Pregnancy is a beautiful journey, but it can come with its fair share of discomforts, one of which is pelvic pain. For many expectant mothers, pelvic pain is a common issue that can impact their daily lives. Understanding the causes and exploring effective treatments can help manage this discomfort and ensure a smoother pregnancy experience. At Triangle Physiotherapy, our trained and experienced pelvic health physiotherapists are committed to helping you with your pelvic pain so that you can get back your quality of life and do the things you love.

Here’s a detailed look at the causes of pelvic pain during pregnancy and the available treatment options.
Causes of Pelvic Pain During Pregnancy
1. Hormonal Changes
During pregnancy, the body undergoes significant hormonal changes, particularly with the increase in relaxin—a hormone that helps the pelvis become more flexible in preparation for childbirth. While this is necessary for delivery, it can also lead to joint instability and pelvic pain as the ligaments and joints become looser and less stable.
2. Growing Uterus
As the pregnancy progresses, the growing uterus exerts pressure on the pelvic region. This pressure can cause discomfort and pain, especially as the uterus expands and shifts its position. The added weight can also put strain on the pelvic joints and muscles.
3. Pelvic Girdle Pain (PGP)
Pelvic Girdle Pain, also known as Symphysis Pubis Dysfunction (SPD), is a condition where the pelvic joints become painful and unstable. This can occur when the ligaments that support the pelvic bones become too relaxed and unable to support the growing weight. PGP can cause pain in the pelvic region, hips, and lower back.
4. Round Ligament Pain
Round ligament pain is another common cause of pelvic discomfort during pregnancy. The round ligaments, which support the uterus, stretch as the uterus grows. This stretching can cause sharp or aching pain in the lower abdomen or groin area, especially with sudden movements.
5. Previous Injuries or Conditions
Women with a history of pelvic injuries or pre-existing conditions like endometriosis or fibroids may experience exacerbated pelvic pain during pregnancy. The added physical changes can aggravate these pre-existing issues.
Schedule an appointment with one of the pelvic health physiotherapists at Triangle Physiotherapy and get your recovery journey started.
Prevention
Preventing pelvic pain during pregnancy involves a combination of lifestyle adjustments and self-care practices:
- Exercise Regularly: Engage in low-impact exercises like walking, swimming, or prenatal yoga to strengthen the muscles around the pelvis and improve flexibility.
- Maintain Good Posture: Pay attention to your posture, especially when sitting or standing for extended periods. Proper posture can alleviate unnecessary strain on the pelvic region.
- Use Supportive Gear: Consider using a maternity support belt or pelvic support belt to help stabilize the pelvis and reduce pain.
- Avoid High-Risk Movements: Try to avoid activities that involve sudden movements or heavy lifting, which can exacerbate pelvic pain.
Progressive Resistance
Progressive resistance training involves gradually increasing the intensity of exercises to build strength and stability. For pregnant women experiencing pelvic pain, this approach can be adapted to:
- Strengthen Core Muscles: Exercises that target the core, such as modified planks or gentle pelvic tilts, can help support the pelvic region and reduce pain.
- Strengthen Pelvic Floor Muscles: Kegel exercises can help strengthen the pelvic floor muscles, providing better support to the pelvic organs and reducing pain.
Neuromuscular Exercises
Neuromuscular exercises focus on improving coordination and muscle control, which can be beneficial for managing pelvic pain:
- Balance Training: Exercises that enhance balance and stability, such as gentle balance exercises on a stability ball, can help reduce the risk of falls and support the pelvic region.
- Proprioceptive Exercises: Activities that improve body awareness and spatial orientation can help in managing pelvic discomfort and improving overall function.
Mobility Exercises
Mobility exercises aim to enhance the range of motion and flexibility of the pelvic joints and surrounding muscles:
- Hip Flexor Stretches: Gentle stretching of the hip flexors can help alleviate tension and discomfort in the pelvic area.
- Pelvic Rocking: Performing gentle pelvic rocking exercises can help relieve pressure on the pelvis and improve comfort.
Safety Tips
Consult a Healthcare Provider: Always consult with your healthcare provider before starting any new exercise or treatment regimen to ensure it is safe for your specific situation.
- Listen to Your Body: Pay attention to your body’s signals and avoid pushing through pain. Modify or stop activities that exacerbate discomfort.
- Seek Professional Help: If pelvic pain becomes severe or persistent, consider seeking help from a physiotherapist who specializes in prenatal care.
Pelvic pain during pregnancy can be challenging, but understanding its causes and exploring effective treatments can provide significant relief. By incorporating preventative measures, progressive resistance training, neuromuscular exercises, and mobility exercises, expectant mothers can manage pelvic pain more effectively. Always prioritize safety and consult with healthcare professionals to tailor an approach that suits your individual needs. With the right care and support, you can navigate the journey of pregnancy with greater comfort and ease.
For athletes, whether they’re professional competitors or weekend warriors, massage therapy isn’t just a luxury—it’s a crucial part of their training and recovery routine. While the soothing effects of a massage might seem like a simple indulgence, its benefits extend far beyond relaxation.

Here are five compelling reasons why athletes should incorporate massage therapy into their regimen:
1. Enhanced Recovery and Reduced Muscle Soreness
After an intense workout or a grueling competition, muscles can feel sore and fatigued. This is where massage therapy shines. By increasing blood flow and enhancing circulation, massage helps to deliver essential nutrients and oxygen to tired muscles, facilitating quicker recovery. Additionally, it helps to flush out metabolic waste products like lactic acid, which can accumulate and contribute to soreness. Regular massages can reduce muscle stiffness and speed up the recovery process, allowing athletes to get back to training faster and more efficiently.
2. Injury Prevention and Improved Flexibility
Injuries are an unfortunate part of an athlete’s life, but many can be prevented with proper care. Massage therapy plays a critical role in maintaining flexibility and preventing injuries. By working on tight or imbalanced muscles, massage helps to release tension and improve range of motion. This not only reduces the risk of strains and sprains but also helps athletes maintain proper biomechanics, which is essential for both performance and injury prevention.
3. Improved Performance and Reduced Muscle Tension
Massage therapy is not just about recovery; it also contributes to enhanced performance. By addressing muscle tension and promoting relaxation, massage can improve an athlete’s overall sense of well-being and focus. This relaxation helps in reducing the mental and physical stress that can negatively impact performance. Furthermore, a well-tuned muscle system can lead to better coordination, agility, and strength, giving athletes a competitive edge.
4. Stress Relief and Enhanced Mental Clarity
The pressures of training, competition, and performance expectations can take a toll on an athlete’s mental health. Massage therapy provides an opportunity for relaxation and stress relief. The act of being touched and the calming environment of a massage session can reduce levels of the stress hormone cortisol while boosting the release of endorphins, which are natural mood lifters. This not only helps athletes manage stress more effectively but also contributes to better mental clarity and focus, which are essential for peak performance.
5. Better Sleep Quality
Quality sleep is vital for recovery, performance, and overall health. However, athletes often struggle with sleep issues due to the physical demands of their training and competitions. Massage therapy can improve sleep quality by promoting relaxation and reducing physical discomfort that might interfere with rest. Enhanced relaxation and reduced muscle tension can lead to deeper, more restorative sleep, which is crucial for muscle repair, cognitive function, and overall well-being.
