Undergoing any type of surgery can be a daunting experience, especially when you are dealing with pain or discomfort in the lead-up to the procedure. For many patients, managing pain before surgery can be as crucial as the surgery itself, both in terms of improving the surgical outcome and enhancing recovery. Physiotherapy is an essential part of this pre-surgical care, providing strategies to manage pain, improve mobility, and prepare the body for the challenges of surgery and rehabilitation. The highly trained physiotherapists at Triangle Physiotherapy can advise you on strategies on managing pain before surgery and how it can help you feel stronger, more comfortable, and better equipped for recovery.
What is Pre-Surgical Physiotherapy?
Pre-surgical physiotherapy, often referred to as “prehabilitation,” is the practice of preparing the body before surgery through a series of targeted exercises, education, and therapies. The goal is to improve physical fitness, increase mobility, and reduce pain prior to undergoing surgery. By strengthening muscles, improving joint mobility, and reducing stress on affected areas, prehabilitation can make the body more resilient during the recovery process and even reduce the risk of complications after surgery.

The Importance of Managing Pain Before Surgery
Chronic pain, whether from conditions like arthritis, injuries, or musculoskeletal disorders, can be overwhelming and can negatively affect the body’s ability to heal post-surgery. Pre-surgical pain management is not just about addressing discomfort; it’s about setting the stage for a smoother recovery. Here’s why it’s essential to manage pain before surgery:
- Reducing the Impact of Surgery on the Body
Chronic pain can weaken muscles and joints, affecting overall mobility. If these issues are not addressed before surgery, they can impede recovery, increase stress on the surgical site, and lengthen the rehabilitation process. By managing pain pre-operatively, you can make the body more capable of handling the stresses of surgery. - Improved Post-Surgical Outcomes
Research has shown that patients who engage in pre-surgical physiotherapy tend to have better outcomes following surgery. They often experience reduced pain post-operation, faster healing, and a quicker return to normal activities. - Preventing Muscle Atrophy and Stiffness
When dealing with long-term pain, it’s common to limit movement in order to avoid discomfort. This inactivity can lead to muscle atrophy (weakening) and joint stiffness. Physiotherapy helps maintain and even improve strength and flexibility before surgery, ensuring the body is in the best possible condition for a smooth recovery.
How Physiotherapy Can Help Manage Pain Before Surgery
Physiotherapists are experts in movement and pain management, and they can develop tailored treatment plans that address the specific needs of each individual. Here’s how physiotherapy can help manage pain before surgery:
- Pain Relief Techniques
Physiotherapists use a variety of manual therapy techniques to reduce pain and improve joint function. These may include:- Massage therapy to relax muscles and reduce tension.
- Joint mobilizations to increase range of motion and alleviate stiffness.
- Myofascial release to address tightness and discomfort in the soft tissues.
- These techniques can help reduce the intensity of pain, making it easier to engage in exercises and movements that promote healing.
- Strengthening Exercises
Weak muscles can contribute to pain and difficulty moving. Physiotherapists can develop a customized exercise program to strengthen muscles around the affected joints, improving stability and reducing the strain on pain-prone areas. Strengthening key muscle groups ensures that the body is well-prepared for the demands of surgery and recovery. - Mobility and Flexibility Training
Stiffness in the joints and muscles can exacerbate pain and hinder movement. Physiotherapists incorporate stretching and flexibility exercises into pre-surgical programs to improve range of motion. Whether it’s the hips, knees, or shoulders, increasing flexibility can reduce discomfort and prevent further limitations, allowing for better post-surgical rehabilitation. - Postural Correction
Poor posture can put additional strain on joints and muscles, exacerbating pre-existing pain. Physiotherapists assess your posture and provide education on how to align your body correctly during daily activities. Proper posture can prevent unnecessary pressure on joints and muscles, reducing pain and discomfort before surgery. - Education and Pain Management Strategies
Physiotherapists teach patients how to manage pain more effectively through techniques like breathing exercises, mindfulness, and relaxation strategies. Additionally, they may provide advice on managing pain at home, such as the use of heat or cold therapy and ergonomic adjustments in daily activities.
When Should You Seek Pre-Surgical Physiotherapy?
If you’re preparing for surgery and are experiencing pain, stiffness, or limited mobility, it’s a good idea to seek physiotherapy before your procedure. The sooner you begin prehabilitation, the better the results. Ideally, pre-surgical physiotherapy should begin a few weeks to months before the surgery date. However, even if you’re closer to your surgery, starting physiotherapy as soon as possible can still provide significant benefits.
Where can I find a Pre-Surgical Physiotherapy clinic in Oakville?
Triangle Physiotherapy has 8 locations in the GTA, with a physiotherapy clinic in Oakville, located at 2501 Prince Michael Drive, Oakville ON L6H7V6.
Book your prehabilitation appointment today to ensure you get the best outcomes from your surgery.
Knee pain can significantly impact your daily activities and overall quality of life. Whether it’s due to an injury, arthritis, or overuse, finding effective relief is essential. Physiotherapy is a valuable tool in managing knee pain, providing strategies to alleviate discomfort and improve function. Whether your knee pain is from a fall, a sports injury, arthritis or everyday aches and pains, our physiotherapists at Triangle Physiotherapy are here to help you navigate your recovery.
