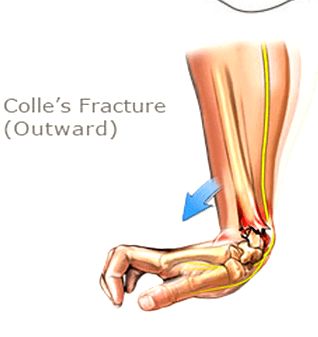
A Colles’ fracture, commonly referred to as a wrist fracture, typically occurs when a person falls onto an outstretched hand. This type of fracture primarily affects the distal radius, the bone located on the thumb side of the wrist. Colles’ fractures are prevalent among older adults, particularly those with osteoporosis, but they can occur at any age. Understanding the nature of this injury, along with effective recovery strategies and preventive measures, is crucial for regaining full functionality of the wrist and minimizing the risk of future injuries.
If you or someone you know has a Colle’s fracture, our physiotherapists at Triangle Physiotherapy can help.
Understanding Recovery
Recovery from a Colles’ fracture generally involves a combination of immobilization, rehabilitation, and lifestyle adjustments. After the fracture is diagnosed—often through X-rays—a healthcare provider may recommend a cast or splint to immobilize the wrist and allow for proper healing. The duration of immobilization can vary, typically lasting between six to eight weeks, depending on the severity of the fracture and the individual’s healing process. Once the cast is removed, the focus shifts to rehabilitation. Recovery times can vary widely, with many patients regaining full function in a few months, while others may take longer. Patience and adherence to a structured recovery plan are essential for optimal healing.
Neuromuscular Exercises post Colle’s Fracture
Neuromuscular exercises are designed to enhance the coordination and communication between the brain and muscles, which is especially important after a wrist injury. These exercises often focus on improving proprioception—the body’s ability to sense its position in space.
1. Wrist and Hand Movements: Start with simple wrist flexion and extension exercises, moving the wrist slowly through its range of motion.
2. Finger Coordination: Practice tapping each finger to the thumb, which helps improve dexterity and coordination.
Incorporating neuromuscular exercises into your recovery routine can significantly aid in regaining strength and functionality.
Mobility Incorporation post Colle’s Fracture
After the initial healing phase, it is crucial to incorporate mobility exercises to restore the full range of motion in the wrist. Gradual stretching and movement help reduce stiffness and enhance circulation.
1. Wrist Circles: Perform wrist circles in both directions to encourage mobility.
2. Tendon Gliding Exercises: These involve moving the fingers and wrist in various positions to promote flexibility and prevent stiffness.
Consistency in these mobility exercises can help ensure a smoother transition back to everyday activities.
Progressive Resistance Exercises
Once mobility is regained, progressive resistance exercises can be introduced to rebuild strength in the wrist and forearm. These exercises should start gently and gradually increase in intensity.
1. Wrist Flexion and Extension with Weights: Using light weights or resistance bands, perform controlled flexion and extension movements.
2. Grip Strengthening: Utilize grip trainers or stress balls to enhance grip strength, which is essential for overall hand function. By progressively increasing resistance, you can strengthen the wrist and surrounding muscles, reducing the likelihood of future injuries.
Prevention
Preventing future Colles’ fractures involves both lifestyle modifications and awareness. Here are some strategies to consider:
1. Fall Prevention: Improve home safety by removing tripping hazards, installing handrails, and ensuring adequate lighting.
2. Bone Health: Engage in weight-bearing exercises and maintain a diet rich in calcium and vitamin D to support bone density.
3. Regular Check-ups: Especially for older adults, regular bone density tests and discussions with healthcare providers about osteoporosis can be critical.
By focusing on prevention, you can significantly lower the risk of future wrist fractures.
FAQs
1. What are the symptoms of a Colles’ fracture?
Symptoms typically include pain and swelling in the wrist, a visible deformity (such as a “dinner fork” appearance), and difficulty moving the wrist or fingers.
2. How long does it take to recover from a Colles’ fracture?
Recovery can vary, but most people see significant improvement within 6 to 12 weeks. Full recovery may take longer, especially for older adults.
3. Can I prevent a Colles’ fracture?
Yes, by improving home safety, maintaining bone health through diet and exercise, and being mindful of your balance and stability, you can reduce your risk of a Colles’ fracture.
4. Are there any long-term effects after recovery?
Some individuals may experience stiffness, reduced range of motion, or chronic pain, particularly if the fracture was severe.
