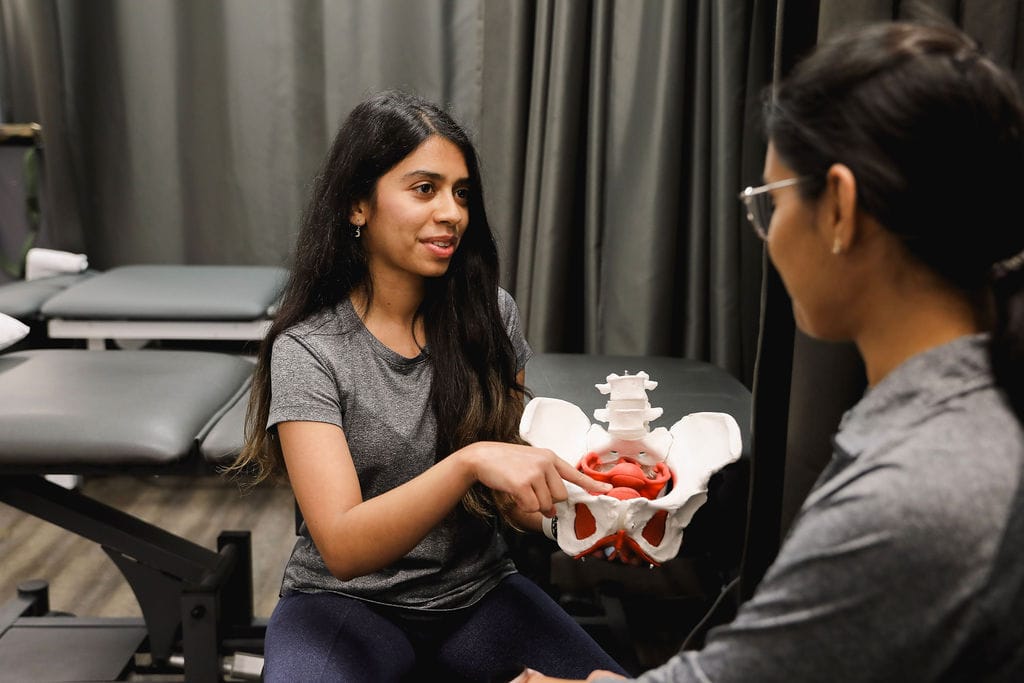
When it comes to women’s health, two conditions often mentioned together are Polycystic Ovary Syndrome (PCOS) and Endometriosis. While both can impact fertility and overall well-being, they are distinct conditions with different causes, symptoms, and treatments. The pelvic health physiotherapists at Triangle Physiotherapy help us break down the key differences to help you better understand them.
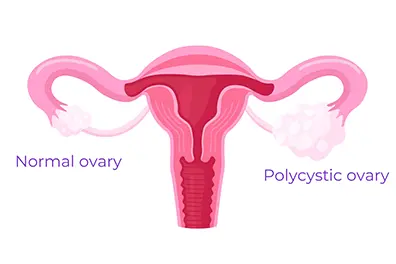
What is PCOS?
Polycystic Ovary Syndrome (PCOS) is a hormonal disorder that affects how the ovaries function. It is one of the most common endocrine disorders among women of reproductive age.
Common Symptoms of PCOS:
- Irregular or Absent Periods: Due to hormonal imbalances, women with PCOS often experience infrequent or prolonged menstrual cycles.
- Excess Hair Growth and Acne: Elevated levels of androgens (male hormones) can lead to hirsutism (excess facial and body hair), acne, and even hair thinning on the scalp.
- Insulin Resistance: Many women with PCOS struggle with insulin resistance, which can increase the risk of type 2 diabetes.
- Ovarian Cysts: Despite its name, not all women with PCOS have cysts on their ovaries, but some may develop multiple small fluid-filled sacs.
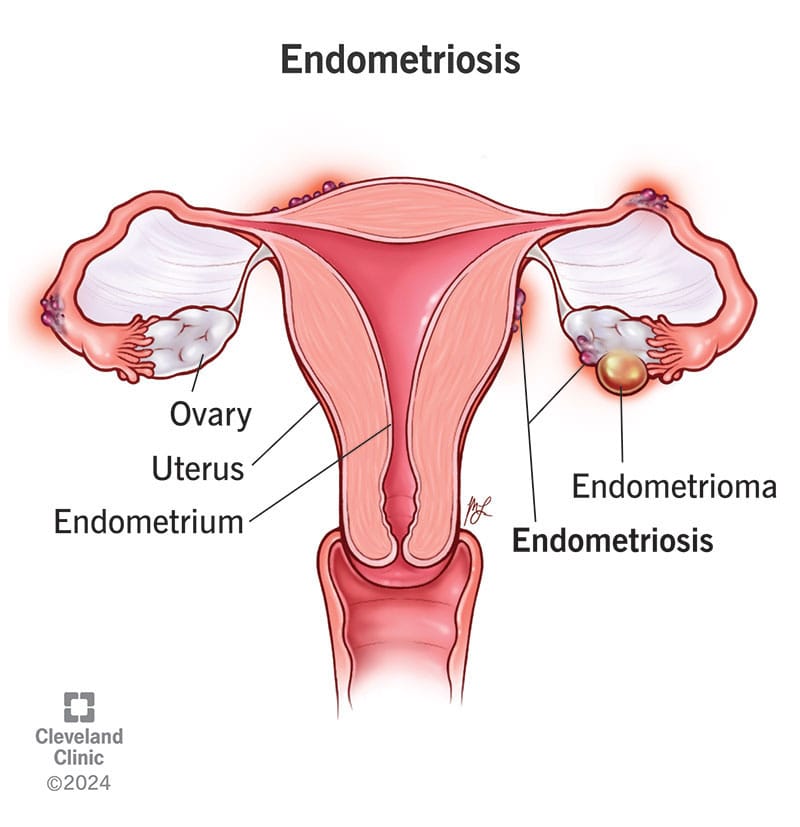
What is Endometriosis?
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside of it, leading to inflammation, scarring, and pain.
Common Symptoms of Endometriosis:
- Severe Menstrual Cramps: One of the hallmark symptoms of endometriosis is intense pelvic pain that can start before and last beyond the menstrual cycle.
- Heavy Periods: Women with endometriosis often experience unusually heavy menstrual bleeding.
- Pain During Intercourse: Pain during or after sex is a common complaint due to the presence of endometrial-like tissue outside the uterus.
- Chronic Pelvic Pain: Many women with endometriosis experience ongoing pelvic discomfort, even outside their periods.