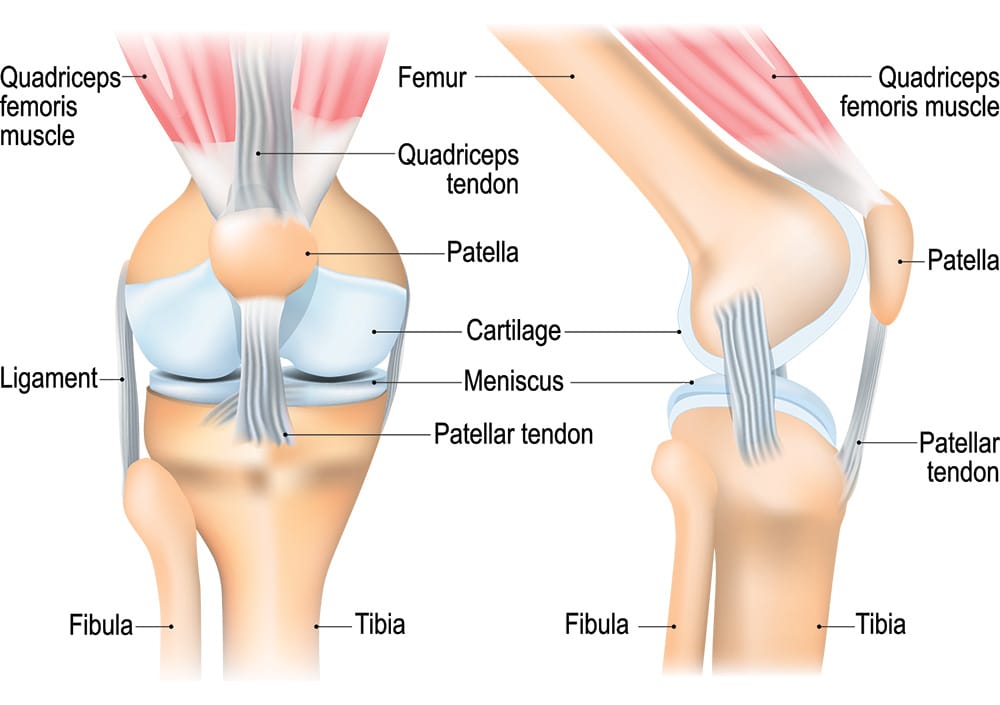
Understanding Knee Pain
Knee pain can arise from various conditions, including ligament injuries, tendonitis, bursitis, post-surgery or osteoarthritis. The pain may manifest as sharp, dull, or throbbing sensations, making it challenging to perform everyday tasks. Understanding the underlying cause is crucial for effective treatment. Physiotherapy takes a comprehensive approach to address not only the symptoms but also the root cause of the pain.
The Role of Physiotherapy
Physiotherapy offers a structured treatment plan tailored to your specific needs. A physiotherapist will conduct a thorough assessment, reviewing your medical history and evaluating your knee’s function. Based on this assessment, they will develop an individualized treatment plan focused on relieving pain, restoring mobility, and strengthening the muscles around the knee.
Pain Management Techniques for Knee Pain
Physiotherapists employ various techniques to manage knee pain effectively. These can include:
- Manual Therapy: Hands-on techniques to mobilize the knee joint and surrounding tissues, reducing stiffness and improving range of motion.
- IMS: Intra muscular Stimulation is an effective tool to trace and treat the root cause, reducing recurrence.
- Modalities: Methods such as ultrasound, heat, or cold therapy can help alleviate pain and inflammation. Read about PEACE and LOVE protocol instead of PRICE.
- Education: Learning about your condition, including proper body mechanics and strategies to avoid aggravating your knee, is vital for long-term management.
Strengthening Exercises
Strengthening the muscles surrounding the knee is crucial for stability and pain relief. Physiotherapists will guide you through targeted exercises that focus on the quadriceps, hamstrings, and calves. These exercises help improve strength and support the knee joint, reducing strain and preventing further injuries.
Mobility and Flexibility
Maintaining mobility and flexibility in the knee is essential for functional movement. Physiotherapy includes stretching exercises and gentle range-of-motion activities to help restore flexibility and reduce stiffness. This focus on mobility not only alleviates pain but also enhances your overall physical activity levels.
Knee Pain Prevention Strategies
Preventing future knee pain is a key aspect of physiotherapy. Your physiotherapist will educate you on proper techniques for daily activities, including walking, climbing stairs, and exercising. They will also address any risk factors, such as muscle imbalances or poor posture, to help you avoid re-injury.
FAQs
Can a physiotherapist help with my knee pain?
Yes, physiotherapists specialize in treating knee pain through tailored rehabilitation programs that target the underlying causes and symptoms.
What should I expect during my first visit to Triangle Physiotherapy?
During your first visit, you’ll undergo a comprehensive assessment, where your physiotherapist will evaluate your knee’s condition, discuss your medical history, and outline your treatment goals. A personalized plan will be created based on this information.
How many sessions will I need?