Engaging in rehabilitation exercises can help mitigate these issues. — Understanding and effectively managing a Colles’ fracture is key to ensuring a smooth recovery and maintaining wrist health. By following a comprehensive rehabilitation plan and taking preventive measures, individuals can regain their strength and enjoy a more active lifestyle.
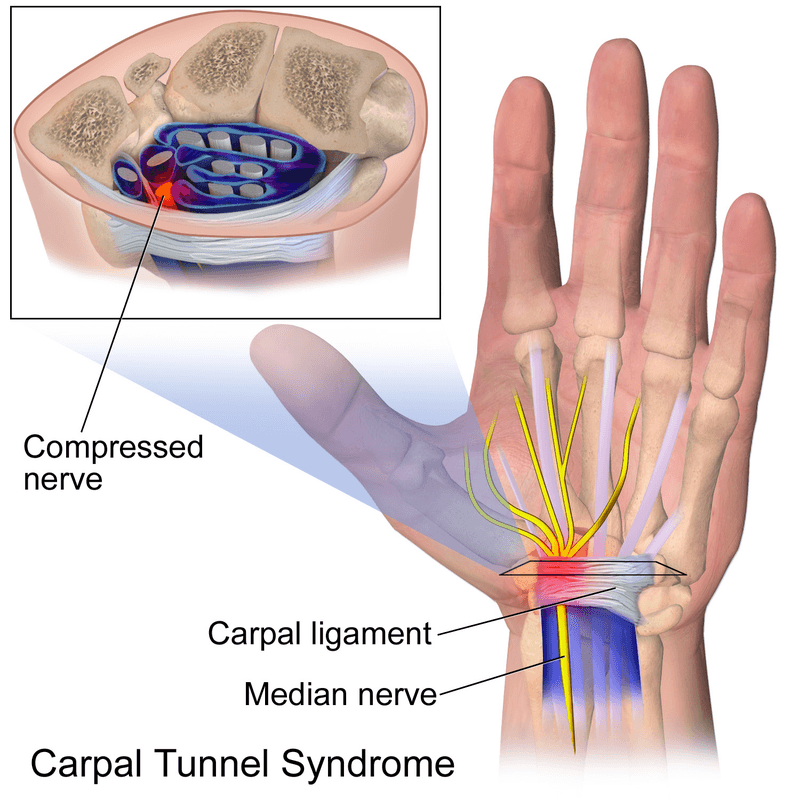
Carpal tunnel syndrome is a painful disorder of the hand caused by the entrapment of the median nerve that passes through the carpal tunnel at the wrist. The wrist bones (carpal bones) form the base of the tunnel and strong ligaments (flexor retinaculum) form the roof. The carpal tunnel contains the median nerve, blood vessels, and tendons that pass to and from your hand. Carpal tunnel syndrome occurs when either the space in the tunnel decreases or when the contents enlarge.
What are the causes of carpal tunnel syndrome?
Some common causes and risk factors include:
- Repetitive hand and wrist movements: Performing repetitive motions with the hands and wrists, especially in awkward positions, can contribute to the compression of the median nerve. This is common in activities such as typing, using a computer mouse, or assembly line work.
- Prolonged wrist flexion: Keeping the wrist in a flexed or extended position for extended periods can increase pressure on the median nerve. This can happen during activities like using a computer keyboard or mouse, playing musical instruments, or using tools that vibrate.
- Anatomical factors: Certain anatomical characteristics, such as having a smaller carpal tunnel or a shape that predisposes to compression, can increase the likelihood of developing carpal tunnel syndrome.
- Trauma or injury: A wrist injury or trauma, such as a fracture or sprain, can lead to swelling and inflammation in the carpal tunnel, compressing the median nerve.
- Medical conditions: Certain medical conditions, such as rheumatoid arthritis, diabetes, and thyroid disorders, can increase the risk of carpal tunnel syndrome. Hormonal changes, such as those that occur during pregnancy or menopause, can also contribute.
- Genetics: There may be a genetic predisposition to carpal tunnel syndrome, as some individuals may have a family history of the condition.
- Obesity: Being overweight or obese may increase the risk of developing carpal tunnel syndrome, possibly due to increased pressure on the median nerve.
Who is most at risk for carpal tunnel syndrome?
Women are more commonly affected by carpal tunnel syndrome than men, possibly due to differences in hand anatomy and hormonal factors.
