Tension headaches are one of the most common forms of headache, often described as a constant ache or pressure around the forehead, temples, or back of the head. Unlike migraines, tension headaches usually don’t come with nausea or sensitivity to light, making them easy to overlook but challenging to manage for those who experience them frequently. In this blog, we’ll look into recovery strategies, including neuromuscular exercises, mobility incorporation, and progressive resistance exercises, as well as prevention techniques to help manage future occurrences.
The physiotherapists at Triangle Physiotherapy are happy to share practical tips and strategies to relieve you of your tension headaches.
What Recovery Involves
Recovery from tension headaches often involves addressing the underlying muscle tension and stress that contribute to their onset. These headaches can be triggered by various factors, including poor posture, prolonged sitting, stress, and lack of physical activity. A comprehensive recovery plan should focus on both immediate relief and long-term strategies to reduce the frequency and intensity of headaches. \
Neuromuscular Exercises
Neuromuscular exercises are designed to improve the coordination and function of the muscles involved in head and neck movement. These exercises can help alleviate tension and prevent future headaches by:
Strengthening Weak Muscles: Focus on the neck, shoulders, and upper back, which often harbor tension.
Improving Posture: Correcting posture can significantly reduce the strain on muscles and prevent the buildup of tension.
Promoting Relaxation: Gentle stretches and relaxation techniques can help reduce stress and muscle tightness. Examples of neuromuscular exercises include chin tucks, neck stretches, and shoulder rolls. Consistent practice can enhance muscle function and overall comfort.

Mobility Incorporation
Incorporating mobility exercises into your routine is vital for maintaining flexibility and preventing stiffness that contributes to tension headaches. Mobility exercises can include:
Dynamic Stretching: Engaging in movements that promote range of motion, such as arm circles and torso twists.
Foam Rolling: Targeting tight muscle groups in the neck, shoulders, and upper back can release tension and improve blood flow.
Yoga or Pilates: These practices emphasize controlled movements and breathwork, promoting both physical and mental relaxation.
Aim to incorporate mobility exercises into your daily routine, especially if you have a sedentary lifestyle.
Progressive Resistance Exercises for Tension Headaches
Progressive resistance exercises help build strength and endurance in the muscles that support your head and neck. A strong musculoskeletal system can better handle physical stressors, reducing the likelihood of tension headaches. Key components include:
Resistance Bands: Incorporating band exercises for the shoulders and upper back can help strengthen these areas.
Weight Training: Focus on compound movements like deadlifts and rows that engage multiple muscle groups.
Gradual Increase: Start with lighter weights or resistance and gradually increase as your strength improves.
This approach not only enhances physical strength but also boosts overall confidence and body awareness.
Prevention of Tension Headaches
Preventing tension headaches involves a multi-faceted approach:
1. Regular Exercise: Aim for at least 30 minutes of moderate exercise most days of the week to promote overall well-being.
2. Stress Management: Techniques such as meditation, deep breathing, and mindfulness can help manage stress levels.
3. Ergonomics: Ensure that your workspace is set up to promote good posture and reduce strain on your neck and shoulders.
4. Hydration and Nutrition: Staying hydrated and maintaining a balanced diet can play a crucial role in overall health and headache prevention.
5. Sleep Hygiene: Prioritize good sleep habits, as lack of sleep can trigger headaches.
FAQs
Q: What are the common triggers for tension headaches?
A: Common triggers include stress, poor posture, eye strain, dehydration, and muscle tension.
Q: How can I differentiate between a tension headache and a migraine?
A: Tension headaches typically present as a dull, aching pain with a sensation of tightness, whereas migraines are often accompanied by nausea, vomiting, and sensitivity to light or sound.
Q: When should I see a doctor for my headaches?
A: If headaches become frequent, severe, or are accompanied by other concerning symptoms, it’s essential to seek medical advice.
Q: Can lifestyle changes really help reduce tension headaches?
A: Yes, adopting a healthy lifestyle with regular exercise, stress management, and good posture can significantly reduce the frequency and severity of tension headaches.
Q: Are there any specific exercises I should avoid?
A: Avoid exercises that strain the neck or upper back, especially if you experience pain during or after the activity. Tension headaches can be managed effectively with the right strategies in place. By incorporating neuromuscular exercises, enhancing mobility, and building strength through progressive resistance exercises, you can pave the way for recovery and prevention.
Book an appointment with our expert physiotherapists, chiropractors or massage therapists to get relief from your nagging tension headaches today!
Living in Canada, especially in cities like Etobicoke, means dealing with long winters and limited sunlight. Unfortunately, this impacts our Vitamin D levels. Many people aren’t aware of the importance of Vitamin D supplementation, often treating it like an optional vitamin similar to Vitamin C. However, Vitamin D is not as easily obtained from foods, making it vital to get it from other sources.
Our Naturopath in Etobicoke, Dr. David Gabriele talks about Vitamin D and it’s importance in this blog.
Why Is Vitamin D Important?

Vitamin D plays a crucial role in various bodily functions. Here’s what Vitamin D does and why maintaining optimal levels is essential:
Key Functions of Vitamin D
- Calcium & Phosphorus Balance
- Vitamin D helps in regulating calcium and phosphorus, which are necessary for maintaining strong bones. A deficiency can lead to bone density loss and chronic bone pain.
- Muscle Strength and Pain Reduction
- Low levels of Vitamin D can result in muscle weakness, cramps, and increased pain, which can affect daily activities and overall quality of life.