Key Differences Between PCOS and Endometriosis
| Feature | PCOS | Endometriosis |
|---|---|---|
| Cause | Hormonal imbalance | Endometrial-like tissue growing outside the uterus |
| Periods | Irregular or absent | Heavy and painful |
| Pain | Not always present | Severe pelvic pain |
| Fertility Impact | May cause ovulation issues | May lead to scarring and blockages |
| Hormonal Symptoms | Excess androgens (acne, hair growth) | Usually no androgen-related issues |
How Are PCOS and Endometriosis Treated?
Since these conditions have different causes, their treatments also vary:
- PCOS Treatment: May involve hormonal birth control, lifestyle changes, insulin-sensitizing medications (like Metformin), and fertility treatments if pregnancy is desired.
- Endometriosis Treatment: Can include pain management (NSAIDs), hormonal therapy (such as birth control or GnRH agonists), and in severe cases, surgery to remove endometrial-like tissue.
The Bottom Line
Both PCOS (Polycystic Ovary Syndrome) and Endometriosis are complex conditions that need personalized treatment. If you notice symptoms of either, it’s important to talk to a healthcare provider to get the right diagnosis and treatment plan.
Along with medical care, adding Physiotherapy Oakville can also help. Physiotherapy can ease pelvic pain, improve movement, and reduce muscle tension caused by these conditions. It supports your overall well-being and helps you feel better over time.
By combining medical advice and physiotherapy, you can manage symptoms more effectively and improve your quality of life.
💬 Do you or someone you know struggle with these conditions? Let’s continue raising awareness and supporting women’s health! 💙
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
After menopause, women face an increased risk of knee injuries due to hormonal changes, decreased muscle strength, and other age-related factors. These changes, combined with weight gain and joint instability, can make the knees more vulnerable. However, with the right prevention strategies, knee injuries can be minimized, allowing you to stay active and pain-free. Give us a call at one of our Toronto locations and our physiotherapists at Triangle Physiotherapy can help you.
What Causes Knee Injuries in Post-Menopausal Women?
Several factors contribute to knee injuries in post-menopausal women, including:
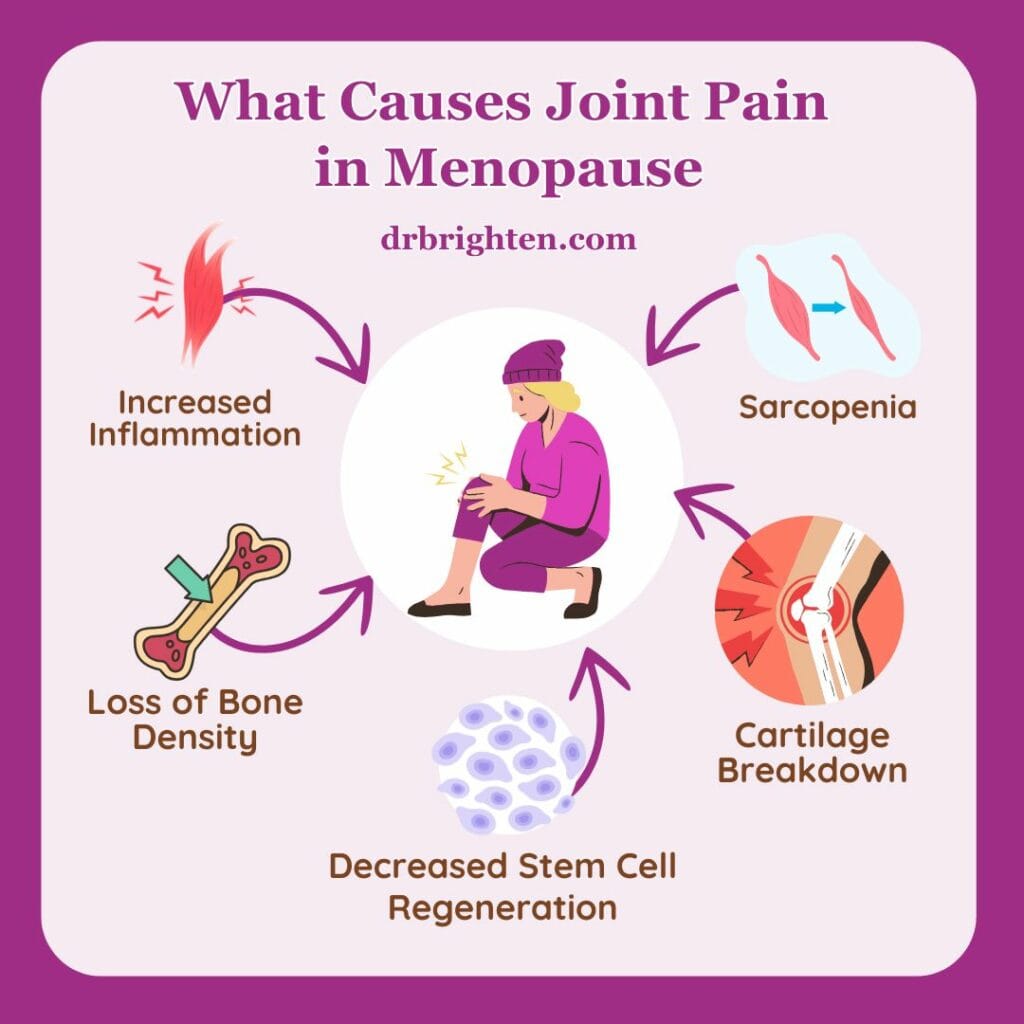
- Hormonal Changes: The drop in estrogen after menopause can weaken bones, muscles, and ligaments, increasing the risk of knee injuries.
- Muscle Weakness: Aging leads to a natural decline in muscle mass, which weakens the muscles surrounding the knee, leaving it less supported.
- Joint Instability: Weakened muscles and bones contribute to joint instability, making the knee more prone to sprains, strains, and tears.
- Weight Gain: Many women gain weight after menopause, which places added stress on the knee joints, leading to pain and increasing the risk of conditions like osteoarthritis.
Common Knee Injuries Post-Menopause
Some of the most common knee injuries women face include:
- Osteoarthritis: A condition where the knee’s cartilage wears down, causing pain and stiffness.
- Patellofemoral Pain Syndrome: Pain around the kneecap often caused by overuse or poor alignment.
- Ligament Injuries: Sprains or tears in the knee’s ligaments, such as the ACL or MCL, from sudden movements or falls.
- Tendonitis: Inflammation of the tendons, usually due to overuse or muscle imbalances.
Preventing Knee Injuries
Here are some essential physiotherapy tips to help prevent knee injuries post-menopause:
- Strengthen Muscles Around the Knee: Build strength in the quadriceps, hamstrings, and calves through exercises like squats and lunges to support the knee joint.
- Maintain a Healthy Weight: Extra weight adds stress to the knees, so managing weight through diet and exercise can reduce knee strain.
- Increase Mobility: Stretching the quadriceps, hamstrings, and calves can prevent tightness, but having overall mobility helps keep the joints healthy.