Incorporating Massage Therapy into Your Routine
To reap the maximum benefits of massage therapy, it’s important for athletes to incorporate it into their regular training regimen. Working with a skilled therapist who understands the specific needs of athletes can make a significant difference. Whether it’s a post-workout recovery session, a pre-competition tune-up, or a routine maintenance massage, finding the right type of massage and frequency that works best for your body can help you achieve optimal performance and maintain overall health.
In conclusion, massage therapy offers a wealth of benefits for athletes, from speeding up recovery and preventing injuries to enhancing performance and improving mental clarity. By integrating massage into their training and recovery routines, athletes can better support their physical and mental well-being, paving the way for sustained success and peak performance.
Massage Therapy Mississauga
We have 2 locations with massage therapists in Mississauga to help you.
Sprains vs. strains? Understanding the difference between sprains and strains is crucial for anyone engaged in physical activities or sports. Both are common injuries, but they affect different parts of the body and require distinct approaches for treatment and prevention. Here’s a comprehensive look at sprains and strains, including their causes, prevention strategies, and more.
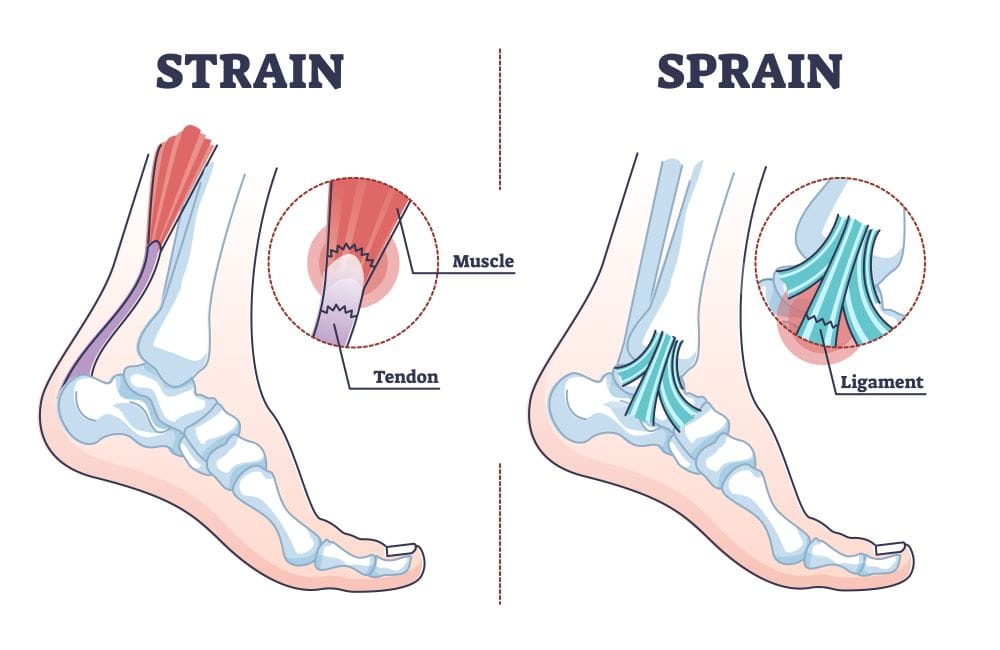
Picture Credit: Louisville Bones
Causes
Sprains occur when the ligaments, which are the tough bands of connective tissue that connect bones to each other, are stretched or torn. This usually happens due to a sudden twist or impact that forces a joint out of its normal range of motion. Common examples include rolling an ankle during a fall or twisting a knee while playing sports.
Strains, on the other hand, involve injuries to muscles or tendons, which connect muscles to bones. They are typically caused by overstretching or overusing a muscle, often due to sudden movements or lifting heavy objects improperly. Strains can happen during activities that require a lot of physical effort, such as running, lifting weights, or engaging in sports.
Prevention
Preventing sprains and strains starts with proper preparation and conditioning.
- For Sprains: Wearing appropriate footwear and using supportive gear during activities can help reduce the risk. Strengthening the muscles around the joints and improving balance through exercises can also be beneficial. Additionally, warming up properly before engaging in physical activities is crucial to prepare the ligaments for stress.
- For Strains: To prevent strains, it’s important to use proper techniques when lifting or performing strenuous activities. Regular strength training and flexibility exercises can help maintain muscle balance and reduce the risk of overstretching. Ensuring you are adequately warmed up before exercising can also protect against strains.
Progressive Resistance
Progressive resistance training involves gradually increasing the weight or resistance in exercises to build strength and endurance over time. This method is effective in preventing both sprains and strains by:
- For Sprains: Strengthening the muscles around the joints can provide better support and stability, reducing the likelihood of ligaments being stretched or torn.Practice ankle exercises using resistance bands
For Strains: Progressive resistance training helps in building muscle strength and resilience, which can prevent overstretching and muscle fatigue.Peform isolated movements that help with day to day resilience.
Neuromuscular Exercises
Neuromuscular exercises focus on improving the communication between the brain and muscles, enhancing coordination and stability. These exercises are particularly effective for:
- For Sprains: They help improve joint stability and balance, reducing the risk of accidents that might lead to sprains. Exercises such as balance training and proprioceptive drills can be beneficial. Use BOSU ball
- For Strains: Neuromuscular exercises enhance the control and responsiveness of muscles, reducing the chances of strains by improving movement patterns and muscle coordination. Allow it to rest, knowing when to rest is equally important.Drink plenty of water, and practice unilateral movements.Stretch the lower limbs.
Mobility Exercises
Mobility exercises aim to improve the range of motion and flexibility of joints and muscles. They are crucial for:
- For Sprains: Increasing joint mobility can help maintain a healthy range of motion, which can reduce the risk of injuries. Regular stretching and joint mobility exercises can keep ligaments and surrounding tissues flexible.
- For Strains: Enhancing muscle flexibility through mobility exercises can help prevent strains by allowing muscles to stretch properly without being overstretched. Incorporating dynamic stretches and functional movements can be beneficial. Go into deeper joint ROM.
Safety Tips
- Warm Up: Always start with a proper warm-up to prepare your muscles and ligaments for activity.
- Use Proper Techniques: Whether lifting weights or engaging in sports, ensure you use the correct techniques to avoid unnecessary strain.
- Listen to Your Body: Pay attention to any signs of discomfort or pain, and avoid pushing through it.
- Rest and Recover: Allow adequate time for rest and recovery to prevent overuse injuries.
If you suspect you have a sprain or a strain, give us a call or book an appointment to see one of our physiotherapists to get an assessment and treatment plan.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Menopause brings about numerous changes in a woman’s body, and one of the more common, yet rarely discussed, issues is painful sex. This discomfort can be distressing and have a significant impact on your intimate relationships and quality of life. However, many don’t realize that a key factor in this pain could be pelvic floor health.
In this post, we’ll explore how menopause affects your pelvic floor, why it can lead to painful sex, and what can be done to manage and alleviate this condition. Let’s break it down.