- Mood Regulation
- Vitamin D impacts mood and mental health. Deficiency has been linked to conditions like depression and anxiety, which are common concerns during the darker months in Etobicoke.
- Immune System Support
- A robust immune system needs adequate Vitamin D to function effectively. Low levels can increase the risk of infections and illnesses.
- Mitochondria Function and Energy Levels
- Vitamin D plays a role in the function of mitochondria, the powerhouse of cells, which can influence energy levels and combat fatigue.
- Blood Pressure and Insulin Regulation
- It also helps in regulating blood pressure and insulin sensitivity, reducing the risk of hypertension and Type 2 diabetes.
Risks of Vit D Deficiency
Due to the geographical location of Etobicoke and its long winter season, residents are at a higher risk of Vitamin D deficiency. Here are some health issues associated with low Vitamin D levels:
- Bone Density Loss & Chronic Pain
- Increased Muscle Weakness and Cramping
- Elevated Risk of Depression and Anxiety
- Higher Susceptibility to Infections
- Fatigue and Low Energy Levels
- Insulin Resistance and Risk of Type 2 Diabetes
- Increased Blood Pressure
Recommended Vitamin D Supplementation
The American Academy of Pediatrics advises all breast-fed and partially breast-fed infants to receive an oral vitamin D supplement of 400 IU/day. For children aged 1 to 13 years, a daily intake of 600 IU is recommended.
For adults, the general recommendation is 2000 IU/day. However, the required dosage may vary based on factors like:
- Diet
- Skin Pigmentation
- Age
- Body Weight
- Health Conditions
- Clothing Choices (especially in winter)
How to Boost Your Vit D Levels
Food Sources of Vitamin D
While supplements are often necessary, you can also get Vitamin D from dietary sources, such as:
- Fatty Fish (e.g., salmon, mackerel, tuna)
- Beef Liver
- Fortified Dairy Products
However, given Canada’s limited sunlight exposure, especially during winter, Vitamin D supplementation is generally recommended to ensure optimal health and disease prevention.
Get Your Vit D Levels Tested at Triangle Physiotherapy Etobicoke
At Triangle Physiotherapy Etobicoke, we understand the importance of maintaining adequate Vitamin D levels, especially for our clients dealing with chronic pain, muscle weakness, and other health conditions. If you suspect you might have a Vitamin D deficiency or are experiencing symptoms like fatigue, muscle cramps, or low mood, consider scheduling an appointment with one of our physiotherapists.
We can guide you on how to improve your Vitamin D levels through dietary adjustments, lifestyle changes, and appropriate supplementation.
Book Your Consultation Today!
Take charge of your health and well-being. Contact Triangle Physiotherapy Etobicoke to schedule an assessment and get personalized advice on Vitamin D supplementation.
In the realm of pain management and holistic health, both Intramuscular Stimulation (IMS) and acupuncture have gained popularity for their therapeutic benefits. While they share some similarities, they are distinct techniques with different underlying principles and applications. Understanding these differences can help you make an informed choice about which treatment might be right for you.
At Triangle Physiotherapy, our team of physiotherapists have training in Functional IMS, which is a highly effective, evidence-based dry needling technique.
What is Intramuscular Stimulation (IMS)?

Intramuscular Stimulation is a form of dry needling that targets trigger points in muscles. Developed by Dr. Chan Gunn in the 1970s, IMS focuses on relieving chronic pain caused by muscle dysfunction. The technique involves inserting thin needles into specific areas of the muscle to release tightness and improve blood flow, which can help alleviate pain.
Key Features of IMS:
- Targeted Treatment: IMS specifically addresses myofascial pain syndrome, where muscle tightness contributes to discomfort.
- Needling Technique: The needles used in IMS are usually inserted deeper into the muscle tissue compared to acupuncture needles.
- Focus on Muscle Dysfunction: IMS is primarily used for conditions like chronic pain, sports injuries, and muscle spasms.
What is Acupuncture?
Acupuncture is a traditional Chinese medicine practice that has been used for thousands of years. It involves inserting fine needles into specific points on the body, known as acupoints, to balance the body’s energy (Qi) and promote healing. Acupuncture is commonly used for a wide range of conditions, including pain management, stress relief, and overall wellness.
Key Features of Acupuncture:
- Holistic Approach: Acupuncture aims to restore balance in the body and address various health concerns beyond just pain.
- Meridian System: The treatment is based on the concept of energy pathways (meridians) and the flow of Qi, which influences overall health.
- Wider Applications: Acupuncture is used for conditions such as anxiety, digestive issues, and even insomnia, in addition to pain relief.
Comparing IMS and Acupuncture
Technique and Focus
- IMS targets specific muscles and trigger points, primarily addressing musculoskeletal pain. The needles are typically inserted deeper into the muscle and may elicit a local twitch response, which can help release tension.
- Acupuncture focuses on restoring balance in the body’s energy system and is used for a broader range of health issues. The needles are usually placed at superficial levels and may not target specific muscle dysfunctions.
Pain Experience
- IMS may involve more discomfort during treatment due to the depth of needle insertion and the nature of trigger point therapy.
- Acupuncture is generally perceived as a gentler technique. Patients often report feeling relaxed during the session, with minimal discomfort.
Treatment Goals
- IMS is primarily used for pain relief related to muscular dysfunction, helping to improve movement and reduce chronic pain.