The number of sessions varies depending on the severity of your knee pain and your progress. Some patients may notice improvement in a few sessions, while others may require ongoing treatment. Your physiotherapist will provide an estimate during your assessment.
Do I need a referral to see a physiotherapist?
No, you do not need a referral to access physiotherapy services. You can book an appointment directly, unless required by your insurance for billing purposes.
How soon can I expect pain relief?
Many patients report relief within a few sessions, but the timeline may vary based on individual circumstances and the underlying cause of the knee pain.
How can I ensure effective management of my knee pain?
Engaging in physiotherapy, adhering to your rehabilitation plan, and performing prescribed exercises regularly are vital for managing knee pain effectively. Open communication with your physiotherapist will also help track your progress.
Conclusion
Physiotherapy is a powerful resource for managing knee pain. By understanding the nature of your condition and engaging in a tailored treatment plan, you can alleviate pain, restore function, and improve your quality of life. If you’re struggling with knee pain, consider the benefits that physiotherapy can provide in your recovery journey. To get help for your knee pain, you can call any of the locations of Triangle Physiotherapy or simply Book An Appointment online.
Recovering from orthopedic surgery is a crucial phase that sets the foundation for long-term mobility and quality of life. While surgery is a significant step toward healing, the recovery process often requires dedicated effort and guidance. This is where physiotherapy plays a vital role, helping patients regain strength, flexibility, and overall function. Triangle Physiotherapy can help you with your recovery journey post-surgery and safely transition back into your daily activities and sports.
Understanding Recovery from Surgery
Post-operative recovery involves more than just healing the surgical site; it encompasses rebuilding strength, restoring movement, and managing pain. Many patients face challenges like stiffness, weakness, and discomfort during this phase. Physiotherapy provides a structured approach to recovery, focusing on individualized treatment plans tailored to each patient’s specific needs. Engaging in physiotherapy early can significantly enhance recovery outcomes.
Neuromuscular Exercises for Recovery after Surgery
Neuromuscular exercises are designed to improve muscle coordination, strength, and balance. These exercises are particularly important after orthopedic surgery, as they help re-educate the muscles surrounding the surgical area. Examples include balance exercises, proprioceptive training, and targeted movements that activate specific muscle groups. By strengthening these muscles, patients can alleviate pain and improve stability, reducing the risk of future injuries.
Mobility Incorporation
Maintaining mobility is crucial during the recovery process. Physiotherapists incorporate mobility exercises, such as stretching and gentle range-of-motion activities, to help patients regain flexibility and prevent stiffness. Activities like yoga or tai chi may also be recommended, as they promote relaxation and enhance overall well-being. Incorporating mobility into daily routines not only aids in recovery but also encourages a healthier lifestyle.
Progressive Resistance Exercises
As recovery progresses, progressive resistance exercises become essential. These exercises gradually increase the intensity of strength training, allowing patients to build endurance and strength safely. Utilizing resistance bands, weights, or bodyweight, physiotherapists design programs that align with each patient’s recovery stage. This gradual approach ensures that patients do not overexert themselves while still making meaningful gains.
Prevention
Preventing future injuries is a significant aspect of post-operative care. Physiotherapists educate patients on proper body mechanics, ergonomics, and strategies to avoid movements that could lead to re-injury. By addressing risk factors and instilling healthy habits, patients can enhance their resilience and reduce the likelihood of setbacks.

FAQs
Can a physiotherapist help with my recovery?
Absolutely! Physiotherapists specialize in rehabilitation, offering tailored exercises and strategies to facilitate recovery from surgery.
What should I expect during my first visit to Triangle Physiotherapy?
During your first visit, you’ll undergo a thorough assessment where your physiotherapist will evaluate your condition, review your medical history, and discuss your recovery goals. A personalized treatment plan will be created based on this information.
How many sessions will I need?
The number of sessions varies based on your specific surgery and recovery progress. Some patients may see improvement in a few sessions, while others might require ongoing therapy. Your physiotherapist will provide an estimate during your assessment.
Do I need a referral to see a physiotherapist?
No, you do not need a referral to access physiotherapy services. You can book an appointment directly, unless your insurance requires it for billing purposes.
How soon can I expect pain relief?
Many patients report improvements within a few sessions, but the timeline can vary depending on individual circumstances and the nature of the surgery.
How can I ensure a smooth recovery?
Engaging in physiotherapy, following your rehabilitation plan, and incorporating exercises into your daily routine are essential for a successful recovery. Listening to your body and communicating with your physiotherapist will also help you stay on track.
Learn More About Pre and Post-Surgery Physiotherapy at Triangle Physiotherapy
Physiotherapy is integral to post-orthopedic surgery recovery. By understanding the recovery process, incorporating targeted exercises, and prioritizing prevention, patients can regain their independence and improve their quality of life. If you’re preparing for surgery or currently in recovery, consider the invaluable support that physiotherapy can offer.
If you would like to know more about how we can help you with your pre or post-surgery rehab, call us to schedule an initial assessment today!