- Low-Impact Exercises: Activities like swimming, cycling, or walking are easier on the knees while still strengthening muscles and improving cardiovascular health.
- Strengthen Core and Hips: Strong core and hip muscles improve overall stability, reducing strain on the knees.
- Wear Supportive Footwear: Shoes with proper arch support and cushioning can reduce stress on the knees, especially during physical activities.
- Use Proper Technique: Ensure correct form when exercising, lifting, or performing daily tasks to avoid unnecessary stress on the knees.
- Balance Exercises: Improve stability and prevent falls with exercises that challenge balance, such as standing on one leg.
Managing Knee Injuries
If knee pain or injury occurs, here are some strategies for managing it:
- Physiotherapy: A physiotherapist can design a program to improve strength, flexibility, and mobility, helping you recover and prevent further injury.
- Braces or Sleeves: Knee supports can provide stability and reduce pain during activity.
Conclusion
Post-menopausal women are at higher risk for knee injuries, but with proactive care, the risk can be minimized. Strengthening the knee muscles, maintaining a healthy weight, and practicing good form are key to keeping your knees healthy. If knee pain occurs, working with a physiotherapist and using the right treatments can help you stay active and injury-free. Book an appointment with one of the physiotherapists at Triangle Physiotherapy in Toronto to get help today!
Menopause is a fact of life for people who menstruate – periods need to stop eventually! So why don’t we talk about menopause more often? Even when we do talk about it, there seem to be a lot of misconceptions and myths. It’s time to bust them wide open!
1. Menopause symptoms are mostly hot flashes and mood swings
Though it may be true that hot flashes and mood swings are common symptoms of menopause, it is so much more than that! In fact, comprehensive lists of menopausal symptoms have over 100 different symptoms! Our naturopathic doctor and pelvic health physiotherapists at Triangle Physiotherapy can help educate you on the symptoms and their natural management.
2. Menopausal symptoms are unpreventable and a fact of life for all women

Some women have their periods stop without experiencing any symptoms at all! But even if you’re not one of those lucky people, there are things you can do to help this transitional time in your life to be more manageable. Talk to your naturopathic doctor to find out what you can do!
3. During peri-menopause, your periods always get lighter and farther apart
Though this may be true that eventually your periods become lighter and farther apart, it often doesn’t start that way. Many women find that when menopause begins, it’s actually the exact opposite of this. Periods can become more frequent and heavier before they eventually peter out.
4. The only mood changes that happen during menopause are irritability and mood swings
This is one of the most important myths for us to clarify. Yes, it’s true that irritability, anger, and mood swings are all potential symptoms of menopause. But anxiety and depression are part of what can happen during menopause, too. Instead of thinking of a menopausal woman as “cranky and short-tempered”, keep in mind that they may be going through anxiety and depression. Check up on menopausal women, and ensure they have the mental health support they often need at this time.
5. Menopause only happens after age 50
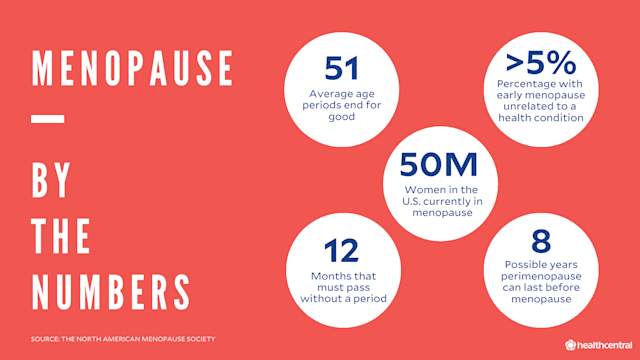
The most common age for menopause to happen is 50, but there is a lot of variance with this. In fact, some women can even go into menopause in their 30’s!
6. A hysterectomy always causes menopause
If you have a total hysterectomy, it is true that you will enter menopause post-surgery. But if your ovaries are not removed, then this isn’t the case. You would go through menopause naturally, and this could happen many years after your hysterectomy.
7. An IUD can cause you to skip over menopause
IUD’s have no impact on when you will go through menopause. What they can do, however, is help to manage some of the bleeding symptoms that can occur along with menopause.
8. Menopause marks the end of a woman’s sex life
Absolutely not! Women can have healthy sex lives well beyond menopause! Some symptoms of declining estrogen levels, such as lower libido and vaginal dryness, may make intercourse more difficult. However, there are natural options that can help to manage these symptoms to make intercourse more pleasurable for you. Be sure to speak to a naturopathic doctor if you would like to explore more of these options. Our pelvic health physiotherapists can also help you navigate the effects menopause can have on your sex life.
9. Menopause lasts a couple of years
It’s usually much longer than this. In fact, menopausal symptoms can begin up to 10 years before your periods actually stop!
10. Men go through menopause too
Nope. You may have heard of “andropause” or “manopause”, which refer to when testosterone levels decline in men. However, this testosterone decline happens very slowly, over several years. In menopause, the hormonal fluctuations are more drastic and happen much more quickly. This is why menopause can cause uncomfortable symptoms.
We hope this helped to clear up some of the common myths out there about menopause. If you have any further questions about menopause or women’s health, reach out to our naturopathic doctor at Triangle Physiotherapy and book an appointment today!
Bloating is a common issue that many of us experience at one point or another. Whether it’s caused by a heavy meal, certain foods, or even stress, feeling bloated can be uncomfortable and frustrating. The good news is that there are plenty of ways to relieve bloating and get back to feeling like yourself.
If you are feeling bloated, the Naturopaths and Acupuncturists at Triangle Physiotherapy are able to assess and find the root cause of your bloating.
In this blog, we’ll share 7 practical tips that can help reduce bloating and improve your digestive health.