- Acupuncture aims to enhance overall well-being, addressing not only pain but also various health conditions by balancing the body’s energy.
Which Treatment is Right for You?
Choosing between IMS and acupuncture depends on your specific needs and health goals. If you are experiencing chronic muscle pain or specific musculoskeletal issues, IMS may be more suitable. On the other hand, if you are looking for a holistic approach to improve overall health or manage multiple symptoms, acupuncture could be the better option.
Consultation with Professionals
Consulting with a qualified practitioner is crucial for determining the best treatment for your situation. Many practitioners are trained in both IMS and acupuncture, allowing them to tailor a treatment plan based on your unique needs.
The expert physiotherapists at Triangle Physiotherapy understand that every individual perceives pain differently, so they make sure every treatment plan is customized. We look forward to helping you recover from your pain and getting you back to the activities you love to do!
Experiencing upper back pain while running can be both frustrating and concerning. While many runners focus on lower body injuries, upper back pain is a common issue that can affect performance and enjoyment. Understanding the causes of this discomfort and exploring effective solutions is essential for maintaining a healthy running routine.
At Triangle Physiotherapy, our team of physiotherapists have the expertise and education to help you develop a plan to ensure your runs are done right!
Understanding Upper Back Pain
Upper back pain during running can arise from various factors, including muscle strain, poor posture, or underlying conditions. The upper back, or thoracic region, comprises the spine and surrounding muscles, which play a crucial role in maintaining proper running form. If any part of this system is compromised, it can lead to discomfort and pain.

Common Causes of Upper Back Pain While Running
- Poor Posture: Runners who hunch their shoulders or lean forward excessively may put strain on their upper back muscles, leading to pain. Maintaining a neutral spine and relaxed shoulders is essential for proper running form.
- Muscle Imbalance: Weakness in the core or upper back muscles can result in poor stabilization during running. This imbalance may lead to overcompensation by other muscles, causing pain.
- Overuse: Increasing running distance or intensity too quickly can lead to muscle fatigue and strain in the upper back. It’s crucial to allow adequate recovery time between runs.
- Tension and Stress: Mental stress can lead to physical tension in the upper body, exacerbating discomfort during exercise. Runners may unconsciously tighten their shoulders and upper back while running, contributing to pain.
How can Physiotherapy help?
Physiotherapy can play a significant role in addressing upper back pain related to running. A physiotherapist will conduct a thorough assessment to identify the underlying causes of your discomfort. Based on this evaluation, they will develop a personalized treatment plan that may include:
- Postural Assessment: Evaluating your running posture and identifying areas for improvement can help alleviate strain on the upper back.
- Strengthening Exercises: Targeted exercises to strengthen the upper back and core muscles can improve stability and support proper running form.
- Stretching and Flexibility Training: Incorporating stretches for the upper back and shoulders can relieve tension and enhance flexibility.
- IMS: Intra muscular Stimulation is an effective tool to trace and treat the root cause, reducing recurrence.
- Education: Learning about proper running techniques and body mechanics can help prevent further injuries.
Tips for Reducing Upper Back Pain While Running
- Warm-Up Properly: Engage in a dynamic warm-up to prepare your muscles for running. Focus on movements that activate the upper back and shoulders.
- Focus on Form: Pay attention to your running posture. Keep your shoulders relaxed and your chest open, and avoid hunching over while you run.
- Strength Train: Incorporate strength training exercises targeting the upper back and core into your fitness routine to build muscle balance and support.
- Gradually Increase Intensity: Avoid sudden increases in running distance or intensity. Follow a structured training plan to prevent overuse injuries.
- Manage Stress: Practice stress-reduction techniques, such as mindfulness or yoga, to help relieve physical tension in the upper body.
FAQs
Why does my upper back hurt when I run?
Upper back pain while running can result from poor posture, muscle imbalances, overuse, or tension. Identifying the specific cause is essential for effective treatment.
What should I expect during my first visit to Triangle Physiotherapy?
During your initial visit, a physiotherapist will assess your posture, movement patterns, and any contributing factors to your pain. They will develop a personalized treatment plan to address your needs.
How many sessions will I need?
The number of sessions varies based on the severity of your pain and your response to treatment. Your physiotherapist will provide an estimate after your assessment.
Do I need a referral to see a physiotherapist?
No, you do not need a referral to access physiotherapy services. You can book an appointment directly, unless needed by insurance for billing purposes.
How soon can I expect to feel better?
Many individuals notice improvements within a few sessions, but the timeline can vary depending on individual circumstances and the nature of the pain.
How can I prevent upper back pain while running?
Focus on maintaining good posture, strengthening your upper back and core, warming up properly, and gradually increasing your running intensity to help prevent pain.
Call us today to get help with any running related back pain issues!
Upper back pain during running is a common issue that can hinder performance and enjoyment. By understanding the underlying causes and implementing effective strategies, you can alleviate discomfort and enhance your running experience. Book an appointment with us to get help!
Chemotherapy-induced peripheral neuropathy (CIPN) is a common side effect that can significantly impact the quality of life for cancer patients. As chemotherapy drugs target rapidly dividing cells, they can inadvertently affect nerve cells, leading to symptoms that range from mild discomfort to debilitating pain. Understanding CIPN and exploring management strategies are essential steps in supporting patients through their cancer journey.
