash
- Headaches
- Shoulder pain
- Ankle sprains
- Knee pain
- Shin splints
- Groin & hip injuries
- Muscular corks/contusions/tears
- Osteoarthritic/degenerative joint pain and more.
What are the different types of physiotherapy?
There are different types of specializations in physiotherapy, some of which are listed below:
- Orthopedic Physiotherapy
- Pelvic Floor Physiotherapy
- Vestibular Physiotherapy
- Cancer Rehab Physiotherapy
- Neurological Physiotherapy
- Sports Physiotherapy
- Pediatric Physiotherapy
Who would benefit from pelvic floor physiotherapy?
Pelvic Floor Physiotherapists are specifically trained in diagnosing and treating conditions associated with the pelvic floor muscles. This usually refers to muscles involved in reproductive and digestive processes in the body. While these muscles are in close proximity to muscles commonly involved in lower back problems, and sometimes even overlap, physiotherapy treatment for the lower back involves significantly different techniques.
Men, women, and children with pelvic floor dysfunction can benefit from pelvic floor physiotherapy.
What can I expect from my pelvic floor physiotherapy appointment?
When attending an appointment at our Mississauga Pelvic Health clinic for the first time, you will be asked to fill in a new patient information form prior to your initial visit. We highly recommend filling out your forms at home through our user-friendly patient portal, the link for which will be sent to you as soon as you book your session.
We will endeavor to make your first visit to our clinic a comfortable experience.
At your initial consultation, your physiotherapist will:
- Conduct a thorough examination including history taking and a physical assessment, which may include an internal examination of your pelvic area;
- Give you a working diagnosis of your condition;
- Education
- Treatment Plan
The initial visit will be an hour long and follow-up visits can range from 30 minutes to an hour depending on the amount of time your physiotherapist needs with you.
Who performs acupuncture at your physiotherapy clinic in Mississauga, Erin Mills location?
At Triangle Physiotherapy Erin Mills, acupuncture treatment is carried out by our physiotherapists, who have undergone specialized training. They use acupuncture or dry needling as part of their physiotherapy treatment to reduce pain and stimulate the healing process.
In addition to our physiotherapists, our acupuncturist also has specialized training in needling and can help with conditions such as:
- Pain
- Stress & anxiety
- Sleep & insomnia
- Allergies
- Respiratory issues
- Women’s health
- Dizziness & Vertigo
- Asthma
- Weakness & Fatigue
What conditions can vestibular physiotherapy be beneficial for?
Vestibular rehabilitation is a specialized form of therapy primarily aimed at reducing symptoms of vertigo, dizziness, visual disturbance, and/or imbalance. Research suggests that it is beneficial, safe & effective.
Vestibular rehabilitation can benefit patients of any age and can be effective for long-standing symptoms, although it is advisable to start as soon as possible.
Treatment plans for vestibular conditions depend on the presenting symptoms, medical history, diagnostic test results, and physical examination. Treatment will be goal focused and progressive and you will be provided with exercises to complete independently on a regular basis.
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you. Book an Appointment today!
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Finding the closest physiotherapy clinic is important for convenient and effective care. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our clinics are easily accessible, providing high-quality physiotherapy to help you achieve your health goals.”
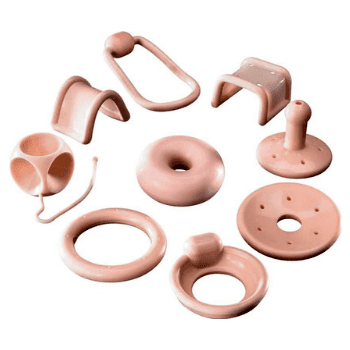
A pessary is a medical device designed to be inserted into the vagina to provide support for pelvic organs or to treat certain gynecological conditions. It is typically made of silicone or plastic and comes in various shapes and sizes to accommodate different needs.
What is the purpose of a pessary?
The purpose of a pessary is to support the pelvic organs and alleviate symptoms of pelvic organ prolapse or urinary incontinence. It helps to hold the organs in place and improve their function.
Who might need a pessary?
Doctors commonly recommend pessaries for women who experience pelvic organ prolapse, which happens when the pelvic organs, such as the uterus, bladder, or rectum, descend from their normal positions. Pessaries can also manage stress urinary incontinence, a condition where involuntary leakage of urine occurs during activities that increase abdominal pressure, such as coughing or lifting.
How is a pessary inserted?
During a pelvic examination, a healthcare provider usually inserts the pessary. The healthcare provider folds the pessary and inserts it into the vagina. Once inside, the pessary opens up and provides support to the pelvic organs. The specific method of insertion may vary depending on the type of pessary being used.
How many appointments will I need?
Typically, you will require a minimum of three appointments to ensure that your pessary is doing what it needs to.
Do I need a doctor’s note to get fitted for a pessary?