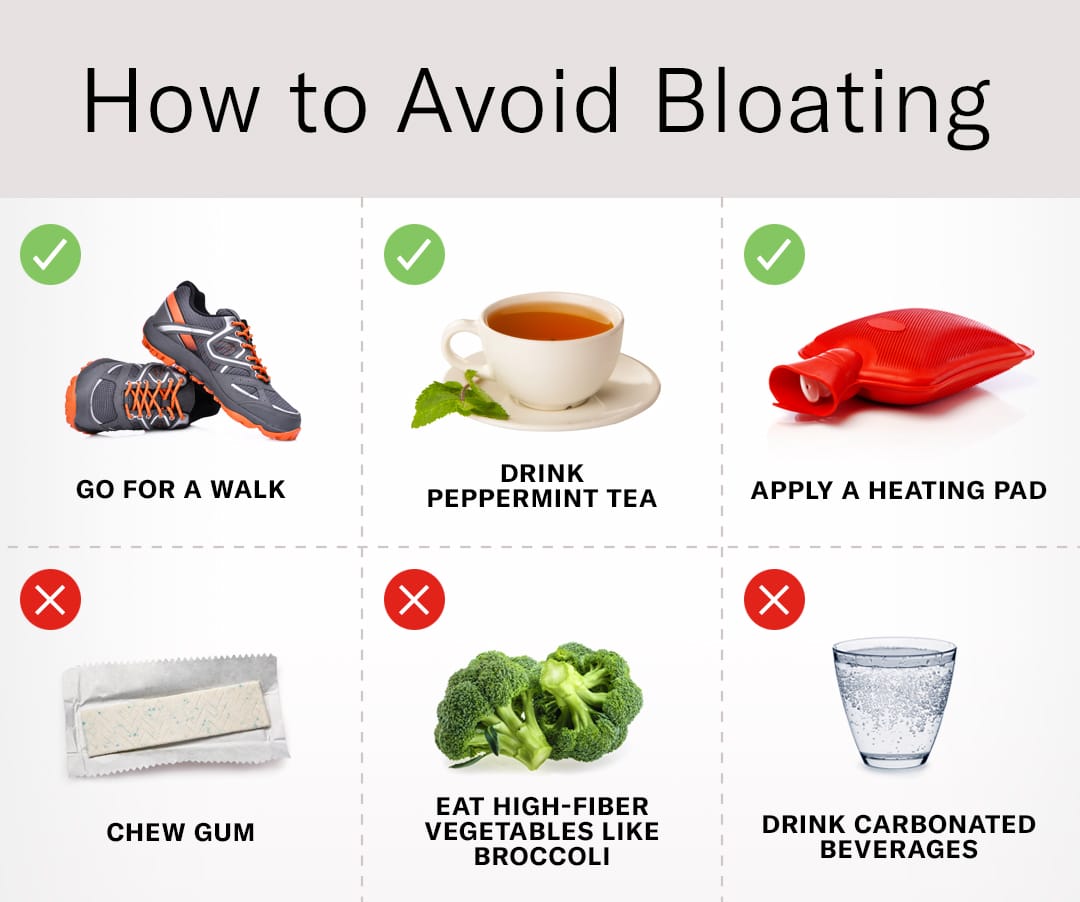
1. Watch What You Eat
Certain foods are known to cause bloating, especially those that are difficult to digest or contain high levels of fiber. While fiber is important for your health, some foods, like beans, lentils, cruciferous vegetables (like broccoli and cauliflower), and dairy, can cause gas and bloating, especially if you’re not used to eating them in large amounts.
- Tip: Try keeping a food journal to track which foods may be causing bloating and experiment with cutting them out for a while. If dairy is an issue, consider switching to lactose-free or plant-based alternatives.
2. Stay Hydrated
It might sound counterintuitive, but drinking more water can actually help reduce bloating. When your body is dehydrated, it can hold on to excess water, leading to that uncomfortable, swollen feeling. Staying hydrated helps to keep your digestive system moving and can prevent water retention.
- Tip: Aim for about 8 glasses of water a day, or more if you’re active. Adding a squeeze of lemon or cucumber can make it more refreshing.
3. Eat Smaller, More Frequent Meals
Large meals can overwhelm your digestive system, leading to bloating and indigestion. Instead of eating three big meals a day, try splitting your meals into smaller, more frequent servings. This helps to regulate your digestive process and prevents excessive bloating after eating.
- Tip: Opt for 4–6 smaller meals throughout the day, and try to eat slowly to give your body time to digest properly.
4. Move Around After Eating
It’s tempting to slump on the couch after a large meal, but sitting still can actually make bloating worse. Moving around gently after eating helps stimulate your digestive system and can ease any discomfort.
- Tip: Go for a short walk after meals to help with digestion. Even a few minutes of movement can do wonders for reducing bloating.
5. Try Probiotics
Probiotics are beneficial bacteria that can help balance the gut microbiome and improve digestion. If your bloating is due to an imbalance of gut bacteria, taking a probiotic supplement or eating probiotic-rich foods like yogurt, kefir, sauerkraut, or kimchi might help ease the symptoms.
- Tip: Start with a mild probiotic and gradually increase your intake to avoid gas or discomfort. Be patient—it can take a few days or even weeks for probiotics to have their full effect.
6. Avoid Carbonated Drinks
The bubbles in carbonated drinks, including soda, sparkling water, and beer, can cause gas to build up in your stomach, leading to bloating. While it’s tempting to grab a fizzy drink, the air trapped in the bubbles can make you feel swollen and uncomfortable.
- Tip: Opt for still water or herbal teas instead. Ginger or peppermint tea can be particularly helpful in soothing your digestive system.
7. Mind Your Stress Levels
Believe it or not, stress can contribute to bloating. When you’re stressed, your body releases hormones that can slow down digestion and cause bloating. Practicing relaxation techniques like deep breathing, meditation, or yoga can help reduce stress and alleviate bloating.
- Tip: Try setting aside time each day for a short relaxation practice, even if it’s just 5–10 minutes of mindful breathing or stretching.
FAQs About Bloating
Q: Can I prevent bloating altogether?
While it’s not always possible to completely prevent bloating, you can reduce the frequency and severity by paying attention to your diet, staying hydrated, and managing stress. If you consistently experience bloating, it might be a good idea to consult with a healthcare professional to rule out underlying conditions like food intolerances or gastrointestinal disorders.
Q: Is bloating a sign of a serious health problem?
In most cases, bloating is a normal part of digestion and isn’t a cause for concern. However, if bloating is persistent, painful, or accompanied by other symptoms like significant weight loss, diarrhea, or vomiting, it could indicate an underlying health condition such as IBS (Irritable Bowel Syndrome), celiac disease, or a digestive disorder. It’s best to seek medical advice if you’re worried.
Q: What can I do if I feel bloated after every meal?
If bloating occurs after every meal, it could be related to how you’re eating, what you’re eating, or how your body is processing food. Try eating smaller meals, chewing your food thoroughly, and avoiding foods that cause gas. If the issue persists, consider keeping a food diary and discussing it with a healthcare provider or dietitian.
Q: Are there any natural remedies for bloating?
Yes! Several natural remedies may help relieve bloating, including:
- Ginger: Known for its digestive properties, ginger can help soothe the stomach.
- Peppermint tea: Helps to relax the digestive muscles and reduce bloating.
- Fennel seeds: Can help reduce gas and bloating when chewed or steeped in hot water.
Bloating is an issue that the Naturopaths and Acupuncturists at Triangle Physiotherapy can help you with. Book an appointment today!
Undergoing any type of surgery can be a daunting experience, especially when you are dealing with pain or discomfort in the lead-up to the procedure. For many patients, managing pain before surgery can be as crucial as the surgery itself, both in terms of improving the surgical outcome and enhancing recovery. Physiotherapy is an essential part of this pre-surgical care, providing strategies to manage pain, improve mobility, and prepare the body for the challenges of surgery and rehabilitation. The highly trained physiotherapists at Triangle Physiotherapy can advise you on strategies on managing pain before surgery and how it can help you feel stronger, more comfortable, and better equipped for recovery.