The Cancer Rehabilitation Physiotherapists at Triangle Physiotherapy are trained to help you navigate through the side effects of cancer treatment.
Understanding Chemotherapy-Induced Peripheral Neuropathy
CIPN is characterized by damage to the peripheral nerves, which can manifest in various ways, including tingling, numbness, burning sensations, and weakness in the hands and feet. This condition is not only uncomfortable but can also hinder daily activities and diminish overall well-being. Different chemotherapy agents, particularly platinum-based drugs, taxanes, and vinca alkaloids, are known to pose a higher risk for developing neuropathy.
Symptoms and Impact
The symptoms of CIPN can be diverse, including:
- Sensory changes: Tingling, numbness, or a “pins and needles” sensation.
- Motor issues: Weakness that may affect fine motor skills.
- Pain: Burning or sharp pain that can be constant or intermittent.
- Balance problems: Difficulty walking or maintaining stability, increasing the risk of falls.
The psychological impact of CIPN should not be overlooked, as patients may experience anxiety, depression, or a sense of loss of independence. Understanding the multifaceted nature of CIPN is crucial for effective management.
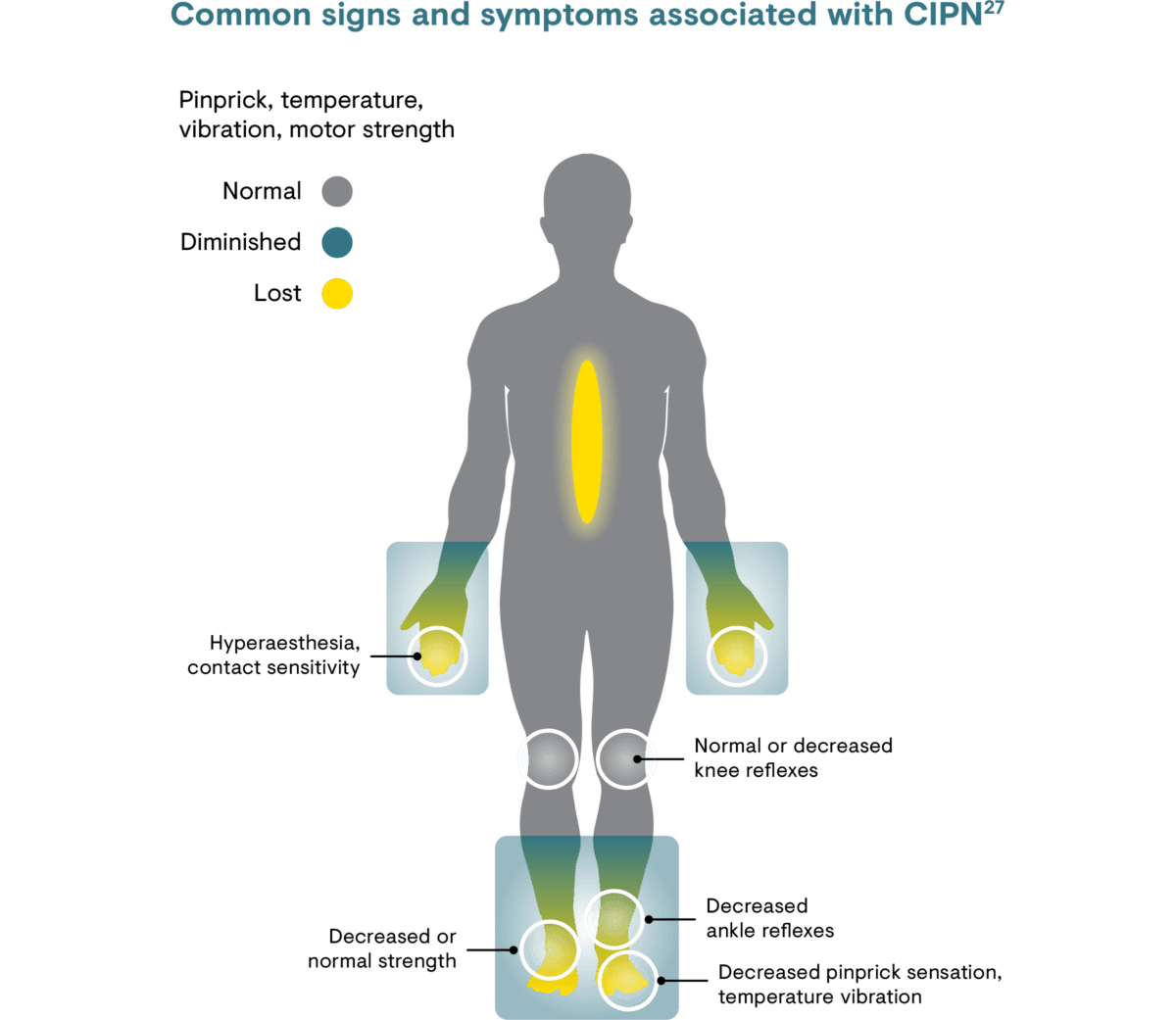
Picture Credit: https://www.grunenthal.com
Management Strategies
Education and Awareness
Empowering patients with knowledge about CIPN is vital. Understanding the potential for neuropathy allows patients to communicate effectively with their healthcare team and advocate for their needs. Regular screenings for neuropathy can help catch symptoms early, allowing for timely intervention.