No, you don’t need a doctor’s note to see the pelvic health physiotherapist, however, if your insurance requires one for reimbursement then you need to get one. Also if the therapist decides after assessing you, that you will benefit from a pessary then you will be provided with a clearance letter that will need to be signed by your family dr or your ob-gyn prior to fitting.
Are pessary fitting appointments covered by insurance?
Yes, the services are covered under physiotherapy coverage.
Does Triangle Physiotherapy do pessary fittings?
This service is currently provided at 4 of our locations in Toronto and Mississauga.
a. King West
c. North York
d. Mississauga
Who provides pessary fittings at Triangle Physiotherapy?
Some of our pelvic health physiotherapists at our Toronto Pessary Clinics and Mississauga Pessary Clinic are trained to do pessary fittings and insertions. Schedule an appointment to see if a pessary can help you.
How does the process work?
When you come in for your initial assessment, the therapist will do a pelvic assessment as well as take the measurement for the pessary. At your 2nd appointment, you will be fitted with a pessary device. You will have a follow-up appointment after 2-3 weeks to check if everything is ok and that there is no redness or infection. The pelvic physiotherapists will also explain to you how to take it out and clean it.
How can I find a pelvic health physiotherapist who does pessary fittings near me?
We have 4 locations with pelvic health physiotherapists that do pessary fittings to help you.
- Pessary Fittings North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health, Mississauga Pessary Fitting – Triangle Physiotherapy Mississauga
- Toronto Pessary Clinic – Triangle Physiotherapy King West
- Uptown Toronto Pessary Clinic – Triangle Physiotherapy Lawrence Park
A pessary can be an effective non-surgical option for managing pelvic organ prolapse, and combining it with pelvic floor physiotherapy can enhance results. If you are looking for professional physiotherapy services to support your pelvic health, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and personalized treatment plans to help manage prolapse symptoms and improve quality of life.
Menopause can be a very overwhelming time for a lot of women. During this period, there are a lot of hormonal changes that can influence the way you feel in your body. Menopause tends to start between the ages of 45 to 55. This can include a range of symptoms such as hot flashes and mood swings to vaginal dryness and changes in pelvic health.

How does Menopause affect pelvic health?
Many women don’t realize that menopause can affect pelvic health. As estrogen levels decline, tissues in the vagina, urethra, and bladder can become thinner, drier, and less elastic, leading to a condition called vaginal atrophy. This can cause uncomfortable symptoms such as vaginal dryness, itching, burning, and pain during sex. In addition, menopause can also increase the risk of pelvic floor disorders, such as incontinence and prolapse. But don’t worry, many of these conditions can be improved through pelvic physiotherapy!
What is pelvic floor physiotherapy?
Pelvic floor physiotherapy is a specialized form of physiotherapy that focuses on the pelvic floor muscles, which support the pelvic organs (bladder, uterus, and rectum) and control bladder and bowel function. Pelvic physiotherapy can help to improve pelvic health during menopause and beyond, providing relief from uncomfortable symptoms and reducing the risk of pelvic floor disorders.
What does Pelvic Health Physiotherapy Involve?
Pelvic floor physiotherapy involves a range of techniques designed to improve the strength, coordination, and function of the pelvic floor muscles. These techniques may include pelvic floor exercises, biofeedback, electrical stimulation, manual therapy, and education on lifestyle modifications. It is an effective alternative to drug based therapy and surgery, and allows for you to take your health into your own hands.
How Can Pelvic Physiotherapy Help During Menopause?
- Pelvic physiotherapy can help to address a range of pelvic health issues that can arise during menopause, including:
- Vaginal Dryness: Pelvic physiotherapy can help to improve blood flow to the vaginal area, which can increase lubrication and reduce discomfort during intercourse. Additionally, exercises to strengthen the pelvic floor muscles can help to improve vaginal tone and elasticity.
- Urinary Incontinence: Pelvic physiotherapy can help to strengthen the pelvic floor muscles that support the bladder, which can improve bladder control and reduce urinary incontinence.
- Prolapse: Pelvic physiotherapy can help with prolapse symptoms or post-hysterectomy. With a prolapse, there is commonly increased muscle tone causing the organ to descend. This can be improved with exercise and treatment. Post hysterectomy, there can be pelvic floor weakness or altered sensation internally which can also be treated through strengthening and sensitization work.
- Painful Intercourse: Pelvic physiotherapy can help to improve vaginal tone and elasticity, which can reduce pain and discomfort during intercourse.
How can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“While menopause symptoms can be challenging, they are not inevitable for everyone and can be managed with the right care. Triangle Physiotherapy offers specialized services to help you navigate this stage of life across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can provide personalized treatment plans to alleviate symptoms and improve your quality of life.”
What is vaginismus?