CTS is more prevalent in individuals who are middle-aged or older. As people age, the risk of developing the condition increases.
What are the symptoms of carpal tunnel syndrome?
- Gradual onset of pain, burning, tingling, or numbness in the median nerve pathway (the thumb, index finger, and middle finger)
- Symptoms may be worse at night or early in the morning
- Symptoms may be relieved by shaking or flicking of the hand
- As the condition progresses, there may be numbness, weakness, and muscle wasting of the thumb muscles causing difficulty with pinching, gripping, and frequently dropping things
Can physiotherapy help with Carpal Tunnel Syndrome?
Physiotherapy treatment for carpal tunnel syndrome:
- Education on rest, activity modification, and workplace ergonomics
- Mobilization of the carpal bones and the median nerve
- Therapeutic ultrasound therapy over the carpal tunnel to speed up healing
- Splinting the wrist during sleep
- Exercises to stretch and strengthen forearm and hand muscles, nerve gliding and correction exercises
- Acupuncture
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Managing Carpal Tunnel Syndrome effectively can improve your quality of life, and Triangle Physiotherapy is here to help. We offer expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists can provide tailored treatment plans to alleviate symptoms and restore function in your hands and wrists.”
Winter weather can be challenging for individuals with arthritis, as cold temperatures and changes in atmospheric pressure can exacerbate joint pain and stiffness. Here are 10 tips to help manage arthritis during the winter months:
- Stay Warm:
- Start your day by using a heating pad or a warm bath or shower to increase the mobility in your joints and reduce pain before you go about your day.
- Dress in layers to trap heat and stay warm.
- Use heated blankets or warm packs on achy joints.
- Protect Your Joints:
- Wear gloves to keep your hands warm and protect your finger joints.
- Use knee-high socks and warm footwear to keep your feet and ankles insulated.
- Stay Active:
- Engage in gentle exercises to keep your joints flexible.
- Consider indoor activities like swimming, which is easy on the joints.
- Maintain a Healthy Weight:
- Excess weight can put more pressure on your joints, so try to maintain a healthy weight through a balanced diet and regular exercise.
- Stay Hydrated:
- Cold weather can lead to dehydration, which may worsen arthritis symptoms. Drink plenty of water to stay hydrated.
- Use Assistive Devices:
- Consider using assistive devices such as canes or braces to reduce the strain on affected joints.
- Manage Stress:
- Stress can exacerbate arthritis symptoms. Practice stress-reducing techniques like deep breathing, meditation, or yoga.
- Warm Up Before Activities:
- Before heading outdoors, warm up your body with gentle stretching exercises to prepare your joints for movement.
- Take Warm Baths:
- Soaking in a warm bath can help soothe joint pain and relax your muscles.
- Consult Your Doctor:
- Keep your healthcare provider informed about changes in your symptoms and discuss any concerns you have about managing arthritis in the winter.

Remember, it’s essential to tailor these tips to your specific situation, as arthritis can affect individuals differently. Always consult with your healthcare provider for personalized advice and treatment options.
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Winter weather can be challenging for those with arthritis, but with the right care, you can manage your symptoms effectively. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists can help you develop strategies to stay active and pain-free during the colder months.”
Gardening is a favourite activity for many people as the summer season arrives. As healthcare professionals, we understand the importance of gardening in promoting physical health and well-being.

Here are some gardening tips to ensure a safe and enjoyable experience:
- Warm-Up Exercises: Treat gardening as a physical activity and warm up before starting. Perform gentle stretches for your back, shoulders, and legs to prepare your muscles for the tasks ahead.
- Maintain Good Posture: Pay attention to your posture while gardening. Bend from your knees and hips, not your back, to avoid strain. Avoid prolonged periods of bending or kneeling; take breaks and change positions frequently.
- Use Proper Lifting Techniques: When lifting heavy objects like bags of soil or pots, bend your knees, keep the object close to your body, and lift with your legs, not your back. Avoid sudden twisting movements.
- Choose Ergonomic Tools: Invest in high-quality, ergonomic gardening tools that reduce strain on your joints and muscles. Look for tools with padded handles and adjustable lengths.
- Start Slowly: If you’re new to gardening or haven’t done it in a while, start with lighter tasks and gradually increase your gardening time and intensity to build endurance and strength.
- Alternate Activities: Vary your gardening tasks to avoid overusing specific muscles. Switch between planting, weeding, and watering to distribute the workload.