What is Pre-Surgical Physiotherapy?
Pre-surgical physiotherapy, often referred to as “prehabilitation,” is the practice of preparing the body before surgery through a series of targeted exercises, education, and therapies. The goal is to improve physical fitness, increase mobility, and reduce pain prior to undergoing surgery. By strengthening muscles, improving joint mobility, and reducing stress on affected areas, prehabilitation can make the body more resilient during the recovery process and even reduce the risk of complications after surgery.

The Importance of Managing Pain Before Surgery
Chronic pain, whether from conditions like arthritis, injuries, or musculoskeletal disorders, can be overwhelming and can negatively affect the body’s ability to heal post-surgery. Pre-surgical pain management is not just about addressing discomfort; it’s about setting the stage for a smoother recovery. Here’s why it’s essential to manage pain before surgery:
- Reducing the Impact of Surgery on the Body
Chronic pain can weaken muscles and joints, affecting overall mobility. If these issues are not addressed before surgery, they can impede recovery, increase stress on the surgical site, and lengthen the rehabilitation process. By managing pain pre-operatively, you can make the body more capable of handling the stresses of surgery. - Improved Post-Surgical Outcomes
Research has shown that patients who engage in pre-surgical physiotherapy tend to have better outcomes following surgery. They often experience reduced pain post-operation, faster healing, and a quicker return to normal activities. - Preventing Muscle Atrophy and Stiffness
When dealing with long-term pain, it’s common to limit movement in order to avoid discomfort. This inactivity can lead to muscle atrophy (weakening) and joint stiffness. Physiotherapy helps maintain and even improve strength and flexibility before surgery, ensuring the body is in the best possible condition for a smooth recovery.
How Physiotherapy Can Help Manage Pain Before Surgery
Physiotherapists are experts in movement and pain management, and they can develop tailored treatment plans that address the specific needs of each individual. Here’s how physiotherapy can help manage pain before surgery:
- Pain Relief Techniques
Physiotherapists use a variety of manual therapy techniques to reduce pain and improve joint function. These may include:- Massage therapy to relax muscles and reduce tension.
- Joint mobilizations to increase range of motion and alleviate stiffness.
- Myofascial release to address tightness and discomfort in the soft tissues.
- These techniques can help reduce the intensity of pain, making it easier to engage in exercises and movements that promote healing.
- Strengthening Exercises
Weak muscles can contribute to pain and difficulty moving. Physiotherapists can develop a customized exercise program to strengthen muscles around the affected joints, improving stability and reducing the strain on pain-prone areas. Strengthening key muscle groups ensures that the body is well-prepared for the demands of surgery and recovery. - Mobility and Flexibility Training
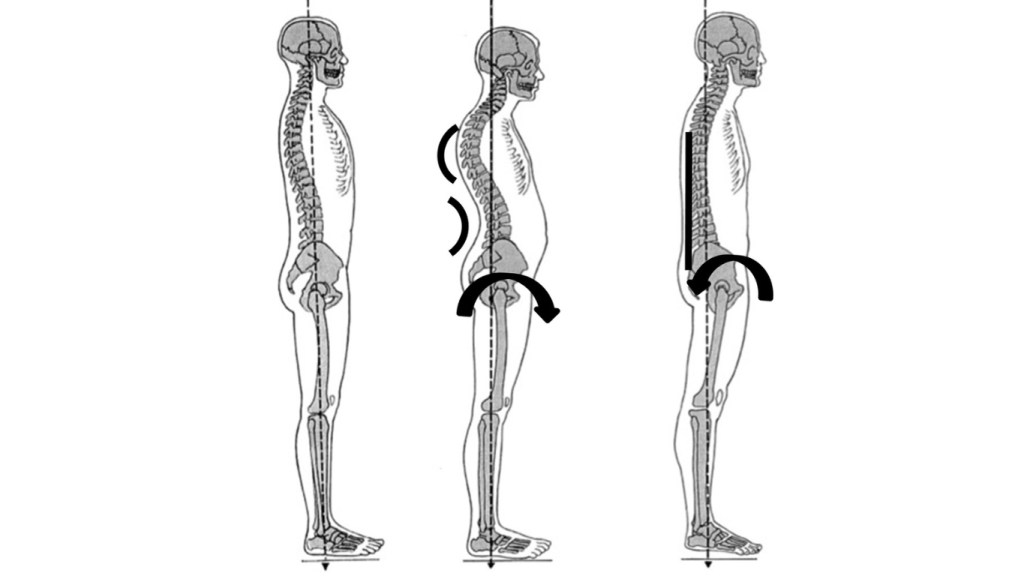
Stiffness in the joints and muscles can exacerbate pain and hinder movement. Physiotherapists incorporate stretching and flexibility exercises into pre-surgical programs to improve range of motion. Whether it’s the hips, knees, or shoulders, increasing flexibility can reduce discomfort and prevent further limitations, allowing for better post-surgical rehabilitation. - Postural Correction
Poor posture can put additional strain on joints and muscles, exacerbating pre-existing pain. Physiotherapists assess your posture and provide education on how to align your body correctly during daily activities. Proper posture can prevent unnecessary pressure on joints and muscles, reducing pain and discomfort before surgery. - Education and Pain Management Strategies
Physiotherapists teach patients how to manage pain more effectively through techniques like breathing exercises, mindfulness, and relaxation strategies. Additionally, they may provide advice on managing pain at home, such as the use of heat or cold therapy and ergonomic adjustments in daily activities.
When Should You Seek Pre-Surgical Physiotherapy?
If you’re preparing for surgery and are experiencing pain, stiffness, or limited mobility, it’s a good idea to seek physiotherapy before your procedure. The sooner you begin prehabilitation, the better the results. Ideally, pre-surgical physiotherapy should begin a few weeks to months before the surgery date. However, even if you’re closer to your surgery, starting physiotherapy as soon as possible can still provide significant benefits.
Where can I find a Pre-Surgical Physiotherapy clinic in Oakville?
Triangle Physiotherapy has 8 locations in the GTA, with a physiotherapy clinic in Oakville, located at 2501 Prince Michael Drive, Oakville ON L6H7V6.
Book your prehabilitation appointment today to ensure you get the best outcomes from your surgery.
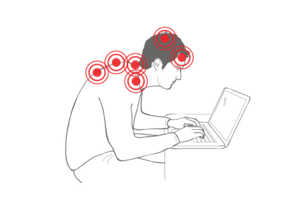
In today’s digital age, it’s hard to avoid spending long hours staring at screens, whether it’s for work, social media, or entertainment. Unfortunately, this extended screen time can often lead to neck pain, commonly known as “tech neck” or “text neck”. Tech neck refers to the discomfort or pain caused by poor posture when using digital devices, such as smartphones, tablets, and computers. The good news is that with a few simple physiotherapy tips, you can reduce the risk of developing tech neck and promote better posture.