Pharmacological Approaches
Medications such as anticonvulsants (e.g., gabapentin, pregabalin) and antidepressants (e.g., duloxetine) are often used to manage neuropathic pain. While these medications can be effective, it’s important for patients to discuss potential side effects and the best options for their individual situation with their oncologist.
Physical Rehabilitation
Engaging in physiotherapy can significantly aid in managing CIPN symptoms. A tailored rehabilitation program may include:
- Strength training: Gentle exercises to improve muscle strength and coordination.
- Balance training: Activities to enhance stability and reduce the risk of falls.
- Sensory retraining: Exercises that help patients re-learn normal sensations and improve tactile discrimination.
Incorporating regular physical activity can also boost overall health and mood.
Lifestyle Modifications
Adopting healthy lifestyle choices can help mitigate CIPN symptoms. Patients may benefit from:
- Nutritional support: A balanced diet rich in antioxidants and vitamins can support nerve health.
- Hydration: Staying well-hydrated may help reduce symptoms.
- Mindfulness practices: Techniques such as yoga, meditation, and deep-breathing exercises can reduce stress and improve overall well-being.
Complementary Therapies
Some patients find relief through complementary therapies such as acupuncture, massage, or mindfulness-based practices. While research on these therapies is still ongoing, many report positive outcomes in managing pain and improving quality of life.
CIPN FAQs
What should I do if I experience symptoms of CIPN?
It’s important to communicate any symptoms to your healthcare provider as soon as they arise. Early intervention can help manage symptoms more effectively.
Can CIPN be prevented?
While not all cases of CIPN can be prevented, discussing dose adjustments or alternative therapies with your oncologist may help mitigate risks.
How long does CIPN last?
The duration of CIPN varies among patients. Some may experience symptoms that resolve over time, while others may have persistent issues. Regular follow-up with your healthcare team is essential.
Is there a cure for CIPN?
Currently, there is no definitive cure for CIPN, but various management strategies can significantly alleviate symptoms and improve quality of life.
How common is CIPN?
Peripheral neuropathy after chemotherapy is very common. Experts estimate it’s experienced by 30% to 50% of patients who receive these types of chemotherapy.
The drugs most likely to cause CIPN are used to treat the most common types of cancer, including breast cancer, colon cancer, lung cancer, and prostate cancer.
Where can I find a physiotherapist that can help me with CIPN?
Triangle Physiotherapy has physiotherapists that are trained in helping you navigate the side effects caused by cancer treatments.
High ankle sprains are a common and often misunderstood injury, particularly among athletes and active individuals. While a typical ankle sprain affects the ligaments on the outside of the ankle, a high ankle sprain involves the ligaments above the ankle joint, specifically the syndesmosis. This injury can lead to significant discomfort and prolonged recovery times. The team of physiotherapists at Triangle Physiotherapy have the knowledge and expertise to treat ankle sprains, provide strategies for recovery, and ways to prevent future injuries.
Understanding Recovery from Ankle Sprains
Recovery from a high ankle sprain requires a comprehensive approach, focusing on reducing pain and swelling, restoring function, and strengthening the affected area. Typically, recovery can take anywhere from a few weeks to several months, depending on the severity of the sprain. Immediate treatment often involves the RICE method—Rest, Ice, Compression, and Elevation. As symptoms improve, a structured rehabilitation program becomes essential to regain full range of motion and strength. Key Phases of Recovery are as follows:
- Acute Phase: Focus on pain management and reducing swelling.
- Rehabilitation Phase: Gradual reintroduction of movement and strength training.
- Return to Activity: Gradual progression to sports-specific activities and ensuring proper conditioning.

Neuromuscular Exercises for Ankle Sprains
Neuromuscular exercises are vital for enhancing proprioception, balance, and coordination. These exercises train the body to respond to external stimuli, improving the neuromuscular connections essential for injury prevention. Recommended Neuromuscular Exercises can include Balance Board Exercises, Single-Leg Stands, Agility Drills.
Mobility Incorporation
Mobility is crucial for a successful recovery from a high ankle sprain. Incorporating mobility exercises helps restore flexibility and range of motion to the affected area, allowing for a smoother transition back to regular activities. Effective Mobility Exercises can include Ankle Circles, Calf Stretch, Toe Taps to name a few of the exercises.
Progressive Resistance Exercises for Ankle Sprains
Once basic mobility and strength have been regained, it’s important to incorporate progressive resistance exercises. These exercises help rebuild strength in the ligaments and muscles surrounding the ankle, providing greater support and stability. Examples of Progressive Resistance Exercises can include Theraband Exercises, Heel Raises, Squats and Lunges.
Prevention
Preventing high ankle sprains is crucial, especially for those involved in high-impact sports. Here are some effective strategies:
1. Warm-Up Properly: Always perform dynamic stretches and warm-up routines before engaging in physical activity.
2. Strengthen Ankle Muscles: Regularly incorporate exercises targeting the muscles around the ankle.
3. Wear Proper Footwear: Ensure shoes provide adequate support and are appropriate for the activity.
4. Practice Balance and Agility Drills: Regularly engage in activities that improve balance and coordination.
FAQs about Ankle Sprains
1. What is the difference between a high ankle sprain and a regular ankle sprain?
A. A high ankle sprain affects the ligaments above the ankle joint (the syndesmosis), while a regular ankle sprain involves the ligaments on the outside of the ankle. High ankle sprains typically take longer to heal.