- Garden at Waist Height: If possible, create raised garden beds or use elevated planters to reduce the need for bending and kneeling.
- Use Knee Pads or Cushions: Protect your knees by using knee pads or cushions when kneeling on the ground.
- Stay Hydrated: Gardening can be physically demanding, so remember to drink water regularly to stay hydrated, especially on hot days.
- Take Breaks: Listen to your body and take breaks as needed. Use your break time to stretch and relax.
- Ask for Help: If a task seems too challenging or requires heavy lifting, don’t hesitate to ask for assistance from family members or friends.
- Cool Down and Stretch: After gardening, take a few minutes to cool down and stretch your muscles to prevent stiffness and promote flexibility.
What are some common gardening postures that can lead to discomfort or injury?
Several gardening postures can lead to discomfort or injury if not done with proper form and technique. Some common ones include:
- Bending from the Waist
- Kneeling on Hard Surfaces
- Repetitive Twisting
- Overreaching
- Incorrect Lifting
How can I avoid discomfort while gardening?
To avoid discomfort while gardening, consider the following tips:
- Use Proper Posture
- Take Breaks
- Use Knee Pads or a Kneeler
- Alternate Tasks
- Garden at Waist Height
- Use Ergonomic Tools
- Lift Properly
- Stretch Before and After
Can gardening worsen pre-existing musculoskeletal conditions?
Yes, gardening can exacerbate pre-existing musculoskeletal conditions if proper precautions are not taken. People with conditions like osteoarthritis, back pain, or joint issues may be more susceptible to discomfort or injury while gardening. However, with proper body mechanics, adaptive tools, and awareness of limitations, gardening can still be enjoyed safely. It’s essential for individuals with pre-existing conditions to consult their physiotherapist or chiropractor before engaging in gardening to get personalized recommendations and precautions.
I often experience neck and shoulder pain after a day of gardening. How can I prevent this discomfort?
Neck and shoulder pain after gardening can result from poor posture and overuse of certain muscles. Here’s how to prevent discomfort:
- Maintain Proper Posture: Keep your head aligned with your spine and avoid prolonged forward head posture while working in the garden.
- Avoid Overreaching: Use gardening tools with extended handles to reduce strain on your shoulders. Avoid overreaching when pruning or planting.
- Take Frequent Breaks: Schedule regular breaks during gardening to rest your neck and shoulder muscles.
- Incorporate Shoulder Exercises: Perform shoulder-strengthening exercises recommended by a physiotherapist to improve muscle endurance and stability.
- Warm-Up Before Gardening: Engage in light shoulder and neck stretches to prepare your muscles for gardening tasks.
- Use Proper Lifting Techniques: Lift objects close to your body and use your leg muscles to minimize strain on your neck and shoulders.
- Ice and Heat Therapy: Apply ice to sore areas after gardening to reduce inflammation, and use heat packs to relax tense muscles.
Can gardening worsen my existing back condition? Can physiotherapy help?
Gardening can potentially worsen existing back conditions if proper precautions are not taken. Physiotherapy can certainly help to alleviate back pain and prevent it from affecting your gardening game. Individuals with back issues should consider the following:
- Consult a Physiotherapist: Seek advice from a physiotherapist to assess your back condition and receive personalized recommendations for gardening.
- Avoid Heavy Lifting: Refrain from lifting heavy objects that could strain your back. Use lightweight containers and gardening tools.
- Choose Low-Impact Tasks: Opt for low-impact gardening activities such as container gardening or raised beds to minimize strain on your back.
- Use Assistive Devices: Consider using gardening tools with ergonomic designs or assistive devices to reduce stress on your back.
- Pace Yourself: Take frequent breaks and limit the duration of gardening sessions to avoid overexertion.
- Engage in Back Exercises: Perform back-strengthening exercises prescribed by your physiotherapist to improve the stability and flexibility of your spine.
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Gardening is a rewarding activity, but it’s important to stay injury-free during the summer. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you prevent and manage injuries, ensuring that you can enjoy your gardening activities all season long.”
Yoga has been gaining immense popularity lately, due to the short-term as well as long-term benefits that it provides. Practicing yoga provides a strong spiritual element that offers fitness and flexibility. People suffering from various health disorders can find solutions through yoga, and they may reap the extra benefits yoga provides through living a more stress-free lifestyle as well as with increased fitness.