1. Understanding Menopause and Vaginal Changes
Menopause, typically occurring between ages 45 and 55, is marked by the natural decline in estrogen levels. This hormone is essential for maintaining the health and elasticity of your vaginal tissue. When estrogen production decreases, the vagina can become:
- Drier (vaginal atrophy or dryness)
- Thinner and more fragile
- Less elastic
These changes contribute to vaginal discomfort, especially during intercourse, and are a common cause of pain during sex for women in menopause.
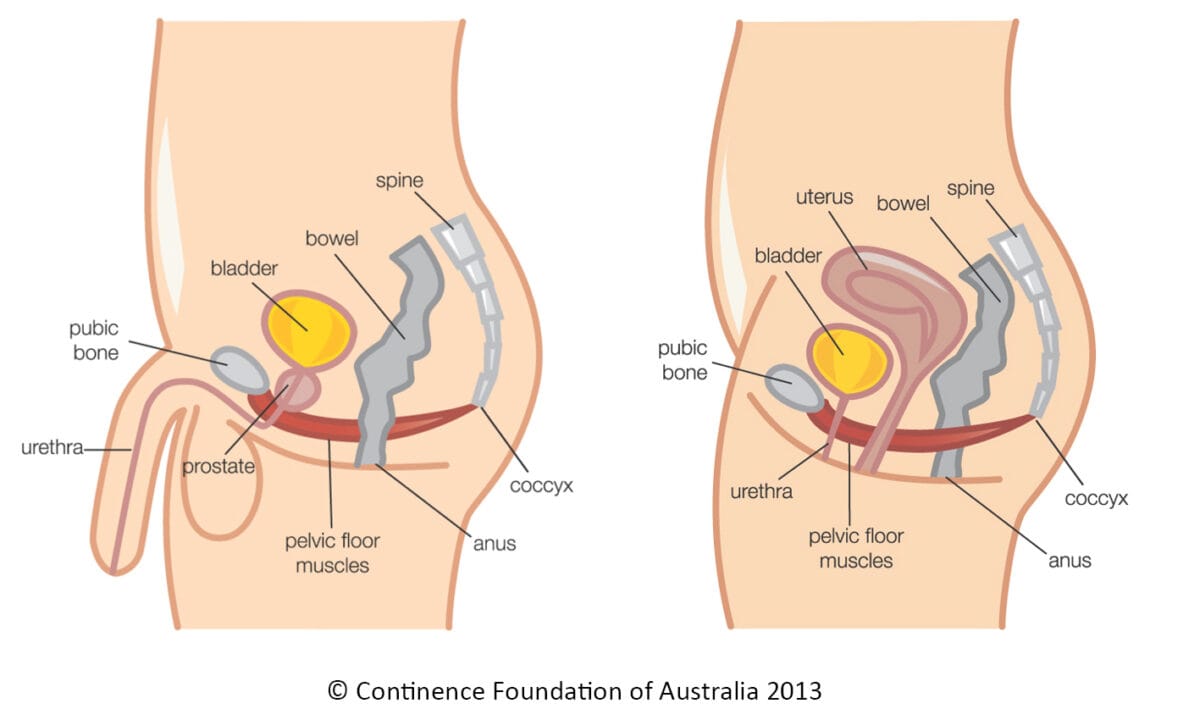
2. The Role of the Pelvic Floor in Sexual Health
Your pelvic floor muscles play a crucial role in sexual function. These muscles support the pelvic organs, including the bladder, uterus, and rectum, and also control vaginal tightness and relaxation during sex.
When pelvic floor muscles are functioning properly, they:
- Help maintain vaginal tone
- Support lubrication and arousal
- Allow comfortable contraction and relaxation during intercourse
However, during menopause, the pelvic floor muscles may weaken or become overly tight (hypertonic), both of which can contribute to pain during sex. In fact, pelvic floor dysfunction is one of the leading causes of dyspareunia (painful sex) in menopausal women.
3. How Menopause Affects the Pelvic Floor
As estrogen levels drop, not only does vaginal tissue change, but the pelvic floor muscles also lose elasticity and strength. There are two main types of pelvic floor dysfunction that can result from menopause:
- Weak Pelvic Floor: Weakened muscles can result in less support for the pelvic organs, which may contribute to conditions like pelvic organ prolapse. This can lead to discomfort during sex.
- Tight Pelvic Floor: Some women develop tight or overactive pelvic floor muscles (hypertonicity), which can create tension and pain during penetration.
These issues, combined with vaginal dryness, can make intercourse uncomfortable or even painful.
4. Managing Painful Sex: The Role of Pelvic Floor Physiotherapy
The good news is that pelvic floor physiotherapy can play a significant role in managing and reducing pain during sex, particularly for women going through menopause.

Here’s how it works:
Pelvic Floor Muscle Training
For women with weakened pelvic floor muscles, physiotherapists may recommend exercises such as Kegels to strengthen the muscles. Strengthening exercises can improve vaginal tone, enhance sexual function, and reduce discomfort during intercourse.
Relaxation Techniques and Biofeedback
For those experiencing tight or overactive pelvic floor muscles, relaxation techniques are key. Physiotherapists can guide you through:
- Stretching exercises to release tension in the pelvic floor
- Breathing exercises to promote muscle relaxation
- Biofeedback to help you learn how to consciously relax your pelvic floor during sex
Vaginal Dilators

In some cases, physiotherapists may recommend vaginal dilators to help gently stretch and relax the vaginal muscles. This can be particularly helpful for women experiencing severe pain with penetration.
5. Additional Tips to Alleviate Painful Sex
In addition to physiotherapy, there are a few lifestyle adjustments and treatments that can help alleviate painful sex during menopause:
- Lubricants: Using a water-based lubricant can ease vaginal dryness and reduce friction during intercourse.
- Moisturizers: Regular use of vaginal moisturizers can help maintain hydration and prevent tissue dryness.
- Hormone Therapy: Consult with your doctor about localized estrogen treatments, such as creams, to restore vaginal tissue health.
- Open Communication: Talk to your partner about your pain and work together to find positions and techniques that minimize discomfort.
6. When to Seek Help
It’s important to remember that painful sex during menopause is not something you have to live with. If sex becomes uncomfortable or painful, seeking the help of a pelvic health physiotherapist can make a big difference. They will conduct a thorough assessment, address the underlying pelvic floor issues, and create a personalized treatment plan to restore your comfort and confidence in intimacy.
Painful sex during menopause is a common yet manageable issue. The changes in hormone levels can affect your vaginal health and pelvic floor, leading to discomfort during intercourse. However, pelvic floor physiotherapy can offer effective solutions, whether through strengthening, relaxation techniques, or other therapeutic methods.
By addressing these changes head-on and seeking appropriate treatment, you can enjoy pain-free and fulfilling intimacy throughout your menopausal years.
Do you have questions about how your pelvic floor may be contributing to painful sex? Contact us today to learn more about how pelvic health physiotherapy can help you regain comfort and confidence in your body.
Our pelvic health physiotherapists in Mississauga can help you regain your quality of life, menopause or not!