2. How long does it take to recover from a high ankle sprain?
A. Recovery time varies depending on the severity of the injury, ranging from a few weeks to several months.
3. Can I return to sports before I’m fully healed?
A. It’s essential to follow a structured rehabilitation program and consult with a healthcare professional like a physiotherapist or chiropractor before returning to sports to avoid re-injury.
4. Are there any specific exercises to avoid during recovery?
A. High-impact activities or exercises that put excessive strain on the ankle, such as running or jumping, should be avoided until cleared by a professional.
Source: www.physio-pedia.com
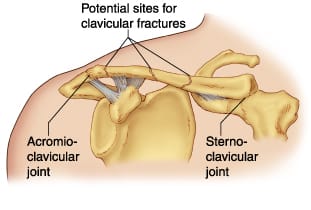
Clavicular fractures, commonly known as broken collarbones, are prevalent injuries, especially among athletes and those engaged in physical activities. This type of fracture typically occurs due to falls, direct trauma to collarbone or shoulder, or collisions. Understanding the clavicular fractures in detail, their recovery process, and preventive measures can help individuals better manage their healing journey and minimize the risk of future injuries.
Schedule an appointment with one of the physiotherapists at one of the 8 locations of Triangle Physiotherapy if you have had a clavicular fracture and are looking to achieve optimal recovery.
What is the recovery timeline for clavicular fractures?
The recovery timeline for a clavicular fracture can vary based on the severity of the break and the individual’s overall health. Generally, non-displaced fractures may heal within 6 to 12 weeks with conservative treatment, including rest, immobilization, and pain management. In more severe cases, surgical intervention may be necessary, leading to a slightly extended recovery period. During this time, it’s essential to follow medical advice and engage in a structured rehabilitation program under the supervision of a Physiotherapist to restore strength and function to the shoulder.
What type of exercises are beneficial in the rehabilitation Clavicular Fractures?
Neuromuscular Exercises
Neuromuscular exercises play a crucial role in the rehabilitation process. These exercises focus on improving coordination and communication between the nervous system and muscles, which is vital for shoulder recovery. Some forms of improving the neuro-muscle link could be gentle isometric contractions of the shoulder muscles without joint movement, activating the shoulder blade muscles. As healing progresses, activities that involve controlled movements can help enhance muscle activation and prevent stiffness, promoting a smoother transition to more strenuous exercises.
Mobility Incorporation
Incorporating mobility exercises into the rehabilitation program is essential for restoring range of motion in the shoulder. Gentle stretching and mobility drills should begin as soon as cleared by a healthcare professional. Physiotherapist would be the perfect healthcare practitioner that can guide you in terms of muscle activation and rehabilitation. Common exercises include pendulum swings and passive arm movements. These activities not only help to alleviate stiffness but also prepare the shoulder for more demanding functional tasks. Regularly practicing mobility exercises ensures that the joint remains flexible and reduces the risk of future injuries.
Progressive Resistance Exercises
Once the shoulder has regained sufficient mobility and strength, progressive resistance exercises can be introduced. These exercises aim to gradually increase the load on the muscles surrounding the shoulder joint, facilitating strength development and functional recovery. Starting with lightweight resistance bands or dumbbells, individuals can perform exercises focusing on rotator cuff, shoulder stabilizers as well as the scapular muscles. The key is to focus on form and gradually increase resistance as strength improves, avoiding any pain or discomfort.
How can clavicular fractures be prevented?
Preventing clavicular fractures involves a combination of strength training, proper technique, and awareness of one’s surroundings. In order to prevent clavicular fractures, one needs a multidisciplinary approach under the supervision of a Physiotherapist, Chiropractor and a Massage Therapist. Engaging in shoulder-strengthening exercises can improve stability and reduce the likelihood of injuries. Athletes should prioritize learning proper falling techniques to minimize impact during falls or collisions. Additionally, wearing protective gear in high-risk sports can provide an extra layer of safety. Overall, being proactive about shoulder health can significantly decrease the chances of experiencing a clavicular fracture.
Other FAQ’s
FAQs
Q: How can I tell if I have a clavicular fracture?
A: Symptoms may include sharp pain at the site of the injury, swelling, bruising, and difficulty moving the shoulder. A visible deformity or “bump” over the collarbone may also indicate a fracture.
Q: Do all clavicular fractures require surgery?
A: No, not all fractures require surgery. Non-displaced fractures are often treated conservatively, while displaced fractures or those involving significant displacement may necessitate surgical intervention.
Q: How long will it take to return to normal activities?
A: Recovery times vary but typically range from 6 to 12 weeks for non-displaced fractures. Full recovery and return to sports may take longer, depending on the nature of the fracture and rehabilitation progress.
Q: Are there any long-term effects of a clavicular fracture?
A: Most individuals recover fully without long-term complications. However, some may experience residual pain or reduced strength in the shoulder. Engaging in a comprehensive rehabilitation program can help mitigate these risks.
Q: What should I do if I suspect a clavicular fracture?
A: Seek medical attention immediately. A healthcare professional can provide an accurate diagnosis and develop a treatment plan tailored to your needs. By understanding clavicular fractures and their recovery process, individuals can better navigate their healing journey and take proactive steps to prevent future injuries. Always consult with healthcare professionals to ensure the best outcomes during recovery and rehabilitation.
If you would like to start you post-fracture rehab at Triangle Physiotherapy, contact us today to schedule a physiotherapy appointment.