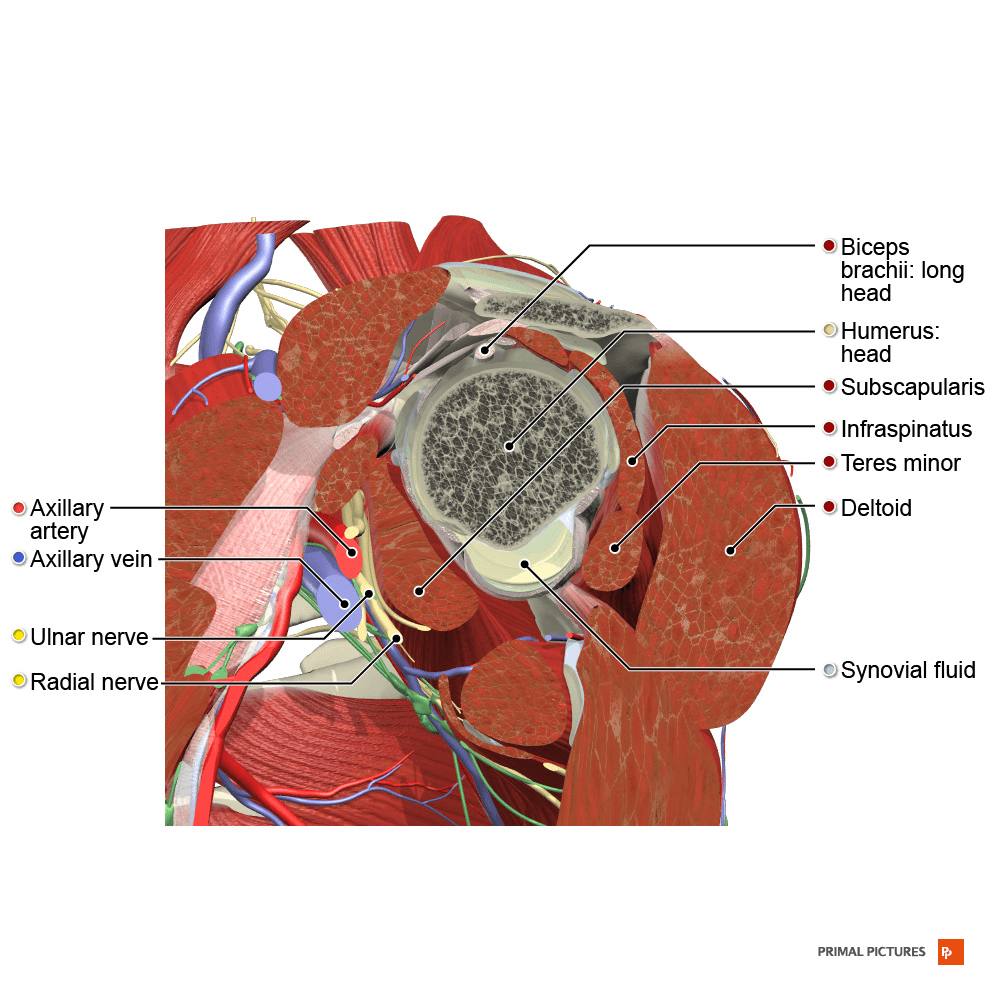
Rotator cuff tears can be a challenging injuries, impacting your ability to perform everyday tasks and participate in activities you enjoy. The rotator cuff, a group of four muscles and their tendons located in the shoulder, is crucial for shoulder stability and movement. Physiotherapy plays a vital role in the recovery process, helping to alleviate pain, restore function, and prevent future injuries. In this guide, we’ll explore how physiotherapists can assist with a rotator cuff tear, including causes, prevention strategies, and various physiotherapy techniques.
Our physiotherapists in Toronto can help you with rotator cuff injuries and rehabilitation.
Causes of Rotator Cuff Tears
What It Is: The rotator cuff consists of four muscles—supraspinatus, infraspinatus, teres minor, and subscapularis (SITS) —that stabilize and move the shoulder joint. A tear in one or more of these tendons can disrupt shoulder function.
Common Causes:
- Overuse: Repetitive overhead motions, such as those performed in sports like baseball or tennis, can lead to gradual wear and tear.
- Acute Injury: A sudden fall or lifting a heavy object can cause an acute rotator cuff tear.
- Aging: As we age, the tendons can weaken and become more prone to tears due to decreased blood supply and collagen degeneration.
Prevention Strategies
How to Reduce Risk: Although some rotator cuff tears are unavoidable, implementing preventive measures can help minimize the risk.
- Strength Training: Strengthen the muscles around the shoulder, including the rotator cuff muscles, to support the joint and prevent strain.
- Proper Technique: Use correct form when performing overhead activities or lifting weights to reduce undue stress on the shoulder.
- Regular Stretching: Maintain flexibility in the shoulder and adjacent joints to prevent stiffness and improve the range of motion. For example, one tends to have tight chest muscles and weak back muscles, hence the shoulder overcompensates.
Resistance Exercises
Purpose: Resistance exercises help build strength in the rotator cuff and surrounding muscles, which is crucial for stabilizing the shoulder joint and aiding recovery.
Examples:
- External Rotations: Use a resistance band or light dumbbell to perform external rotation exercises, targeting the infraspinatus and teres minor.
- Internal Rotations: Perform internal rotation exercises with a band or dumbbell to strengthen the subscapularis muscle.