Vaginismus is a condition where the muscles around the vagina involuntarily contract, making it difficult or impossible to have vaginal penetration.
Do I have vaginismus?
If you answer yes to one or more of the following questions, you must book an appointment with a pelvic health physiotherapist to find out if you have vaginismus.
“Sex is so uncomfortable for me.”
“Why does it hurt to have sex? My doctor cannot find anything wrong with me.”
“Internal pelvic exams are a no for me – they are so painful.”
“My vagina feels like a fort that is impenetrable. I never realized it was vaginismus.”
“I used to have great sex, but now I close up—it burns and stings.”
“When my partner starts to move inside me, it hurts and we have to stop.”
“I don’t wear tampons because they don’t go in.”
What are the symptoms of vaginismus?
The symptoms may differ between younger and older women, emphasizing the significance of an accurate diagnosis and effective treatment for vaginismus.
The primary symptoms of vaginismus are:
- Sexual penetration seems physically impossible despite repeated attempts
- Difficulty inserting tampons from youth even after repeated attempts.
- Difficulty undergoing internal pelvic/gynecological exam
What are the causes of Vaginismus?

The exact causes of vaginismus can vary from person to person, and in many cases, the condition is multifactorial, meaning that multiple factors may contribute to its development. Here are some potential causes and contributing factors:
- Psychological factors: Emotional or psychological factors can play a significant role in vaginismus. Past traumatic experiences, such as sexual abuse, rape, or a history of painful intercourse, can contribute to the development of vaginismus. Anxiety, fear, guilt, or negative beliefs about sex can also trigger involuntary muscle contractions.
- Fear of pain or discomfort: Some individuals may develop vaginismus due to a fear of pain or discomfort during sexual intercourse. This fear can be based on previous painful experiences, cultural or religious beliefs, or misinformation about sex.
- Relationship issues: Difficulties in the relationship, such as poor communication, lack of trust, unresolved conflicts, or sexual problems, can contribute to the development or persistence of vaginismus. Emotional or physical distance between partners can create tension and anxiety during sexual activity.
- Cultural or religious factors: Cultural or religious beliefs and practices surrounding sex can influence a person’s perception of sexuality and contribute to the development of vaginismus. Upbringing that emphasizes guilt, shame, or negative attitudes towards sex can lead to involuntary muscle contractions during attempts at vaginal penetration.
- Lack of sexual education: Insufficient knowledge or understanding about sexual anatomy, arousal, and relaxation techniques can contribute to vaginismus. Inadequate sexual education may lead to misconceptions, anxiety, and fear surrounding sexual activity.
- Medical conditions or infections: Certain medical conditions, such as vaginal infections, urinary tract infections, endometriosis, or pelvic inflammatory disease, can cause pain during sex, leading to the development of vaginismus. Vaginal dryness or atrophy, often associated with menopause, can also contribute to discomfort and muscle tightness.
- Traumatic childbirth experiences: Some women may develop vaginismus after experiencing a traumatic childbirth, especially if they had a difficult or painful delivery. The association of vaginal penetration with the traumatic event can trigger involuntary muscle contractions.
What are the treatment options for vaginismus?
Pelvic health physiotherapy is a common treatment option for vaginismus. It involves a physical therapist working with the patient to help relax and strengthen the pelvic floor muscles.
Possible treatments include:
- Progressive pelvic floor muscle relaxation
- Biofeedback or muscle stimulation
- Yoga-based therapy
- Hip mobility work
- Lumbar spine mobility work
What can I expect during an assessment and treatment for vaginismus at Triangle Physiotherapy?
Assessment
The first step in pelvic health physiotherapy for vaginismus is usually an assessment of the patient’s pelvic floor muscles. This may involve an internal examination, but the therapist will always seek the patient’s consent and respect their comfort level.
Treatment
Once the assessment is complete, the therapist will develop a treatment plan tailored to the patient’s needs. This may involve exercises to strengthen the pelvic floor muscles or techniques to help the patient relax those muscles.
Techniques
One common technique used in pelvic health physiotherapy for vaginismus is called progressive muscle relaxation. This involves tensing and then releasing the pelvic floor muscles in a controlled way to help the patient become more aware of them and learn how to control them.
Another technique that may be used is biofeedback. This involves using sensors to monitor the activity of the pelvic floor muscles, which can help the patient learn to control them more effectively.
Overall, pelvic health physiotherapy can be an effective treatment for vaginismus, but it is important to work with a qualified physical therapist who has experience in this area. With patience, persistence, and the right guidance, many people with vaginismus can overcome their condition and enjoy fulfilling sexual relationships.
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you. Book an Appointment today!
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Managing vaginismus and improving intimacy is possible with the right physiotherapy care. Triangle Physiotherapy offers specialized pelvic health services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you overcome pain and enhance your intimate relationships through personalized treatment plans.”