Vaginismus is a condition often misunderstood and sometimes left undiagnosed due to lack of awareness or stigma. Lets demystify vaginismus by addressing the most frequently asked questions, including symptoms, causes, diagnosis, and effective treatments. Whether you’re seeking help for yourself or someone you know, understanding vaginismus is the first step toward finding relief and support. The pelvic health physiotherapists at Triangle Physiotherapy can help you overcome this condition and regain your quality of life.
1. What Is Vaginismus?
Vaginismus is a condition where involuntary muscle contractions occur around the vaginal opening, making penetration painful or even impossible. This muscle response can be triggered by physical or psychological factors and often interferes with intimate activities, tampon use, and even gynecological exams.
2. What Are the Symptoms?
- Pain or discomfort during penetration
- Burning, stinging, or tightness in the pelvic area
- Difficulty with vaginal penetration, such as tampon use or gynecological exams
- Anticipation of pain before intimacy due to past experiences
3. What Causes Vaginismus?
Previous painful intercourse or other experiences that create a conditioned response in the muscles
- Anxiety or fear of pain
- Trauma or past experiences, such as sexual abuse
- Certain medical conditions, infections, or hormonal imbalances
- Lack of awareness or knowledge about the condition
4. How common is it?
Although exact prevalence is hard to determine, vaginismus is not uncommon. Many people don’t seek help due to embarrassment or misconceptions, but it is estimated that a significant number of people with vaginas experience some form of pelvic pain or vaginismus at some point.
5. What is the difference between primary and secondary Vaginismus?
Primary Vaginismus
• sexually inexperienced
• penetration problem apparent at first attempt
• sexual penetration may seem physically impossible
• unconsummated couples
• sometimes difficulty inserting tampons/undergoing pelvic exam
Secondary Vaginismus
• sexually experienced
• previously normal sex life
• ongoing vaginal tightness, discomfort, pain with intercourse
• usually precipitated by medical condition, menopause, traumatic event, childbirth, surgery, etc.
• sometimes difficulty with pelvic exam
6. Is there a treatment for Vaginismus?
Vaginismus can be a challenging condition to manage. While exercises and stretches done at home are helpful, additional support may be necessary.
That’s where pelvic floor physiotherapy comes in.
A pelvic health physiotherapist can help you to:
- Offer personalized guidance on pelvic floor exercises for managing vaginismus.
- Identify any pelvic floor dysfunctions.
- Learn specific exercises to strengthen the pelvic floor muscles.
- Practice targeted stretches to relax essential areas.
- Address symptoms such as incontinence, constipation, pelvic pain, prolapse, and others.

While vaginismus can be a challenging condition, there is hope and help available. Seeking support from qualified professionals and understanding treatment options can lead to meaningful improvement. Remember, vaginismus is a common issue, and addressing it openly is the first step toward reclaiming comfort and confidence. Book an appointment with one of our pelvic health physiotherapists in Mississauga, Oakville or Toronto to get help today!
Here are links to studies and articles that discuss the prevalence of vaginismus and the effectiveness of pelvic floor therapy as a treatment:
- Reissing et al.’s study on pelvic floor physical therapy in lifelong vaginismus, which provides insights into patient experiences and therapy outcomes, including reductions in pain and improved quality of life. This research suggests that pelvic floor therapy can be effective, particularly with a tailored approach involving manual techniques and education. You can access it hereRead by QxMD.
- For further context on the prevalence of vaginismus and other sexual dysfunctions, look into studies by Miller et al., which highlight pelvic floor disorders in U.S. women and treatment options.
In today’s world, more people are turning to holistic approaches to health and wellness. Naturopathic medicine emphasizes natural remedies and the body’s inherent ability to heal itself. The Naturopaths at Triangle Physiotherapy can do a detailed initial assessment of your health and provide a treatment plan that can help you live a healthy life.
Here are five compelling reasons to consider visiting a naturopathic doctor.
1. Personalized Healthcare Approach
One of the primary benefits of seeing a naturopathic doctor is the personalized approach to healthcare. Naturopaths take the time to understand your unique health history, lifestyle, and goals. This comprehensive assessment allows them to create tailored treatment plans that address not just symptoms but the root causes of your health issues.
Unlike conventional medicine, which often relies on standardized treatments, naturopathy emphasizes individualized care. This means you’re more likely to receive a treatment plan that resonates with your specific needs, helping you achieve optimal health in a way that feels right for you.
2. Focus on Prevention
Naturopathic doctors prioritize prevention over merely treating symptoms. They educate patients on lifestyle choices that can help prevent illness and promote long-term health. This proactive approach includes guidance on nutrition, stress management, exercise, and sleep hygiene.
By focusing on prevention, naturopathic doctors help you build a strong foundation for wellness, reducing the risk of chronic diseases and other health issues down the line. They empower you to take control of your health, fostering a sense of well-being and resilience.
3. Integration of Natural Therapies
Naturopathic medicine is rooted in the use of natural therapies to promote healing. Naturopathic doctors utilize a variety of modalities, including herbal medicine, homeopathy, acupuncture, and nutrition. These therapies work in harmony with the body, often with fewer side effects than conventional medications.
For those seeking alternatives to pharmaceutical drugs, naturopathy offers a wealth of natural options. Whether you’re dealing with digestive issues, hormonal imbalances, or chronic pain, a naturopathic doctor can help you explore safe and effective natural treatments.