- Scapular Retractions: Strengthen the muscles between the shoulder blades to support overall shoulder function.
How to Do Them Safely: Start with low resistance and increase gradually as your strength improves. Focus on controlled movements to avoid further strain on the shoulder.
Neuromuscular Exercises
Purpose: Neuromuscular exercises enhance coordination and the communication between your brain and muscles, improving shoulder stability and function.
Examples:
- Shoulder Blade Squeezes: Squeeze your shoulder blades together to activate the muscles that stabilize the shoulder.
- Proprioceptive Training: Use a stability ball or balance board to improve proprioception and shoulder stability.
- Dynamic Movements: Incorporate exercises that involve dynamic shoulder movements to enhance neuromuscular control.
How to Do Them Safely: Start with basic exercises and progress to more challenging ones as your coordination and stability improve.
Progressive Exercises
Purpose: Progressive exercises are designed to gradually increase in difficulty, helping to build strength and endurance while avoiding overexertion.
Examples:
- Shoulder Press: Begin with light weights and gradually increase the load as your shoulder strength improves.
- Front Raises: Use light dumbbells to perform front raises, increasing the weight progressively.
- Side-Lying Abduction: Lift your arm while lying on your side to strengthen the shoulder muscles, starting with lighter resistance and increasing as tolerated.
How to Do Them Safely: Follow a structured program that gradually increases the intensity and complexity of exercises to prevent overuse injuries.
Stretching and Strengthening
Purpose: Stretching maintains flexibility and reduces stiffness, while strengthening exercises build muscle support necessary for shoulder stability.
Examples:
- Pendulum Exercises: Allow your arm to swing gently in circles to improve flexibility and reduce stiffness.
- Cross-Body Stretch: Stretch the shoulder by bringing one arm across your body and holding it with the opposite arm.
- Strengthening Exercises: Perform exercises like resisted shoulder external and internal rotations to build rotator cuff strength.
How to Do Them Safely: Stretch slowly and hold each stretch for 15-30 seconds. Ensure strengthening exercises are done with proper form and controlled movements.
Mobility Routine
Purpose: A mobility routine focuses on improving the range of motion and overall function of the shoulder joint.
Examples:
- Shoulder Circles: Perform gentle shoulder circles to increase flexibility and mobility.
- Wall Angels: Stand with your back against a wall and slowly move your arms up and down to improve shoulder movement.
- Towel Stretch: Hold a towel behind your back with both hands and gently pull to stretch the shoulder.
How to Do Them Safely: Perform exercises within a comfortable range of motion and avoid pushing through pain.
Tips for Safely Performing Activities
How to Stay Safe: As you recover and resume activities, following these tips can help prevent re-injury and ensure a safe return to your routine.
- Listen to Your Body: Pay attention to any pain or discomfort and modify your activities as needed.
- Gradual Return: Ease back into your regular activities and sports gradually to allow your shoulder to adjust.
- Use Proper Technique: Ensure you use correct techniques for overhead movements and lifting to prevent undue stress on your shoulder.
Seek Professional Guidance: Work with a physiotherapist to develop a personalized rehabilitation program and get advice on technique and progression.
Recovering from a rotator cuff tear involves a comprehensive approach that includes strength building, flexibility exercises, and proper mobility routines. By incorporating resistance and neuromuscular exercises, following a progressive exercise routine, and paying attention to your body’s signals, you can enhance your recovery and reduce the risk of future injuries. Remember, patience and consistency are key in your rehabilitation journey. With the right physiotherapy and preventive measures, you’ll be back to your favorite activities stronger and more resilient.Don’t let these physical conditions ever ride on you.
Click here to book an appointment with a physiotherapist in Toronto.
Carpal tunnel syndrome (CTS) is a common condition that affects many individuals, often causing pain, numbness, and tingling in the hand and arm. If you’ve undergone carpal tunnel decompression surgery to alleviate these symptoms, you might be wondering about the next steps in your recovery journey.
One crucial aspect of postoperative care is physiotherapy. In this blog post, we’ll explore how physiotherapy can aid in your recovery after carpal tunnel surgery and what you can expect from the process, especially if you’re seeking physiotherapy in Oakville.
Understanding Carpal Tunnel Decompression Surgery
What is Carpal Tunnel Syndrome?