The physiotherapists at Triangle Physiotherapy can help you with the neck pain that is associated with extended use of digital devices.
What Causes Neck Pain from Digital Devices?
The main culprit behind neck pain associated with digital devices is poor posture. When we use our devices, we often find ourselves slouching or looking down for extended periods, which places unnecessary strain on the neck muscles and spine. Over time, this repetitive motion can lead to muscle tension, discomfort, and even long-term damage.
Several factors contribute to this issue, including:
- Forward head posture: When you lean your head forward to look at your device, the muscles in the neck and upper back work harder to hold your head in position, leading to strain.
- Slouching: Sitting or standing with a rounded back and shoulders can cause the neck to overcompensate, increasing pressure on the muscles and joints.
- Screen height and distance: If your screen is too low or too far from your eyes, it forces you to look down or strain your neck to see clearly.
Common Symptoms of Tech Neck from Screen Use
Neck pain related to digital devices can present itself in various ways, including:
- Stiffness and soreness: You may notice tightness in your neck, shoulders, or upper back after using your devices for extended periods.
- Headaches: Tension in the neck muscles can trigger headaches, particularly around the base of the skull.
- Pain with movement: You might feel discomfort or limited mobility when trying to turn your head or tilt your neck.
- Numbness or tingling: In some cases, pressure on the nerves in the neck can cause sensations of numbness or tingling in the arms or hands.
How to Prevent Neck Pain from Digital Devices
The good news is that neck pain from digital devices can be prevented with some mindful changes to your posture and daily habits. Here are a few physiotherapy tips to help you avoid tech neck:
- Maintain Proper Posture: Always aim to keep your head aligned with your spine. Your ears should be over your shoulders, and your shoulders should be back, not hunched forward. Keep your screen at eye level to avoid tilting your head downward.
- Take Regular Breaks: Avoid sitting in the same position for too long. Follow the 20-20-20 rule: every 20 minutes, take a 20-second break and look at something 20 feet away to give your eyes and neck a break.
- Use Ergonomic Setups: Set up your workstation so that your screen is at eye level, and your chair provides proper lumbar support. If you’re using a phone or tablet, consider holding it at eye level or using a stand to prevent looking down.
- Stretch and Strengthen: Incorporate neck and shoulder stretches into your daily routine to relieve tension and promote flexibility. Strengthening exercises for the upper back can also improve posture and support the neck muscles.
- Adjust Screen Time: Reducing the amount of time spent on screens can help lower your risk of neck pain. If you’re working long hours on a computer, try to schedule breaks to move and stretch regularly.
- Stay Hydrated: Dehydration can make muscles more prone to stiffness. Drinking plenty of water can help keep your muscles healthy and prevent tightness.
Treatment for Neck Pain from Digital Devices
If you’re already experiencing neck pain, there are several treatment options available to help alleviate discomfort:
- Physiotherapy: A physiotherapist can assess your posture, identify any muscle imbalances, and recommend specific exercises to strengthen and stretch the muscles that support your neck.
- Massage Therapy: A massage therapist can help release tightness in the neck and upper back muscles, providing relief from tension.
- Hot or Cold Therapy: Applying a warm compress or ice pack to the neck can help reduce inflammation and ease muscle stiffness.
Preventing Text Neck Long-Term
To prevent recurring neck pain, it’s essential to incorporate good posture habits into your daily routine and practice regular stretches and strengthening exercises. Additionally:
- Avoid prolonged screen use: Try to limit the amount of time you spend hunched over devices, especially for tasks that require sustained focus.
- Optimize your workspace: Ensure your desk, chair, and screen setup are ergonomically sound to support good posture.
- Move frequently: Avoid sitting for extended periods without changing positions or stretching.
Neck pain from digital devices is a growing concern, but with the right prevention strategies, it’s entirely possible to avoid or minimize discomfort. By being mindful of your posture, taking regular breaks, and incorporating stretches and strengthening exercises into your routine, you can protect your neck and enjoy your screen time without the pain. If you’re already experiencing neck pain, consider consulting with a physiotherapist to develop a treatment plan that will get you back to feeling your best.
Pediatric physiotherapy is not just about exercises and movements – it’s about making therapy engaging and enjoyable for children. When kids are involved in playful activities, they don’t realize they’re doing therapy, and that’s the magic of it. Here’s how our pediatric physiotherapists at Triangle Physiotherapy incorporate play into physiotherapy to make the experience an exciting adventure for kids.

How Does Play Help in Physiotherapy?
Play is a child’s natural language, and incorporating it into physiotherapy creates a familiar, relaxed environment. It encourages children to engage, reducing the stress or fear they may have about the process. Activities like jumping, running, or even pretend play can help children improve strength, flexibility, and coordination – all while having a blast! For example, hopping over colorful cones can work on leg strength, while throwing soft balls can improve hand-eye coordination. The goal is to blend movement with fun!
When Is Play Incorporated into Pediatric Physiotherapy?
Play is used throughout a physiotherapy session, from the very start to the very end. At the beginning, it can help break the ice and make the child feel comfortable. Mid-session, it helps keep the child motivated and energized. At the end, playful challenges like racing to the finish line or earning “therapy points” can make the experience rewarding. The timing of play depends on the child’s energy levels and interests, ensuring that therapy never feels like a chore.
What Kinds of Play Are Used?
The types of play can vary based on the child’s age, abilities, and therapy goals. Here are some examples:
- Active Play: Running, jumping, climbing, or dancing to a favorite song, all while focusing on improving motor skills.
- Imaginative Play: Pretend scenarios where the child may “rescue” toys or explore new worlds, helping with balance and flexibility. Sensory Integration (SI) is also a great treatment tool for kids.
- Games: Simple games like “Simon Says,” musical chairs, or obstacle courses, which focus on coordination and body awareness.
Where Does Play Fit into Pediatric Physiotherapy?
Play can happen anywhere! Whether it’s at a clinic, at home, or even outdoors, physiotherapists can adapt play to fit the setting. For example, a playground can be the perfect place for a fun session focused on balance and strength. When kids are having fun, they don’t even realize how much they’re improving!

Fun Fact: Kids Have Fun, and It Helps Them Heal Faster!
Did you know that children who enjoy their physiotherapy sessions are more likely to keep practicing their exercises at home? This leads to better recovery outcomes and quicker progress.
Incorporating play into pediatric physiotherapy doesn’t just make the session fun; it also helps children build crucial physical skills without even realizing it. By engaging children through play, physiotherapists create an environment that fosters healing, growth, and development, turning therapy into something they look forward to instead of dread. So, the next time your child has a physiotherapy session, know that play is the secret ingredient to making it both effective and enjoyable!