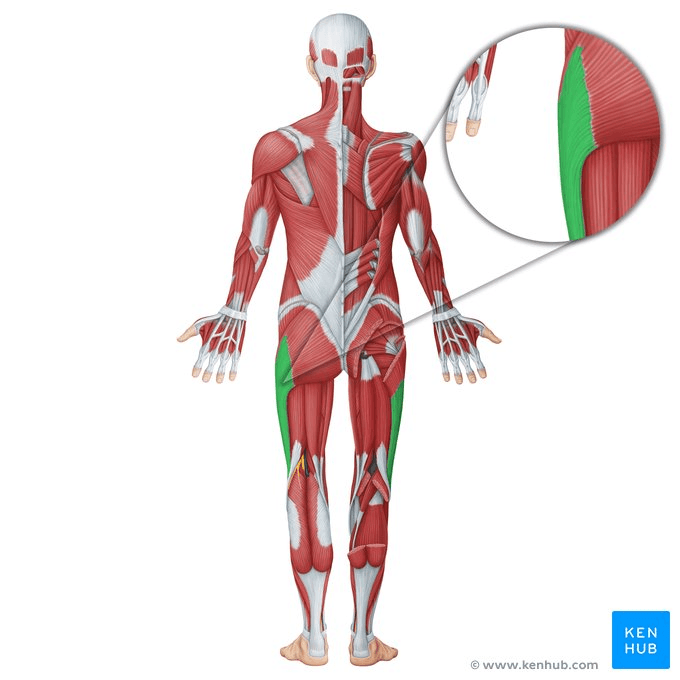
IT Band Syndrome (Iliotibial Band Syndrome) is a common condition among athletes and active individuals, characterized by pain on the outside of the knee. This pain is typically caused by inflammation of the IT band, a thick band of connective tissue running along the outer thigh from the hip to the shin.
Understanding the causes, effective treatment strategies, and prevention methods can help you manage and avoid this frustrating condition. Let’s delve into what IT Band Syndrome is, how to treat it, and strategies to prevent it from recurring.
Causes of IT Band Syndrome
IT Band Syndrome often develops due to repetitive stress and overuse of the knee joint. Several factors can contribute to this condition:
- Overuse: Repeatedly performing activities that involve knee flexion and extension, such as running or cycling, can lead to IT band irritation.
- Biomechanical Issues: Abnormalities in your gait or foot mechanics, like overpronation or leg length discrepancies, can increase stress on the IT band.
- Muscle Imbalances: Weakness or tightness in the muscles of the hip, thigh, or calf can affect the alignment and function of the IT band.
- Improper Footwear: Wearing shoes that do not provide adequate support or cushioning can contribute to the development of IT Band Syndrome.
- Sudden Increase in Activity: Rapidly increasing the intensity or duration of physical activity without proper conditioning can strain the IT band.
Importance of Physiotherapy
Physiotherapy is a crucial component in both the treatment and prevention of IT Band Syndrome. A physiotherapist can help by:
- Assessing and Diagnosing: They will evaluate your movement patterns, muscle strength, and flexibility to pinpoint the underlying issues contributing to your symptoms.
- Developing a Treatment Plan: A tailored treatment plan may include exercises, manual therapy, and advice on activity modifications to alleviate pain and prevent recurrence.
- Education and Guidance: Physiotherapists provide valuable education on injury prevention, proper technique, and ways to incorporate exercises into your routine.
Key Principles of Physiotherapy
- Pain Relief: The initial focus is on managing pain and inflammation. This might involve rest, ice application, and anti-inflammatory medications.
- Gradual Loading: Gradually reintroducing activity is important to avoid further strain. This includes slowly increasing exercise intensity and duration.
- Muscle Balance and Alignment: Addressing any muscle imbalances and ensuring proper alignment can help reduce the stress on the IT band.
Strengthening Exercises
Strengthening the muscles around the hip and knee can help support the IT band and reduce the risk of future injuries. Effective exercises include:
- Clamshells: Lie on your side with knees bent and feet together. Lift the top knee while keeping your feet touching. This strengthens the hip abductors.
- Bridges: Lie on your back with knees bent and feet flat on the floor. Lift your hips towards the ceiling, then lower them back down. This exercise targets the glutes and hamstrings.

Neuromuscular Exercises
Neuromuscular exercises improve coordination and muscle function, which can aid in injury prevention and recovery:
- Single-Leg Squats: Perform squats on one leg to enhance balance and strength. Start with a small range of motion and gradually increase as strength improves.
- Step-Ups: Step onto a platform with one foot and then back down. This exercise helps improve the strength and control of the hip and knee.
Proprioceptive Exercises
Proprioceptive exercises help improve your body’s awareness of its position, which is vital for maintaining proper movement mechanics:
- Balance Board Exercises: Stand on a balance board and try to maintain stability. This enhances proprioception and ankle stability.
- Bosu Ball Work: Perform exercises such as squats or lunges on a Bosu ball to challenge your balance and coordination.
Incorporating Mobility
Maintaining and improving joint mobility is essential for overall function and injury prevention:
- Foam Rolling: Use a foam roller to massage and release tightness in the IT band and surrounding muscles.
- Dynamic Stretching: Incorporate dynamic stretches such as leg swings and hip circles into your warm-up routine to improve flexibility and range of motion. Try performing the static stretch for ITB in standing as well. Ensure to work on glute medius and hip flexors along with ITB. Learn to brace the core well. Avoid full/deep ROM exercises till you feel better. Using a half foam roller to squat down is better than squatting through pain.
Understanding IT Band Syndrome and implementing effective treatment and prevention strategies can help you manage this condition and maintain an active lifestyle. Physiotherapy plays a vital role in addressing pain, improving function, and preventing future issues. By focusing on strengthening, neuromuscular, proprioceptive exercises, and incorporating mobility work, you can support your recovery and reduce the likelihood of recurrence. Remember to follow safety tips and consult with healthcare professionals to tailor a plan that best suits your needs. With the right approach, you can overcome IT Band Syndrome and get back to enjoying your favorite exercises.
Are you ready to get that IT Band Injury resolved? Contact Triangle Physiotherapy to schedule an Initial Assessment and get on the road to recovery!
Our Toronto locations are conveniently located with easy transit access:
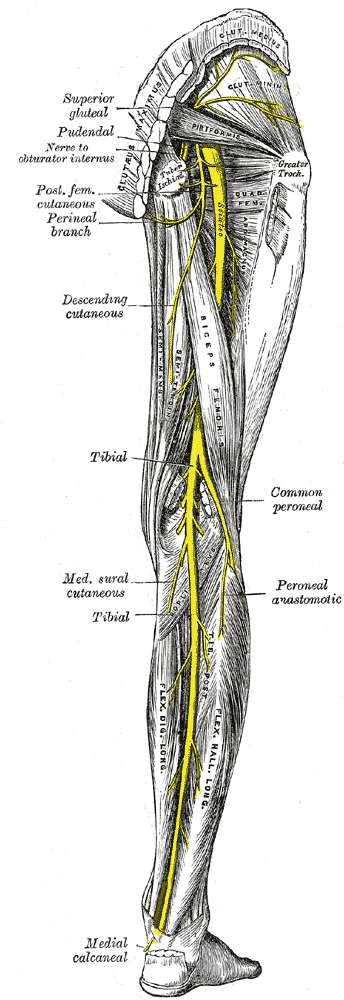
Sciatica is a term that’s often thrown around, but it’s not a condition itself; it’s a symptom of something else. When people talk about sciatica, they’re referring to pain that radiates along the path of the sciatic nerve, which runs from the lower back through the hips and buttocks and down each leg. This pain can vary from a mild ache to a sharp, burning sensation. It can be debilitating, affecting your daily life and limiting your mobility. With so many treatment options available, one common question is whether chiropractic care can effectively help with sciatica. Let’s dive into this topic and see what the evidence and experience suggest.