4. Support for Chronic Conditions
Many individuals struggle with chronic health conditions that don’t seem to improve with traditional treatments. Naturopathic doctors are skilled at addressing these complex issues. They look at the whole person—mind, body, and spirit—considering how factors like stress, nutrition, and lifestyle contribute to your condition.
Whether you’re dealing with conditions like diabetes, autoimmune disorders, or anxiety, a naturopathic doctor can help create a comprehensive plan that addresses your unique challenges. By focusing on healing the body as a whole, you may find more effective relief and improved overall health.
5. Empowerment and Education
Finally, seeing a naturopathic doctor empowers you to take an active role in your health. Naturopathic practitioners emphasize education, providing you with the knowledge and tools to make informed decisions about your well-being.
This collaborative approach fosters a strong doctor-patient relationship, where you’re encouraged to ask questions and participate in your health journey. As you learn about your body and how to care for it, you gain confidence in making choices that promote your wellness.
visiting a naturopathic doctor offers a personalized, preventive, and holistic approach to health. With their focus on natural therapies and empowerment, naturopaths can guide you toward a healthier, more balanced life. If you’re looking for an alternative to conventional medicine or seeking support for chronic conditions, consider reaching out to a naturopathic doctor. Your path to wellness may just begin with a visit to one.
Click HERE to learn more about what a Naturopathic doctor can do for your health.
When it comes to therapeutic massage, two popular techniques often come up: sports massage and deep tissue massage. While they share some similarities, they serve different purposes and are designed for distinct needs. Understanding the nuances between the two can help you choose the right massage for your goals, whether you’re an athlete or simply seeking relief from tension. The massage therapists at Triangle Physiotherapy use techniques that can target the muscles to help reduce your pain and improve your ability to play the sports you love as well as enhance your well-being.
Understanding the Techniques

Sports Massage
Sports massage is specifically tailored for athletes, focusing on enhancing performance, preventing injuries, and aiding recovery. It incorporates various techniques to address the specific needs of athletes at different stages of training and competition. Whether you’re preparing for a big race or recovering from a strenuous workout, sports massage can be a valuable addition to your routine.
Deep Tissue Massage
Deep tissue massage, on the other hand, is a broader technique that targets the deeper layers of muscle and connective tissue throughout the body. It aims to alleviate chronic pain, tension, and stiffness by applying sustained pressure on targeted areas. While deep tissue massage can benefit anyone, it’s particularly effective for those who experience long-term muscle tension or discomfort.
Key Differences
Purpose and Focus
The primary difference between sports and deep tissue massage lies in their purpose. Sports massage is focused on improving athletic performance and recovery, using techniques tailored to the athlete’s specific needs. It may involve stretching, trigger point therapy, and even techniques to stimulate blood flow.
Conversely, deep tissue massage targets specific areas of chronic pain and tension. It works through layers of muscle and fascia to release knots and relieve tightness, making it ideal for individuals dealing with ongoing discomfort rather than performance enhancement.
Techniques Used
Both massages utilize pressure and manipulation, but the techniques may vary significantly. Sports massage often employs:
- Compression techniques: To stimulate circulation and reduce muscle soreness.
- Stretching: To improve flexibility and range of motion.
- Cross-fiber friction: To break down scar tissue and promote healing.
Deep tissue massage, in contrast, focuses on:
- Slow, deep strokes: To reach the deeper layers of muscle.
- Pressure points: To release tension in specific areas, often requiring more intensity.
- Kneading: To work out knots and alleviate chronic tightness.
Ideal Recipients
Sports massage is primarily designed for athletes or active individuals who engage in regular physical activity. It’s beneficial before events to prepare muscles or after workouts to speed recovery. Athletes of all levels, from recreational runners to professional players, can gain from this specialized approach.
Deep tissue massage, however, is suitable for anyone experiencing chronic pain or tension, regardless of their activity level. It’s often recommended for individuals who sit for long periods, have physically demanding jobs, or suffer from conditions like arthritis or fibromyalgia.
FAQs
Can I get a sports massage if I’m not an athlete?
Absolutely! Sports massage can benefit anyone with muscle tension or who engages in physical activities, regardless of their athletic level.
Is deep tissue massage painful?
Deep tissue massage can be intense, especially if you have significant muscle tension. However, communication with your therapist can help manage discomfort.
How often should I get a massage?
The frequency of massage depends on individual needs and goals. Athletes might benefit from more frequent sessions, while those seeking relief from chronic pain may require regular visits to maintain comfort.
Can I use both types of massage?
Yes! Many people find that incorporating both sports and deep tissue massage into their routine addresses different needs effectively.
Choosing between sports massage and deep tissue massage ultimately depends on your individual needs and goals. While sports massage focuses on performance and recovery for athletes, deep tissue massage aims to alleviate chronic tension and discomfort for a broader audience. Understanding these differences can help you select the most beneficial approach for your well-being, ensuring you receive the right care for your body. Whether you’re looking to enhance your athletic performance or simply unwind from daily stresses, both techniques offer unique advantages that can enhance your overall health.
Looking for a Massage Therapist? Call or book your appointment online.
Triangle Physiotherapy has 8 locations in the Greater Toronto Area with registered massage therapists that can help you perform at your best! Book your Appointment today!
References:
https://www.physio-pedia.com/Rehabilitation_in_Sport
https://www.physio-pedia.com/Massage