If you think your child might benefit from Pediatric Physiotherapy get in touch with us and we can book an appointment for you and your little one to get an assessment!
Axillary Web Syndrome (AWS) is a condition that often affects individuals who have undergone breast cancer treatments, particularly those who have had axillary lymph node dissection (ALND) or radiation therapy. This condition, also known as “cording,” involves the development of tight bands or cords of tissue in the armpit area, which can extend down the arm, causing pain and restricting movement. Though it is a common aftereffect of breast cancer treatment, AWS is not always well understood. In this blog, we’ll explore what AWS is, its symptoms, how it affects daily life, and how physiotherapy can help manage the condition.
If you have more questions about Axillary Web Syndrome, the cancer rehab physiotherapists at Triangle Physiotherapy would be more than happy to help you out.
What is Axillary Web Syndrome?
AWS occurs when tight bands of tissue, or “cords,” form under the skin in the armpit (axilla) and sometimes along the upper arm. These bands are typically made of scar tissue or fibrosis that develops after the removal of lymph nodes or following radiation therapy, both of which are common treatments for breast cancer. These tight bands can cause significant discomfort, limit the range of motion, and affect daily activities, such as reaching, lifting, or even carrying objects.
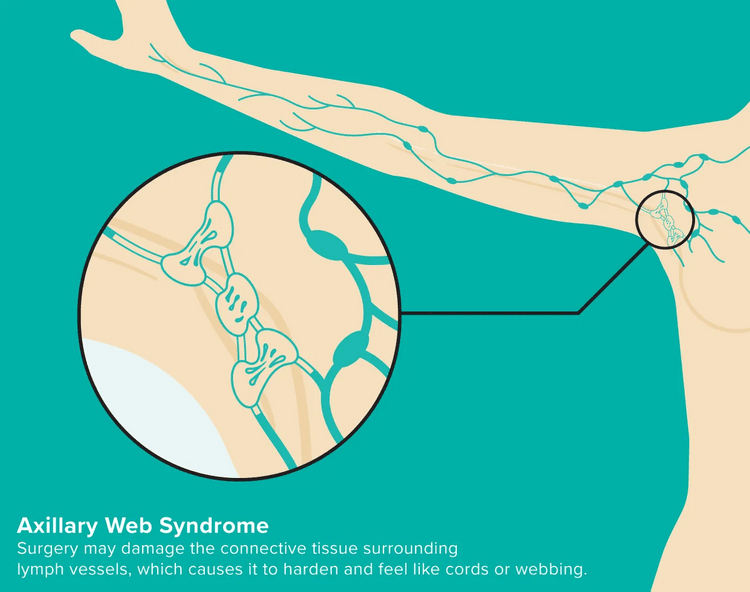
Picture Credit: healthline.com
AWS is usually diagnosed when the cords are palpated (felt) by a healthcare professional during a physical exam. In some cases, individuals may notice the bands themselves or feel a pulling sensation in the arm or chest.
Symptoms of AWS
The most noticeable symptom of AWS is the formation of tight, rope-like cords in the armpit area, but other symptoms may include:
- Pain: The cords can be painful to the touch and can cause discomfort during everyday activities.
- Restricted Mobility: Individuals with AWS often experience limited range of motion in the shoulder and arm, particularly when reaching overhead or behind.
- Tightness: A sensation of tightness or pulling in the chest, armpit, and down the arm is common.
- Swelling: Some people may also experience swelling in the arm or hand due to lymphatic fluid build-up, especially if there has been lymph node removal.
These symptoms can make simple tasks, like putting on a shirt, lifting objects, or even driving, much more difficult. For many people, AWS can impact their emotional well-being as well, as chronic pain and restricted mobility can be frustrating and limiting.
How Does AWS Affect Daily Life?
The symptoms of AWS can significantly affect an individual’s daily life. Limited shoulder and arm mobility can interfere with work, hobbies, and social activities. Pain and tightness may make it hard to perform basic activities, like reaching for items on a high shelf, carrying groceries, or participating in exercise. As a result, people with AWS may become less active, which can lead to muscle weakness, poor posture, and a reduced quality of life.
Additionally, AWS can lead to long-term issues, such as decreased self-esteem and increased stress, as individuals cope with their physical limitations. It’s important for people with AWS to seek support and find ways to manage the condition so that they can maintain a high quality of life during their recovery journey.
How Physiotherapy Can Help
Physiotherapy is one of the most effective treatments for managing AWS. A physiotherapist can develop a personalized rehabilitation program to help manage pain, improve mobility, and reduce the tightness associated with the condition. Common physiotherapy treatments for AWS include:
- Manual Therapy: Techniques like massage or myofascial release can help release tension in the affected tissues, reducing pain and increasing flexibility.
- Stretching and Mobility Exercises: Physiotherapists will guide patients through stretching exercises to improve the range of motion in the shoulder and arm. This can help reduce tightness and discomfort, allowing for greater movement.
- Strengthening Exercises: Strengthening the muscles around the shoulder and upper arm is essential for improving function and reducing strain. Physiotherapists can design specific exercises to help restore muscle strength and support the joint.
- Scar Tissue Management: Physiotherapists can use specific techniques to address scar tissue buildup that can contribute to AWS, helping to soften and break down fibrous tissue, improving movement and reducing pain.
Axillary Web Syndrome is a condition that can develop after breast cancer treatments and cause pain, tightness, and limited mobility. While it can be frustrating and limiting, it’s important to know that physiotherapy can be an effective way to manage the symptoms and improve quality of life. By working with a physiotherapist, individuals with AWS can regain movement, reduce discomfort, and take steps toward better overall health and well-being. If you or someone you know is experiencing symptoms of AWS, don’t hesitate to seek help and explore the benefits of physiotherapy for relief. Our Cancer Rehab Physiotherapists at Triangle Physiotherapy have training in helping individuals who have had cancer treatments to improve their quality of life.
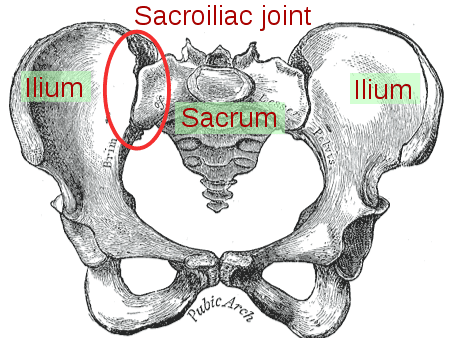
Pelvic girdle pain (PGP) is a common condition that affects the joints and ligaments in the pelvic area, often leading to discomfort in the lower back, hips, and pelvic region. It can occur during pregnancy, after childbirth, or as a result of injury or underlying musculoskeletal issues. PGP can significantly impact daily activities and overall well-being.