Understanding Sciatica
Sciatica typically arises from an issue in the lower back, such as a herniated disc, spinal stenosis, or a misalignment of the vertebrae. These conditions can put pressure on the sciatic nerve, leading to pain, numbness, or tingling sensations that radiate down the leg. The discomfort often worsens with prolonged sitting, standing, or sudden movements, and can be accompanied by muscle weakness or difficulty moving the leg.
The Role of Chiropractic Care
Chiropractic care focuses on diagnosing and treating musculoskeletal disorders, with an emphasis on spinal health. Chiropractors use manual adjustments and other techniques to correct misalignment in the spine and improve overall function. But can these methods help with sciatica?
1. Spinal Adjustments
One of the primary treatments a chiropractor might offer is spinal adjustments. The goal here is to realign the vertebrae in the spine to reduce pressure on the sciatic nerve. Misalignment or subluxation in the spine can sometimes contribute to sciatica by irritating or compressing the nerve. By performing adjustments, chiropractors aim to restore proper alignment, alleviate nerve pressure, and reduce inflammation, which can, in turn, decrease sciatica symptoms.
2. Flexion-Distraction Therapy
Another technique used by chiropractors is flexion-distraction therapy. This method involves a specialized table that gently stretches and flexes the spine, aiming to relieve pressure on the discs and nerves. It’s often used for conditions like herniated discs, which are a common cause of sciatica. This therapy can help in reducing pain and improving mobility by creating more space within the spinal column and reducing nerve compression.
PS : Our FCAMPT certified physiotherapists (Ashish, Jigisha and Ankit) also practice this technique!
3. Physical Therapy and Exercises
Chiropractors often incorporate physical therapy and specific exercises into their treatment plans for sciatica. These exercises can help strengthen the muscles around the spine, improve flexibility, and promote better posture. For sciatica sufferers, strengthening the core and lower back muscles can provide better support for the spine and reduce the likelihood of future episodes.
4. Lifestyle and Ergonomics Advice
In addition to hands-on treatments, chiropractors also provide guidance on lifestyle changes and ergonomics. They may offer advice on how to sit properly, how to lift objects correctly, and how to maintain good posture throughout the day. These adjustments can help prevent the recurrence of sciatica by addressing the factors that may contribute to the condition.
What the Research Says
Scientific studies on chiropractic care for sciatica have shown promising results. Research indicates that spinal manipulation can be effective in reducing pain and improving function in patients with sciatica. For instance, a study published in The Journal of the American Board of Family Medicine found that chiropractic care, combined with standard medical treatments, provided significant relief for sciatica patients.
However, it’s essential to approach chiropractic care with realistic expectations. While many people find relief from chiropractic adjustments, it may not be a cure-all. The effectiveness of chiropractic treatment can vary based on the underlying cause of sciatica, the severity of the symptoms, and individual patient factors.
Consultation and Care
If you’re considering chiropractic care for sciatica, it’s crucial to consult with a healthcare provider first to determine the underlying cause of your symptoms. A comprehensive evaluation can help in designing a treatment plan tailored to your needs. Chiropractors often work in conjunction with other healthcare professionals to provide a holistic approach to managing sciatica.
In summary, chiropractic care can be a beneficial component in managing sciatica, particularly when it comes to spinal adjustments, flexion-distraction therapy, and strengthening exercises. While not a guaranteed solution for everyone, many people find that chiropractic treatments help reduce pain and improve their quality of life. As with any medical treatment, it’s important to approach chiropractic care with informed expectations and in collaboration with your overall healthcare team. If you’re struggling with sciatica, a consultation with a chiropractor might be a worthwhile step in your journey toward relief and recovery.
Is there a Chiropractor in Oakville that can help with Sciatica?
The Chiropractors at Triangle Physiotherapy in Oakville are qualified and experienced professionals that can help you with your Sciatica.
As we age, maintaining mobility and independence becomes increasingly important for overall quality of life. For many elderly individuals, staying active and independent can be challenging due to various age-related factors. Physiotherapy emerges as a crucial tool in addressing these challenges, helping seniors preserve their physical function and improve their daily living. This blog explores the importance of physiotherapy for the elderly, highlighting causes of mobility issues, preventive measures, and effective exercises to support strength and mobility.
Our experienced practitioners at Triangle Physiotherapy can help you to stay active and prevent any mobility issues that may arise with age.
Call us today to learn more about how we can help you start moving better.
Causes
Several factors contribute to decreased mobility in elderly individuals. Common causes include:
- Muscle Weakness: Aging often leads to muscle loss, making it harder to perform everyday activities.
- Joint Stiffness: Reduced flexibility and joint pain can limit movement.
- Balance Problems: Deteriorating balance increases the risk of falls, which can lead to serious injuries.
- Chronic Conditions: Diseases such as arthritis, osteoporosis, and cardiovascular issues can impact physical ability.
Understanding these causes helps in designing targeted physiotherapy interventions to address specific challenges and improve overall function.
Prevention

Preventive measures play a vital role in maintaining mobility and independence as we age. Regular physical activity, a balanced diet, and routine medical check-ups can help mitigate some of the issues that arise with aging. Your Physiotherapist will help you incorporate the following into daily routines can be beneficial:
- Regular Exercise: Engaging in physical activities such as walking, swimming, or biking helps maintain muscle strength and joint flexibility.
- Healthy Diet: A diet rich in calcium and vitamin D supports bone health, while protein helps in muscle maintenance.
- Routine Check-ups: Regular visits to healthcare professionals can help manage chronic conditions and prevent complications.
Importance of Physiotherapy
Physiotherapy is essential for elderly individuals to address and manage mobility issues. It offers several benefits:
- Personalized Care: Physiotherapists design customized exercise programs based on individual needs and limitations.
- Pain Management: Through techniques like manual therapy and modalities such as heat or cold therapy, physiotherapy can help alleviate pain.
- Fall Prevention: Physiotherapy can enhance balance and coordination, reducing the risk of falls and related injuries.
- Enhanced Quality of Life: Improved mobility and independence contribute to a better overall quality of life and increased participation in social activities.
Strengthening and Mobility Exercises
Strengthening and mobility exercises are fundamental components of physiotherapy for seniors. These exercises help maintain and improve physical function:
- Strengthening Exercises: Focus on major muscle groups to enhance overall strength. Examples include seated leg lifts, wall push-ups, and resistance band exercises.
- Mobility Exercises: Improve joint flexibility and range of motion. Simple activities such as ankle circles, shoulder rolls, and gentle stretching can be beneficial.
- Additionally, the GLA:D Program for Knee and Hip Arthritis can be very beneficial because it provides education and targeted exercise that can be applied to movement in everyday activities.
Regular practice of these exercises helps prevent muscle atrophy and joint stiffness, promoting better movement and function.
Neuromuscular Exercises
Neuromuscular exercises target coordination, balance, and proprioception (the sense of body position). These exercises are crucial for fall prevention and overall stability:
- Balance Training: Activities such as standing on one leg, heel-to-toe walking, and balance board exercises enhance stability.