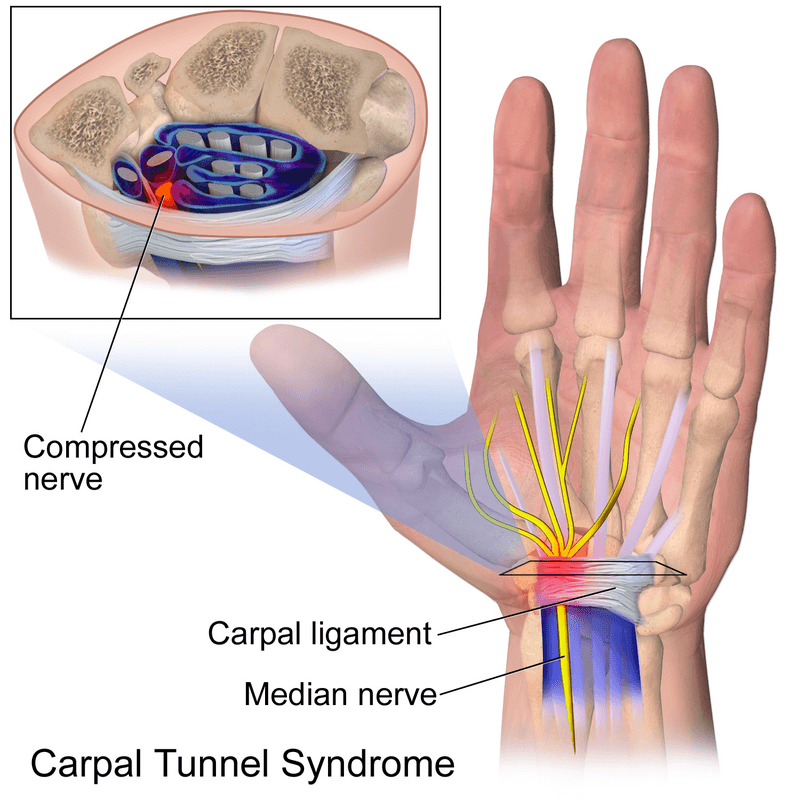
Carpal tunnel syndrome occurs when the median nerve, which runs from the forearm into the palm of the hand, becomes compressed at the wrist. This can result from various factors, including repetitive hand movements, wrist anatomy, or underlying health conditions.
Surgical Intervention
When conservative treatments like splinting, anti-inflammatory medications, or steroid injections fail to relieve symptoms, carpal tunnel surgery might be recommended. The procedure involves cutting the ligament that is pressing on the median nerve, thereby reducing pressure and alleviating symptoms.
The Role of Physiotherapy in Recovery
Initial Post-Surgery Phase
Immediately after surgery, the focus is on wound care, pain management, and preventing infection. During this period, your wrist and hand might be immobilized to promote healing. Physiotherapy often begins shortly after this initial phase.
Benefits of Physiotherapy
- Pain Relief: Physiotherapy can help manage postoperative pain through various techniques such as manual therapy, ice application, and ultrasound therapy.
- Reducing Swelling: Techniques like lymphatic drainage and specific exercises can help reduce swelling in the wrist and hand.
- Restoring Mobility: Gentle exercises and stretches are introduced to restore the range of motion in the wrist and fingers.
- Strengthening Muscles: Gradual strengthening exercises are crucial to rebuild the muscles weakened by surgery and inactivity.
- Scar Management: Physiotherapists can use techniques to minimize scar tissue formation and improve the flexibility of the scar.
- Functionality Restoration: The ultimate goal is to help you return to your normal daily activities without pain or limitation.

Typical Physiotherapy Regimen
- Assessment: Your physiotherapist will assess your specific condition, including the range of motion, strength, pain levels, and any functional limitations.
- Custom Exercise Program: Based on the assessment, a tailored exercise program will be designed. This may include:
- Range of Motion Exercises: Gentle stretching to improve flexibility.
- Strengthening Exercises: Using resistance bands or light weights to strengthen hand and wrist muscles.
- Nerve Gliding Exercises: To enhance the mobility of the median nerve.
- Manual Therapy: Hands-on techniques to mobilize joints and soft tissues, reduce pain, and improve function.
- Education: Learning about ergonomics and proper hand use to prevent recurrence or further injury.
Physiotherapy in Oakville
If you are based in Oakville, you have access to a range of skilled physiotherapists who can guide you through your recovery. Triangle Physiotherapy in Oakville is known for its comprehensive and patient-centered approach, ensuring that each individual receives personalized care tailored to their specific needs.
Triangle Physiotherapy in Oakville emphasizes the importance of a tailored exercise program, which includes range of motion exercises, strengthening routines, and nerve gliding techniques. The physiotherapists here are experienced in scar management and manual therapy, ensuring a holistic approach to your recovery.
How Long Will Physiotherapy Last?
The duration of physiotherapy varies depending on the severity of your condition, the extent of the surgery, and your individual response to treatment. On average, patients may undergo physiotherapy for several weeks to a few months. Regular follow-up sessions will track progress and adjust the treatment plan as needed.
Get started on your journey to recovery with the help of our talented physiotherapists in Oakville.
At Triangle Physiotherapy in Oakville, our team is skilled in evaluating each person’s unique needs to create a customized treatment plan. We ensure that your physiotherapy program provides comprehensive care, addressing all possible issues.
Call us at 905.257.3334 to book an appointment or request an appointment online HERE.
“After carpal tunnel surgery, it’s important to receive the right rehabilitation care. Triangle Physiotherapy is here to help you recover with specialized services across the GTA. Our clinics offer Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Let our expert team guide you through your post-surgery recovery for the best possible outcomes.”