Yoga for a healthy life
Yoga is an ancient system of health that promotes ‘union’ and connects the body, mind, breath and spirit as one unit, therefore enhancing and promoting an overall balanced lifestyle of health and well-being.
Also read, Best Physiotherpist in Oakville

If practiced regularly the benefits of yoga are numerous. Physically and mentally, yoga may result in:
- Improvement in muscular strength
- Endurance
- Flexibility
- Body awareness
- Circulation
- Digestion
- Hormonal balance
- Normalizing blood pressure
- Weight loss
- Pain relief
- Alertness
- Concentration
- Improvement in sleep
- And much, much more!
It is believed that we only have a limited number of breaths in each life. Hence,yoga is believed to stretch our lives out a bit longer by taking slow and deep breaths.
Also read, Physiotherapy Treatment in Mississauga
Research has also suggested that yoga improves social and occupational functioning in schizophrenic patients.
Styles:
Some styles of yoga emphasize breathing and meditation, with limited activity; some styles emphasize form and alignment through postures, some are about a serious workout and flow, & some are all about relaxation.
Not a competition:
Don’t try a posture that you are uncomfortable with; don’t let someone else push you into something that you don’t want to do; and don’t think that you have to compete with yourself or others to achieve a posture.
Yoga is not about competition or feeling the burn. However, a little discomfort is to be expected. There is a huge difference between pain and discomfort, and most people mistake one for the other, especially when they are new to yoga practice.
Consult A Physiotherapist
At Triangle Physiotherapy, we work with the help of your medical history and assess how yoga may help guide your health in the right direction. All you need to do is overlook your anxieties related to your health, and feel free to contact any of our five locations for an in-depth consultation.
Incorporating yoga into your routine can enhance flexibility, strength, and overall well-being, and combining it with physiotherapy can optimize these benefits. For those seeking professional physiotherapy services to complement their yoga practice, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and tailored treatment plans to support your physical health journey.
Massage therapy has a positive effect on a plethora of medical conditions. It rejuvenates both your mind and muscles. Everyone experiences pain, the only difference is some continue to suffer and some proactively seek pain relief through massage therapy. Our skin is the largest organ in our body. The skin interfaces with the environment and is the first line of defense from external factors. Taking good care of your skin through massage therapy will help keep your skin healthy and muscles rejuvenated. Massage therapy is regarded as one of the oldest healthcare professions. Massage therapy is not just for the skin and muscles, it can also help to reduce high blood pressure, lower chances of depression and relieve headaches.

Also read, Physiotherapy Etobicoke
Healing from a car accident injury through massage therapy
Car accidents can cause a variety of physical problems, and many people seek physiotherapy and/or massage therapy for relief from whiplash and other aches and pains. Massage therapy has the potential for facilitating health, wellness, and injury recovery from car accidents.
Massage therapy can relieve Whiplash
Whiplash injuries are common in car and sports accidents. People who get whiplash may experience pain, stiffness, and poor range of motion, among other symptoms. Some people may feel mental or emotional symptoms such as loss of memory or focus, insomnia, and depression. If you have whiplash, ask your physician about adding massage to your physical therapy regimen, as the combination could help speed up your recovery.
- Massage Therapy for Knee Injuries
People in car accidents often injure their knees (though not as often as heads, necks, and spines). Statistics show car crash victims often injure their Anterior Cruciate Ligaments (ACLs), as do many athletes. Massage therapy has been shown to provide pain relief and healing for people with a wide variety of knee problems.
Also read, Physiotherapy Clinic in Oakville
- Massage therapy helps to recover from Immediate emotional trauma
If you’re in a car crash, you may suffer emotionally even if you do not sustain any physical injuries. Massage therapy, especially within several hours of an auto accident, can help people recover their emotional balance.
We all suffer from adverse health effects both psychological and physical, and stress is one of the important factors to look after. A massage can help reduce everyday stress by helping muscles to relieve and relax through the pressure points manually worked on by one of our experienced massage therapists.
Our registered massage therapists at Triangle Physiotherapy are happy to assist you with any questions pertaining to your health goals and guide you on the road to recovery. Adding massage therapy to your healthcare/recovery plan will provide natural relief without the aid of painkillers. Living pain-free naturally is our goal, and at Triangle Physiotherapy, we will guide you every step of the way.
Massage therapy is a great way to relax, reduce muscle tension, and promote overall well-being. For those looking to combine massage therapy with physiotherapy services, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and personalized treatment plans to help you achieve optimal health and relaxation.