- Coordination Drills: Exercises like toe taps, marching in place, and dynamic movements help improve coordination and reaction times.
- Proprioceptive Exercises: Incorporate activities that challenge the senses and improve body awareness, such as using a wobble cushion or performing slow, controlled movements.
Safety Tips
Safety is paramount when performing exercises, especially for seniors. Consider these tips to ensure a safe and effective physiotherapy routine:
- Consult a Professional: Always seek guidance from a qualified physiotherapist before starting any new exercise program.
- Start Slowly: Begin with low-intensity exercises and gradually increase intensity to avoid overexertion.
- Use Proper Equipment: Ensure that any exercise equipment is appropriate and in good condition to prevent accidents.
- Listen to Your Body: Pay attention to any discomfort or pain and stop the activity if necessary.
Call us today to learn more and get started!
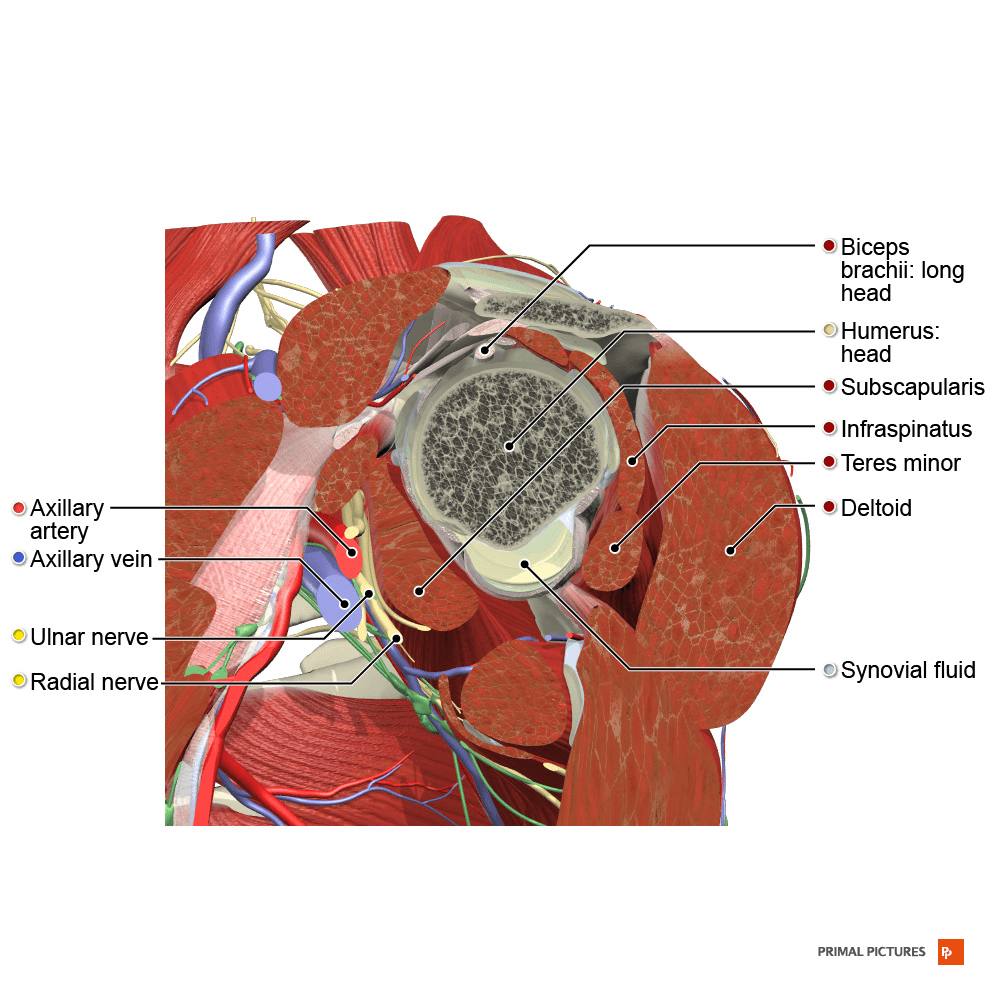
Rotator cuff tears can be a challenging injuries, impacting your ability to perform everyday tasks and participate in activities you enjoy. The rotator cuff, a group of four muscles and their tendons located in the shoulder, is crucial for shoulder stability and movement. Physiotherapy plays a vital role in the recovery process, helping to alleviate pain, restore function, and prevent future injuries. In this guide, we’ll explore how physiotherapists can assist with a rotator cuff tear, including causes, prevention strategies, and various physiotherapy techniques.
Our physiotherapists in Toronto can help you with rotator cuff injuries and rehabilitation.
Causes of Rotator Cuff Tears
What It Is: The rotator cuff consists of four muscles—supraspinatus, infraspinatus, teres minor, and subscapularis (SITS) —that stabilize and move the shoulder joint. A tear in one or more of these tendons can disrupt shoulder function.
Common Causes:
- Overuse: Repetitive overhead motions, such as those performed in sports like baseball or tennis, can lead to gradual wear and tear.
- Acute Injury: A sudden fall or lifting a heavy object can cause an acute rotator cuff tear.
- Aging: As we age, the tendons can weaken and become more prone to tears due to decreased blood supply and collagen degeneration.
Prevention Strategies
How to Reduce Risk: Although some rotator cuff tears are unavoidable, implementing preventive measures can help minimize the risk.
- Strength Training: Strengthen the muscles around the shoulder, including the rotator cuff muscles, to support the joint and prevent strain.
- Proper Technique: Use correct form when performing overhead activities or lifting weights to reduce undue stress on the shoulder.
- Regular Stretching: Maintain flexibility in the shoulder and adjacent joints to prevent stiffness and improve the range of motion. For example, one tends to have tight chest muscles and weak back muscles, hence the shoulder overcompensates.
Resistance Exercises
Purpose: Resistance exercises help build strength in the rotator cuff and surrounding muscles, which is crucial for stabilizing the shoulder joint and aiding recovery.
Examples:
- External Rotations: Use a resistance band or light dumbbell to perform external rotation exercises, targeting the infraspinatus and teres minor.
- Internal Rotations: Perform internal rotation exercises with a band or dumbbell to strengthen the subscapularis muscle.
- Scapular Retractions: Strengthen the muscles between the shoulder blades to support overall shoulder function.
How to Do Them Safely: Start with low resistance and increase gradually as your strength improves. Focus on controlled movements to avoid further strain on the shoulder.
Neuromuscular Exercises
Purpose: Neuromuscular exercises enhance coordination and the communication between your brain and muscles, improving shoulder stability and function.
Examples:
- Shoulder Blade Squeezes: Squeeze your shoulder blades together to activate the muscles that stabilize the shoulder.
- Proprioceptive Training: Use a stability ball or balance board to improve proprioception and shoulder stability.
- Dynamic Movements: Incorporate exercises that involve dynamic shoulder movements to enhance neuromuscular control.
How to Do Them Safely: Start with basic exercises and progress to more challenging ones as your coordination and stability improve.
Progressive Exercises
Purpose: Progressive exercises are designed to gradually increase in difficulty, helping to build strength and endurance while avoiding overexertion.