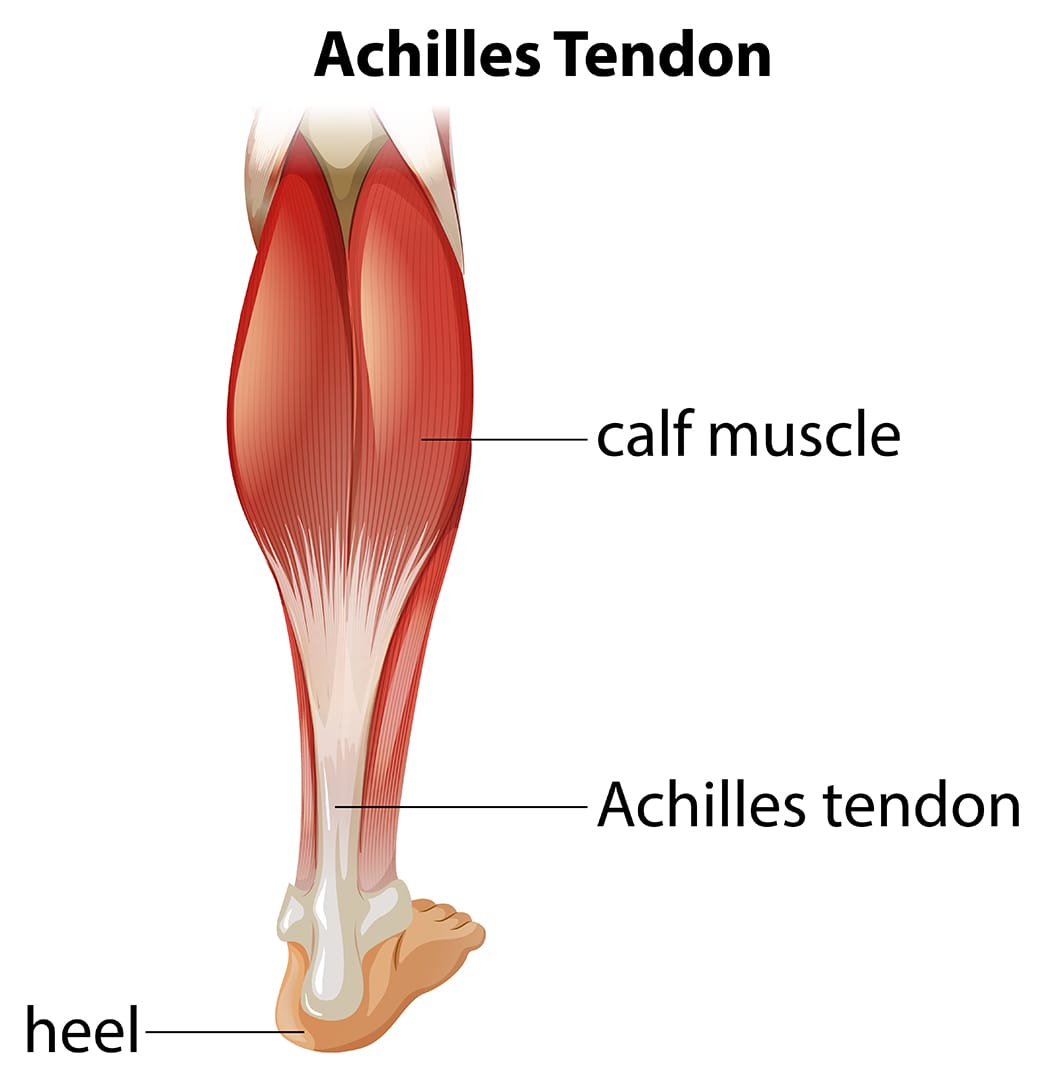
If you have had achilles tendon repair surgery or are scheduled for a procedure, you are likely going to need post-surgery rehabilitation to recover completely. It is also advisable to do physiotherapy pre-surgery to maximize the outcomes of the surgery. This is also known as prehab or pre-surgery rehab. At Triangle Physiotherapy, our physiotherapists are skilled and experienced at helping their patients reach their optimal level of recovery. If you’re looking for expert guidance in post-surgery rehab near you or post-operative physiotherapy in Toronto, you’ve come to the right place.
Achilles tendon injuries are common, particularly among athletes and active individuals. The Achilles tendon, the largest and strongest tendon in the body, connects the calf muscles to the heel bone, playing a crucial role in walking, running, and jumping. When this tendon is torn or ruptured, Achilles repair surgery is often necessary. However, surgery is only the first step toward recovery. Effective rehabilitation is essential for restoring function, strength, and mobility. In this blog, we’ll guide you through the stages of Achilles repair surgery rehab, providing insights and tips to ensure a successful recovery.
Understanding Achilles Tendon Injuries
What is the Achilles Tendon?
The Achilles tendon is a band of fibrous tissue that links the calf muscles to the heel bone. It enables activities that involve pushing off the foot, such as running and jumping.
Common Causes of Achilles Tendon Injuries
- Overuse: Repetitive stress from activities like running can lead to micro-tears.
- Sudden Increase in Activity: Rapid changes in activity levels can strain the tendon.
- Trauma: Direct impact or sudden, forceful movement can cause a rupture.
- Age and Degeneration: As people age, tendons become less flexible and more prone to injury.
Achilles Repair Surgery
Goals of Surgery
- Reattach the torn ends of the tendon.
- Restore the tendon’s length and tension.
- Enable the patient to return to their pre-injury level of activity.
Tips for a Successful Rehab
- Consistency: Adhere to the rehab program and attend all physiotherapy sessions.