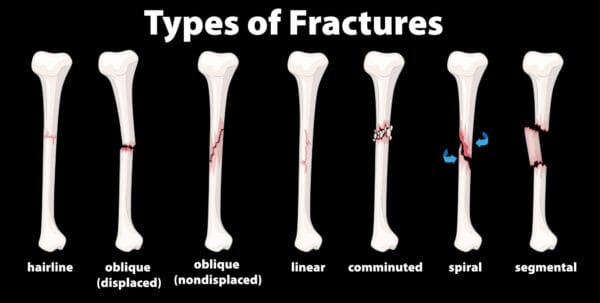
There are many forms of fractures, each causing a dilemma in our lives and requiring the help of a physiotherapist in order to heal safely and adequately. One of the most common types of fractures seen in sports medicine today is called a “hairline” or “stress” fracture. Hairline fractures are caused by repetitive strain and excess training. Hairline fractures are minute cracks on the bones, which can become severe if not immediately treated. The main causes of hairline fractures are:
- Traumatic Incidents
- Repetitive Stress
- Pathological
Also read, Physiotherapy Clinic in Mississauga
Causes of Fractures
Basically, hairline fractures are caused by the depressed response of the bone with the ground reaction forces that are applied to the bones during certain activities such as: running, jumping, or walking. Symptoms may include pain and tenderness to the affected bone. Repetitive stress or a sudden fall or strike to the area can also cause hairline fractures.
Treatment of Fractures
The best way to treat a hairline fracture is to refrain from any activities that can aggravate the injury. Recovery time can span from two weeks to a month and a half. Once the bone is healed from its minute cracks, you can gradually resume normal activities. In extreme circumstances, the affected area must be put at rest and must be immobilized by casting or bracing. The stages of healing a fracture through physiotherapy are as follows:
- Muscle Assessment
- Joint Mobilisation
- Massage Therapy
- Heat and Electro Therapy
- Gait Education
Also read, Physiotherapy Oakville
Shoe inserts like supportive orthotics and walking crutches may also be recommended by your physiotherapist. Treatment through physiotherapy is advised through strengthening exercises that are non-weight bearing like swimming. Luckily, hairline fractures rarely need surgery because they can easily be mended with just two weeks of rest. However, the injury can worsen if not given the proper medical attention.
If you happen to suffer from a hairline fracture and you are looking for a way to relieve pain, and recover from an injury, adding physiotherapy to a routine wellness plan can maximize recovery time and optimize your healing process. Our physiotherapists at Triangle Physiotherapy can be a powerful ally when combating daily stress, muscle pain, and general health issues regarding hairline fractures. Not only does physiotherapy relieve pain, increase energy levels, and improve overall physical and mental performance, it prevents further injuries.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
The experienced, professional physiotherapists at Triangle Physiotherapy are available at eight convenient locations:
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Recovering from a hairline fracture requires careful management and effective physiotherapy to restore strength and prevent further injury. If you are seeking professional physiotherapy services to support your recovery, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and personalized treatment plans to help you heal properly and regain full function.
What is ALS?
Amyotrophic lateral sclerosis (ALS) is the most common type of adult-onset motor neuron disease. Neurological disorders are characterized primarily by progressive degeneration and loss of motor neurons. ALS involves upper and lower motor neurons and presents as an idiopathic, progressive degeneration of anterior horn cells and their associated neurons, resulting in progressive muscle weakness, atrophy, and fasciculations.
What are the symptoms of ALS?
ALS is a gradual-onset disease. The first initial symptoms of ALS vary from person to person. One person may have trouble with their grip, such as holding a cup or pen, while another person may experience a change in pitch in their voice while speaking. The rate at which ALS develops also varies from person to person, with the mean survival time ranging from three to five years.
Although there are cases in which people have lived five, and ten or more years. Onset symptoms can begin in the muscles that control speech and swallowing, or in the hands, arms, legs, or feet. Not all people who suffer from ALS experience the same symptoms as others or the same sequences or patterns of progression. Although, universally progressive muscle weakness and paralysis are experienced.
How is ALS diagnosed?