The pelvic health physiotherapists at Triangle Physiotherapy can help with pelvic girdle pain by doing a thorough assessment and designing a treatment plan to help with your recovery.
Symptoms of Pelvic Girdle Pain
- Pain in the lower back, hips, or pelvic area
- Discomfort that worsens with movement or weight-bearing activities
- Stiffness in the pelvis, especially after sitting or resting
- Difficulty with activities like walking, climbing stairs, or turning in bed
- Sensations of instability or “wobbliness” in the pelvic region
Treatment for Pelvic Girdle Pain at Triangle Physiotherapy Mississauga
At Triangle Physiotherapy, our experienced physiotherapists are dedicated to helping you manage pelvic girdle pain through a tailored treatment plan that may include:
Comprehensive Assessment
A detailed evaluation of your symptoms, medical history, and physical condition to create a personalized treatment approach.
Pain Management
Effective strategies for pain relief, including manual therapy, soft tissue techniques, and modalities like heat or ice therapy.
Targeted Exercises

A program of gentle exercises to strengthen the pelvic floor and core muscles, improve stability, and enhance flexibility.
Postural and Movement Education for Pelvic Girdle Pain
Guidance on proper body mechanics and techniques to reduce strain on the pelvis during daily activities.
Supportive Devices
Recommendations for supportive belts or braces to help stabilize the pelvic area and alleviate discomfort.
Lifestyle Modifications
Advice on activity adjustments and ergonomics to help manage pain and prevent flare-ups, including strategies for safe movement and positioning.
FAQs
Can pelvic girdle pain be cured?
While pelvic girdle pain may not have a definitive cure, our goal at Triangle Physiotherapy is to help you manage your symptoms effectively and improve your quality of life.
Is surgery necessary for pelvic girdle pain?
Surgery is rarely needed for PGP. Most cases can be successfully managed with non-surgical treatments and lifestyle modifications.
How can I prevent pelvic girdle pain from worsening?
Maintaining good posture, avoiding excessive strain, and practicing gentle stretching can help prevent symptoms from worsening.
If you are experiencing pelvic girdle pain, don’t hesitate to contact Triangle Physiotherapy for a consultation. Our team is committed to helping you find relief and regain your comfort in daily life.
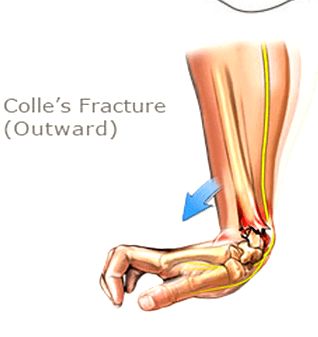
A Colles’ fracture, commonly referred to as a wrist fracture, typically occurs when a person falls onto an outstretched hand. This type of fracture primarily affects the distal radius, the bone located on the thumb side of the wrist. Colles’ fractures are prevalent among older adults, particularly those with osteoporosis, but they can occur at any age. Understanding the nature of this injury, along with effective recovery strategies and preventive measures, is crucial for regaining full functionality of the wrist and minimizing the risk of future injuries.
If you or someone you know has a Colle’s fracture, our physiotherapists at Triangle Physiotherapy can help.
Understanding Recovery
Recovery from a Colles’ fracture generally involves a combination of immobilization, rehabilitation, and lifestyle adjustments. After the fracture is diagnosed—often through X-rays—a healthcare provider may recommend a cast or splint to immobilize the wrist and allow for proper healing. The duration of immobilization can vary, typically lasting between six to eight weeks, depending on the severity of the fracture and the individual’s healing process. Once the cast is removed, the focus shifts to rehabilitation. Recovery times can vary widely, with many patients regaining full function in a few months, while others may take longer. Patience and adherence to a structured recovery plan are essential for optimal healing.
Neuromuscular Exercises post Colle’s Fracture
Neuromuscular exercises are designed to enhance the coordination and communication between the brain and muscles, which is especially important after a wrist injury. These exercises often focus on improving proprioception—the body’s ability to sense its position in space.
1. Wrist and Hand Movements: Start with simple wrist flexion and extension exercises, moving the wrist slowly through its range of motion.
2. Finger Coordination: Practice tapping each finger to the thumb, which helps improve dexterity and coordination.
Incorporating neuromuscular exercises into your recovery routine can significantly aid in regaining strength and functionality.
Mobility Incorporation post Colle’s Fracture
After the initial healing phase, it is crucial to incorporate mobility exercises to restore the full range of motion in the wrist. Gradual stretching and movement help reduce stiffness and enhance circulation.
1. Wrist Circles: Perform wrist circles in both directions to encourage mobility.
2. Tendon Gliding Exercises: These involve moving the fingers and wrist in various positions to promote flexibility and prevent stiffness.
Consistency in these mobility exercises can help ensure a smoother transition back to everyday activities.
Progressive Resistance Exercises
Once mobility is regained, progressive resistance exercises can be introduced to rebuild strength in the wrist and forearm. These exercises should start gently and gradually increase in intensity.
1. Wrist Flexion and Extension with Weights: Using light weights or resistance bands, perform controlled flexion and extension movements.
2. Grip Strengthening: Utilize grip trainers or stress balls to enhance grip strength, which is essential for overall hand function. By progressively increasing resistance, you can strengthen the wrist and surrounding muscles, reducing the likelihood of future injuries.
Prevention
Preventing future Colles’ fractures involves both lifestyle modifications and awareness. Here are some strategies to consider:
1. Fall Prevention: Improve home safety by removing tripping hazards, installing handrails, and ensuring adequate lighting.
2. Bone Health: Engage in weight-bearing exercises and maintain a diet rich in calcium and vitamin D to support bone density.
3. Regular Check-ups: Especially for older adults, regular bone density tests and discussions with healthcare providers about osteoporosis can be critical.
By focusing on prevention, you can significantly lower the risk of future wrist fractures.
FAQs
1. What are the symptoms of a Colles’ fracture?
Symptoms typically include pain and swelling in the wrist, a visible deformity (such as a “dinner fork” appearance), and difficulty moving the wrist or fingers.
2. How long does it take to recover from a Colles’ fracture?
Recovery can vary, but most people see significant improvement within 6 to 12 weeks. Full recovery may take longer, especially for older adults.
3. Can I prevent a Colles’ fracture?
Yes, by improving home safety, maintaining bone health through diet and exercise, and being mindful of your balance and stability, you can reduce your risk of a Colles’ fracture.
4. Are there any long-term effects after recovery?
Some individuals may experience stiffness, reduced range of motion, or chronic pain, particularly if the fracture was severe.
Engaging in rehabilitation exercises can help mitigate these issues. — Understanding and effectively managing a Colles’ fracture is key to ensuring a smooth recovery and maintaining wrist health. By following a comprehensive rehabilitation plan and taking preventive measures, individuals can regain their strength and enjoy a more active lifestyle.