- Listen to Your Body: Avoid pushing through pain; inform your therapist of any discomfort.
- Nutrition: Maintain a balanced diet to support tissue repair and overall health.
- Patience: Recovery takes time; focus on gradual progress rather than rushing the process.
Rehabilitating after Achilles repair surgery is a structured and multi-phased process that requires dedication and guidance from skilled physiotherapists. At Triangle Physiotherapy, we are committed to providing personalized rehabilitation programs to ensure our patients achieve optimal recovery and return to their active lifestyles. If you’ve undergone Achilles repair surgery or are scheduled for one, contact us to learn how our expert team can support you through every step of your recovery journey.
For those searching for physiotherapy in Toronto, post-surgery rehab in Toronto, or post-operative physiotherapy in Toronto, we offer comprehensive services tailored to your needs.
For more information or to schedule an appointment, or call us at 416.203.8622. Let us help you get back on your feet stronger and healthier.
“Recovering from Achilles repair surgery requires expert care and guidance. Triangle Physiotherapy offers comprehensive rehabilitation services at several locations across the GTA. Visit our clinics for Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village to ensure a smooth and effective recovery journey with the help of our specialized physiotherapy team.”
Spinal fusion surgery is a medical procedure used to permanently join two or more vertebrae in the spine, eliminating motion between them. The goal of the surgery is to reduce pain, correct deformities, or improve stability in the spine.
When would I need Spinal Fusion Surgery?
Spinal fusion surgery is typically recommended for various spine conditions, including:
- Degenerative disc disease: When the discs between vertebrae break down, causing pain.
- Spondylolisthesis: When one vertebra slips forward over the one below it.
- Spinal stenosis: Narrowing of the spinal canal, leading to nerve compression.
- Scoliosis: Abnormal curvature of the spine.
- Fractures: Vertebrae that are broken or dislocated.
- Tumors: Removal of tumors that affect spinal stability.
- Infections: Infections that have caused damage to the vertebrae.
When do I start physiotherapy after surgery?
The timing of when to start physiotherapy after spinal fusion surgery depends on several factors, including the specifics of the surgery, the patient’s overall health, and the surgeon’s recommendations.
What does post-surgery rehab involve?
Immediate Postoperative Period (0-6 Weeks)
- Initial Phase: Physiotherapy may start in the hospital within a day or two after surgery. The focus is on gentle movements and exercises to improve circulation and prevent complications.
- Activities:
- Breathing exercises to prevent lung complications.
- Gentle leg movements like ankle pumps to improve blood flow.
- Log rolling technique for safe movement in and out of bed.
- Short, frequent walks to promote circulation and reduce stiffness.
Early Rehabilitation Phase (6-12 Weeks)
- When: Typically, more structured physical therapy begins around 4 to 6 weeks after surgery, depending on the surgeon’s assessment.
- Goals: Gradually increase mobility, start gentle strengthening exercises, and improve functional movements.
- Activities:
- Range of motion exercises.
- Gentle strengthening exercises for the core and lower extremities.
- Walking programs to gradually increase distance and duration.
- Education on proper body mechanics and posture.
Late Rehabilitation Phase (3-6 Months)
- When: Around 3 months post-surgery, assuming there are no complications.
- Goals: Restore full function, enhance strength and endurance, and improve posture and body mechanics.
- Activities:
- More advanced strengthening exercises using resistance bands or light weights.
- Low-impact aerobic exercises like swimming or cycling.
- Balance and coordination exercises.
- Functional training for daily activities.
Long-Term Rehabilitation Phase (6-12 Months)
- When: After 6 months, the patient should continue with physiotherapy based on individual progress and goals.
- Goals: Achieve optimal strength, flexibility, and functional ability, and prevent recurrence of symptoms.
- Activities:
- Progressive resistance training.
- Gradual reintroduction of higher-impact activities, if appropriate.
- Sport-specific training for athletes.
- Ongoing education on maintaining spine health.
Key Points to Consider
- Surgeon’s Recommendations: Always follow the specific guidelines and timelines provided by the surgeon, as they know the details of the surgery and individual patient needs.
- Listen to Your Body: Avoid pushing through pain. Pain is a signal that something might be wrong, and it’s important to communicate any discomfort to the physiotherapist or surgeon.
- Individual Variation: Each patient’s recovery is unique. Factors such as age, overall health, and the complexity of the surgery will influence the timing and intensity of physiotherapy.
Starting physiotherapy at the right time is crucial for a successful recovery, and adhering to a structured rehabilitation program can significantly enhance outcomes after spinal fusion surgery.
Click here to book an appointment for post-surgery rehab with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
General Information: The information provided on this blog is for general informational purposes only. While we strive to ensure the accuracy and relevance of our content, we make no guarantees about the completeness, reliability, or accuracy of the information.
Not Professional Advice: The content on this blog does not constitute professional advice. It is not a substitute for professional medical, legal, financial, or other professional advice. Always seek the guidance of a qualified professional with any questions you may have regarding your specific situation.
Recovering from spinal fusion surgery requires careful physiotherapy to restore mobility and strength. Whether you need physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are expert physiotherapists available to guide your recovery journey and help you regain your quality of life.