ALS is a somewhat difficult disease to diagnose. There is not one test or procedure to instantly establish the diagnosis of ALS. Through the use of clinical examination, and a series of diagnostic tests, often ruling out other diseases that mimic ALS, that a diagnosis can be established. A comprehensive diagnostic check-list includes most, if not all, of the following procedures:
- Electrodiagnostic tests- Electromyography (EMG) and Nerve conduction velocity (NCV)
- Blood & Urine studies
- Spinal tap
- X-rays including MRI
- Myleogram of cervical spine
- Muscle and/or nerve biopsy
- A thorough neurological examination
These tests are done at the discretion of the physician, usually based on the results of other diagnostic tests and the physical examination. There are several diseases that have some of the same symptoms as ALS, and most of these conditions are treatable.
What are the treatments for ALS?
Treatment of ALS can be done with physiotherapy, focusing on stretching and daily range of motion (ROM) exercises. Our physiotherapists at Triangle will focus on the emphasis of energy conservation and teach patients and caregivers methods for performing safe, efficient transfers. They can also provide instruction for strengthening exercise programs.
In one study, individualized, moderate-intensity, endurance-type exercises for the trunk and limbs performed 15 minutes twice daily were shown to significantly reduce spasticity as measured by the Ashworth scale. At Triangle, we may have to recommend wheelchairs to anticipate the patient’s future needs. Initially, a lightweight wheelchair should be rented, with future plans to purchase a heavier chair when the patient is no longer able to ambulate. Modifications will be recommended on the basis of the patient’s condition and tolerance for gadgets.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy is a crucial component in managing ALS, helping to maintain mobility, reduce discomfort, and improve quality of life. For those seeking specialized physiotherapy services to support ALS management, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans tailored to the needs of individuals living with ALS.
What is Carpal Tunnel Syndrome?
Carpal Tunnel Syndrome (CTS) is a wrist and hand condition that occurs when a nerve becomes pinched within a tunnel created by the bones of the wrist. The wrist is composed of 8 small bones called Carpals,which, along with ligaments, create a ‘Carpal Tunnel’ on the palmer side of the forearm. This tunnel creates a space for the passage of the Median nerve and theflexor tendons of the fingers. The Median nerve provides both sensory and motor function to the hand, and if it becomes compromised within this space, Carpal Tunnel Syndrome will occur.

Symptoms:
Symptoms of CTS are numbness, pain, and weakness in the affected wrist and hand. Numbness and pain occur along the sensory distribution of the Median nerve, which includes the palmer side of the thumb, index finger, third finger and lateral half of the ring finger. The progression of symptoms is typically gradual, beginning with itching, tingling or mild burning, and in chronic cases can progress to complete numbness, and involve radiating pain up the arm, decreased grip strength and muscle wasting in the thumb.
Common Causes:
CTS is often due to a combination of multiple factors that result in increased pressure on the Median nerve in the carpal tunnel. This condition is rarely due to an issue with the nerve itself. A common contributing factor to CTS is size of the carpal tunnel, as the smaller the passageway, the greater the likelihood of tendon and Median nerve compression. Women on average have smaller and narrower carpal tunnels then men, making them more prone to CTS. Another contributing factor is injury or trauma to the wrist, because the resultant swelling increases the amount of pressure and decreases the amount of space within the carpal tunnel. Repetitive strain injuries to the wrist can cause inflammation and swelling of the synovial fluid surrounding the flexor tendons, which also decreases the space within the carpal tunnel. These repetitive strain injuries can often occur in the workplace, due to use of vibrating tools and machinery, or repetitive typing and use of a mouse at a computer workstation.
Treatment:
Physiotherapy is often used to help treat Carpal Tunnel Syndrome. Therapy for this condition focuses on proper education about the condition and necessary activity modification, prescription of stretching and strengthening exercises and therapeutic modalities as appropriate. Additionally, bracing can be used to help provide wrist support and stability. Wrist bracing is most effective at night to prevent wrist flexion, and during the day while performing repetitive wrist activities. Occasionally, surgical intervention is required for the treatment of CTS, in which the connective tissue creating the roof of the carpal tunnel is cut to create more room for the Median nerve. Physiotherapy rehabilitation is recommended post-surgery to ensure an optimal outcome.
For more information about Carpal Tunnel Syndrome, ask your physiotherapist at Triangle Physiotherapy and Rehabilitation!
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Managing carpal tunnel syndrome effectively often requires physiotherapy to reduce pain, improve hand function, and prevent further injury. If you are seeking professional physiotherapy services for carpal tunnel syndrome, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide specialized care and customized treatment plans to help you regain hand strength and mobility.