Examples:
- Shoulder Press: Begin with light weights and gradually increase the load as your shoulder strength improves.
- Front Raises: Use light dumbbells to perform front raises, increasing the weight progressively.
- Side-Lying Abduction: Lift your arm while lying on your side to strengthen the shoulder muscles, starting with lighter resistance and increasing as tolerated.
How to Do Them Safely: Follow a structured program that gradually increases the intensity and complexity of exercises to prevent overuse injuries.
Stretching and Strengthening
Purpose: Stretching maintains flexibility and reduces stiffness, while strengthening exercises build muscle support necessary for shoulder stability.
Examples:
- Pendulum Exercises: Allow your arm to swing gently in circles to improve flexibility and reduce stiffness.
- Cross-Body Stretch: Stretch the shoulder by bringing one arm across your body and holding it with the opposite arm.
- Strengthening Exercises: Perform exercises like resisted shoulder external and internal rotations to build rotator cuff strength.
How to Do Them Safely: Stretch slowly and hold each stretch for 15-30 seconds. Ensure strengthening exercises are done with proper form and controlled movements.
Mobility Routine
Purpose: A mobility routine focuses on improving the range of motion and overall function of the shoulder joint.
Examples:
- Shoulder Circles: Perform gentle shoulder circles to increase flexibility and mobility.
- Wall Angels: Stand with your back against a wall and slowly move your arms up and down to improve shoulder movement.
- Towel Stretch: Hold a towel behind your back with both hands and gently pull to stretch the shoulder.
How to Do Them Safely: Perform exercises within a comfortable range of motion and avoid pushing through pain.
Tips for Safely Performing Activities
How to Stay Safe: As you recover and resume activities, following these tips can help prevent re-injury and ensure a safe return to your routine.
- Listen to Your Body: Pay attention to any pain or discomfort and modify your activities as needed.
- Gradual Return: Ease back into your regular activities and sports gradually to allow your shoulder to adjust.
- Use Proper Technique: Ensure you use correct techniques for overhead movements and lifting to prevent undue stress on your shoulder.
Seek Professional Guidance: Work with a physiotherapist to develop a personalized rehabilitation program and get advice on technique and progression.
Recovering from a rotator cuff tear involves a comprehensive approach that includes strength building, flexibility exercises, and proper mobility routines. By incorporating resistance and neuromuscular exercises, following a progressive exercise routine, and paying attention to your body’s signals, you can enhance your recovery and reduce the risk of future injuries. Remember, patience and consistency are key in your rehabilitation journey. With the right physiotherapy and preventive measures, you’ll be back to your favorite activities stronger and more resilient.Don’t let these physical conditions ever ride on you.
Click here to book an appointment with a physiotherapist in Toronto.
An ACL tear can be a significant setback, especially for athletes and active individuals. The ACL (anterior cruciate ligament), located in the knee, plays a crucial role in stabilizing and allowing movement. When it’s torn, physiotherapy becomes essential for a successful recovery. In this guide, we’ll explore the causes of ACL tears, prevention strategies, and the various physiotherapy techniques that can aid in recovery.
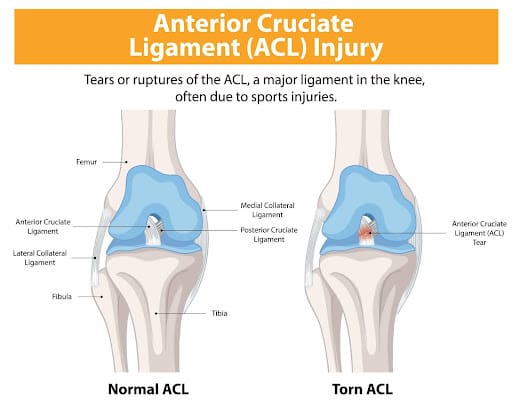
Causes of ACL Tears
What It Is: The ACL is a ligament in the knee that helps stabilize the joint and control movement. An ACL tear is a common knee injury, particularly in sports.
Common Causes:
- Sudden Stops and Starts: Rapid changes in direction or sudden stops can put excessive stress on the ACL.
- Direct Impact: A blow to the knee or a collision, common in contact sports like football or basketball, can cause the ACL to tear.
- Improper Landing: Landing awkwardly from a jump or fall can also strain the ACL.
Prevention Strategies
How to Reduce Risk: While not all ACL tears can be prevented, taking certain measures can significantly lower your risk.
- Strength Training: Strengthen the muscles around your knee, including the quadriceps, hamstrings, and calf muscles, to provide better support and stability.
- Proper Technique: Learn and practice proper techniques for jumping, landing, and pivoting to reduce stress on your knee.
- Warm-Up: Always warm up before engaging in sports or strenuous activities to prepare your muscles and joints for the demands ahead.
Resistance Exercises
Purpose: Resistance exercises help build strength in the muscles surrounding the knee, which is crucial for stabilizing the joint and aiding recovery. The ones mentioned below are to be performed in the latter stages of rehab, with professional help.
Examples:
- Squats: Perform squats with proper form to strengthen the quadriceps, hamstrings, and glutes.
- Leg Press: Use a leg press machine to work on lower body strength while controlling the range of motion.
- Lunges: Lunges help in building strength and balance in the legs, targeting various muscle groups around the knee.
How to Do Them Safely: Start with light weights or bodyweight, gradually increasing the resistance as your strength improves. Focus on maintaining proper form to avoid additional strain.

Neuromuscular Exercises
Purpose: Neuromuscular exercises enhance the communication between your brain and muscles, improving coordination and balance.
Examples:
- Balance Boards: Standing on a balance board helps improve stability and proprioception (awareness of your body’s position in space).
- Single-Leg Stands: Practice standing on one leg to strengthen stabilizing muscles and improve balance.
- Agility Drills: Incorporate ladder drills or cone drills to enhance agility and neuromuscular control.
How to Do Them Safely: Start with easier exercises and gradually progress to more challenging ones as your balance and coordination improve.

Progressive Exercises
Purpose: Progressive exercises are designed to gradually increase in difficulty, helping to build strength and endurance while avoiding overexertion.
Examples:
- Step-Ups: Begin with low steps and gradually increase the height as your strength and stability improve.
- Resistance Bands: Use resistance bands to add progressive resistance to leg exercises, adjusting the band’s tension as needed.
- Cycling: Start with short, low-resistance cycles and progressively increase duration and resistance.
How to Do Them Safely: Follow a structured program that gradually increases the intensity and complexity of exercises to prevent overuse injuries.
Stretching and Strengthening
Purpose: Stretching maintains flexibility and prevents stiffness, while strengthening exercises build the muscle support necessary for knee stability.
Examples:
- Hamstring Stretch: Gentle stretching of the hamstrings can help maintain flexibility and reduce tension in the knee.
- Quadriceps Stretch: Stretch the quadriceps to keep the front of the thigh flexible and balanced.
- Strengthening Exercises: Incorporate exercises like leg lifts and bridges to build muscle strength around the knee.
How to Do Them Safely: Perform stretching exercises slowly and hold each stretch for 20-30 seconds. Strengthening exercises should be done with controlled movements and proper form.
Mobility Routine
Purpose: A mobility routine focuses on improving the range of motion and function of the knee joint.
Examples:
- Knee Circles: Perform gentle knee circles to increase flexibility and mobility.
- Heel Slides: Lie on your back and slide your heel towards your buttocks to improve knee flexion.
- Straight Leg Raises: Lift your leg while keeping it straight to maintain and improve knee range of motion.
How to Do Them Safely: Ensure you’re performing exercises within a comfortable range of motion and avoid pushing through pain.
Tips for Safely Performing Activities
How to Stay Safe: As you recover and resume activities, following these tips can help prevent re-injury and ensure a safe return to your routine.
- Listen to Your Body: Pay attention to any pain or discomfort and modify your activities as needed.
- Gradual Return: Ease back into your regular activities and sports gradually to allow your knee to adjust.
- Use Supportive Gear: Consider using a knee brace or support during high-impact activities for added stability.
- Seek Professional Guidance: Work with a physiotherapist to develop a personalized rehabilitation program and get advice on technique and progression.
Physiotherapy Treatment of an ACL Sprain
A physiotherapist will examine both knees, comparing the injured knee to the uninjured one. During this exam, the physiotherapist will check your injured knee for signs of swelling, deformity, tenderness, fluid inside the knee joint, and discoloration. If the patient does not have too much pain and swelling, a physiotherapist will then evaluate the knee’s range of motion and will pull against the ligaments to check their strength. During the exam, the patient will have to bend their knee and the physiotherapist will gently pull forward or push backward on their lower leg where it meets the knee.
Based on the results of the patient’s exam, diagnostic tests may need to be performed to further evaluate the condition of the patient’s knee. These tests may include standard X-rays to check for ligament separation from bone or fracture. Tests may also include an MRI scan or a camera–guided knee surgery (arthroscopy). The expected duration of recovery depends on the severity of the patient’s knee sprain, their rehabilitation program, and what type of sports the patients play. In general, milder sprains heal within 2-4 weeks, whereas other types may take 4-12 months.
Looking to have an ACL Injury treated? Schedule an appointment today!
Contact our clinic to book an appointment with one of our physiotherapists to help you recover from your ACL injury!
Our Mississauga Physiotherapy Clinics are located at:
Pelvic pain can be a challenging and often misunderstood condition. It can significantly impact your quality of life, making it essential to understand your treatment options and management strategies. In this Q&A guide, we’ll explore the common questions surrounding pelvic pain and provide insights into how pelvic health physiotherapy can help.
What is pelvic pain, and what are its common causes?
Pelvic pain refers to discomfort or pain experienced in the lower abdomen, pelvis, or perineum. It can be acute (short-term) or chronic (lasting six months or more). The causes of pelvic pain are diverse and can include:
- Muscle dysfunction: Tight or weak pelvic floor muscles can lead to pain.
- Nerve conditions: Issues like pudendal neuralgia can cause significant discomfort.
- Gynecological conditions: Endometriosis, ovarian cysts, and uterine fibroids are common culprits.
- Urological issues: Interstitial cystitis or urinary tract infections (UTIs) can cause pelvic pain.
- Digestive disorders: Conditions like irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD) may contribute to pain.
- Pregnancy and Childbirth
Understanding the underlying cause of your pelvic pain is crucial in determining the most effective treatment.
How can pelvic health physiotherapy help in managing pelvic pain?
Pelvic health physiotherapy is a specialized area of physiotherapy focused on the muscles, joints, and tissues of the pelvis. Here’s how it can help:
- Assessment and diagnosis: A pelvic health physiotherapist will conduct a thorough assessment to identify the root cause of your pain, including muscle strength, flexibility, and posture analysis.
- Manual therapy: Techniques such as myofascial release, trigger point therapy, and soft tissue mobilization can help alleviate pain by addressing muscle tension and improving circulation.
- Pelvic floor exercises: Tailored exercises can strengthen or relax pelvic floor muscles, depending on the nature of your pain.
- Education and lifestyle modifications: Understanding how daily activities, posture, and stress contribute to your pain can empower you to make changes that reduce discomfort.
- Biofeedback and relaxation techniques: These can help in retraining your pelvic muscles to function properly without causing pain.
What are the common treatment options for pelvic pain?
Treatment for pelvic pain varies based on its underlying cause but typically includes a combination of the following:
- Medications: Anti-inflammatory drugs, muscle relaxants, and nerve pain medications can provide relief.
- Physiotherapy: Targeted exercises and manual therapies can improve muscle function and reduce pain.
- Injections: Corticosteroid or anesthetic injections may be used to manage pain in specific areas.
- Surgical intervention: In some cases, surgery may be necessary to address structural issues or remove sources of pain, such as endometriosis lesions.
- Alternative therapies: Acupuncture, massage, and yoga can complement traditional treatments by promoting relaxation and reducing stress, which may exacerbate pain.
Your pelvic health physiotherapist will work with you to develop a personalized treatment plan that addresses your specific needs.
How long does it take to see results from pelvic health physiotherapy?
The timeline for seeing results can vary depending on the severity and duration of your pelvic pain, as well as your commitment to the treatment plan. Generally, patients may start noticing improvements within a few weeks of consistent therapy. However, chronic conditions may require several months of treatment to achieve significant relief. Your physiotherapist will regularly reassess your progress and adjust your treatment plan as needed to optimize your recovery.
Can lifestyle changes help manage pelvic pain?
Absolutely! Lifestyle modifications play a crucial role in managing pelvic pain. Consider the following:
- Posture: Improving your posture can reduce strain on your pelvic muscles and nerves.
- Diet: Certain foods can exacerbate pelvic pain, particularly if you have digestive issues. A balanced diet rich in anti-inflammatory foods can be beneficial.
- Stress management: Stress often exacerbates pelvic pain. Techniques like mindfulness, meditation, and breathing exercises can help manage stress levels.
- Regular exercise: Low-impact exercises, such as swimming, walking, or yoga, can improve overall muscle function and reduce pain.
Your pelvic health physiotherapist can guide you in making these changes to enhance your treatment outcomes.
When should I seek help for pelvic pain?
If you experience persistent or severe pelvic pain, it’s important to seek professional help. Early intervention can prevent the pain from becoming chronic and harder to treat. A pelvic health physiotherapist is an excellent first step, as they can assess your condition and direct you to the appropriate treatment options.
What should I expect during my first visit to a pelvic health physiotherapist?
During your first visit, you can expect the following:
- Detailed assessment: Your physiotherapist will ask about your medical history, symptoms, and lifestyle factors.
- Physical examination: This may include an external and internal assessment to evaluate your pelvic muscles, joints, and nerves.
- Discussion of goals: Together, you’ll set realistic goals for your treatment and the physiotherapist will create a treatment plan for you.
- Introduction to treatment: Depending on your assessment, your physiotherapist may begin treatment during your first session and provide you with exercises to do at home.
Navigating pelvic pain can be challenging, but with the right support and treatment, you can regain control over your health and well-being. If you’re struggling with pelvic pain, consider booking an appointment with a pelvic health physiotherapist to explore your treatment options.
Ready to take the first step?
If you’re experiencing pelvic pain and want to explore treatment options, contact us today to schedule a consultation with one of our experienced pelvic health physiotherapists.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 2 locations with pelvic health physiotherapists in Mississauga to help you.













