Pelvic Health physiotherapists advocate the importance of educating individuals about their pelvic health. They are often asked by patients if an internal exam is necessary. Many patients refrain from seeking help for pelvic health issues because of the fear of internal examination. While internal exams are not a must, they can be very helpful to pelvic health physiotherapists in determining the condition of the pelvic floor.
What is an Internal Pelvic Exam?
A pelvic floor assessment, which may or may not include an internal pelvic exam, entails a pelvic health physiotherapist examining the pelvic floor muscles, tissues, and organs by inserting a gloved hand into the vagina or rectum. This examination is crucial for assessing the well-being and performance of the pelvic floor, allowing for the detection of any possible problems or issues.
Why is an internal pelvic exam important?
- Detailed Assessment of Pelvic Floor Muscles: An internal pelvic exam allows the physiotherapist to assess the tone, strength, flexibility, and coordination of the pelvic floor muscles. This information is crucial in developing an accurate understanding of the patient’s pelvic health.
- Identification of Muscle Imbalances: Through internal palpation, a physiotherapist can identify any muscle imbalances or asymmetries in the pelvic floor. This helps in tailoring the treatment plan to address specific issues, such as hypertonic (overactive) or hypotonic (underactive) muscles.
- Assessment of Pelvic Organ Function: Internal examination enables the physiotherapist to assess the function of pelvic organs, such as the bladder, uterus, and rectum. This is important in cases where dysfunction or weakness in the pelvic floor muscles may be contributing to issues such as urinary incontinence or pelvic organ prolapse.
- Evaluation of Connective Tissues and Nerves: The internal exam allows the physiotherapist to assess the condition of connective tissues, ligaments, and nerves in the pelvic region. Dysfunction in these structures can contribute to pelvic pain and other symptoms, and the internal exam helps in identifying such issues.
- Assessment of Trigger Points and Tenderness: The physiotherapist can identify trigger points and areas of tenderness within the pelvic floor muscles. This information is crucial in designing a targeted treatment plan, which may include manual therapy techniques to release muscle tension.
- Feedback on Exercise Performance: During an internal pelvic exam, the physiotherapist may guide the patient through specific exercises to assess the effectiveness of pelvic floor muscle contractions. Real-time feedback helps the patient learn proper muscle engagement and control.
- Patient Education and Empowerment: The internal exam provides an opportunity for the physiotherapist to educate the patient about their pelvic floor anatomy, function, and any specific issues identified during the assessment. This empowers the patient to actively participate in their treatment plan and make lifestyle changes that support pelvic health.

Do I have to have an internal exam during a pelvic health assessment?
It’s important to note that internal pelvic exams are conducted with the patient’s informed consent, and physiotherapists ensure a comfortable and respectful environment during the assessment. The goal is to provide comprehensive care and address the specific needs of individuals experiencing pelvic health issues. That being said, if you are not comfortable being internally examined, please let your physiotherapist know before the start of your assessment.
How do I prepare for an internal pelvic exam?
Preparing for an internal pelvic exam involves a combination of physical and mental preparation. It’s essential to communicate openly with your pelvic health physiotherapist and follow their instructions. Here are some general guidelines to help you prepare:
Comfortable Clothing: Wear comfortable, easy-to-remove clothing. You may be asked to undress from the waist down, so wearing a skirt or loose pants can be convenient.
Relaxation Techniques: Practice relaxation techniques such as deep breathing to help ease anxiety and tension. Relaxing your pelvic muscles can make the exam more comfortable.
Communicate with your Physiotherapist: Inform your pelvic health physiotherapist about any concerns, fears, or past traumatic experiences related to pelvic exams. They can adjust their approach and provide additional support.
Ask Questions: Feel free to ask any questions you may have about the procedure. Knowing what to expect can help alleviate anxiety.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Understanding the need for an internal exam during a pelvic health assessment can help you make informed decisions about your care. If you’re looking for specialized support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can provide comprehensive pelvic health assessments tailored to your comfort and needs.
Menopause can be a very overwhelming time for a lot of women. During this period, there are a lot of hormonal changes that can influence the way you feel in your body. Menopause tends to start between the ages of 45 to 55. This can include a range of symptoms such as hot flashes and mood swings to vaginal dryness and changes in pelvic health.

How does Menopause affect pelvic health?
Many women don’t realize that menopause can affect pelvic health. As estrogen levels decline, tissues in the vagina, urethra, and bladder can become thinner, drier, and less elastic, leading to a condition called vaginal atrophy. This can cause uncomfortable symptoms such as vaginal dryness, itching, burning, and pain during sex. In addition, menopause can also increase the risk of pelvic floor disorders, such as incontinence and prolapse. But don’t worry, many of these conditions can be improved through pelvic physiotherapy!
What is pelvic floor physiotherapy?
Pelvic floor physiotherapy is a specialized form of physiotherapy that focuses on the pelvic floor muscles, which support the pelvic organs (bladder, uterus, and rectum) and control bladder and bowel function. Pelvic physiotherapy can help to improve pelvic health during menopause and beyond, providing relief from uncomfortable symptoms and reducing the risk of pelvic floor disorders.
What does Pelvic Health Physiotherapy Involve?
Pelvic floor physiotherapy involves a range of techniques designed to improve the strength, coordination, and function of the pelvic floor muscles. These techniques may include pelvic floor exercises, biofeedback, electrical stimulation, manual therapy, and education on lifestyle modifications. It is an effective alternative to drug based therapy and surgery, and allows for you to take your health into your own hands.
How Can Pelvic Physiotherapy Help During Menopause?
- Pelvic physiotherapy can help to address a range of pelvic health issues that can arise during menopause, including:
- Vaginal Dryness: Pelvic physiotherapy can help to improve blood flow to the vaginal area, which can increase lubrication and reduce discomfort during intercourse. Additionally, exercises to strengthen the pelvic floor muscles can help to improve vaginal tone and elasticity.
- Urinary Incontinence: Pelvic physiotherapy can help to strengthen the pelvic floor muscles that support the bladder, which can improve bladder control and reduce urinary incontinence.
- Prolapse: Pelvic physiotherapy can help with prolapse symptoms or post-hysterectomy. With a prolapse, there is commonly increased muscle tone causing the organ to descend. This can be improved with exercise and treatment. Post hysterectomy, there can be pelvic floor weakness or altered sensation internally which can also be treated through strengthening and sensitization work.
- Painful Intercourse: Pelvic physiotherapy can help to improve vaginal tone and elasticity, which can reduce pain and discomfort during intercourse.
How can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“While menopause symptoms can be challenging, they are not inevitable for everyone and can be managed with the right care. Triangle Physiotherapy offers specialized services to help you navigate this stage of life across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can provide personalized treatment plans to alleviate symptoms and improve your quality of life.”
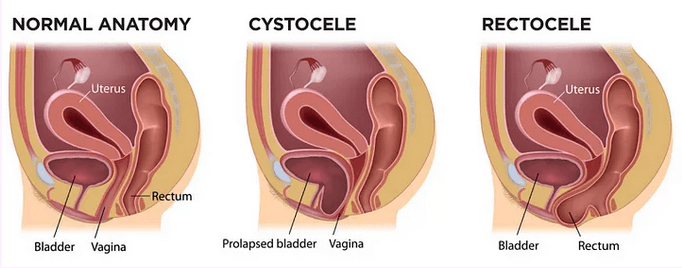
Pelvic organ prolapse (POP) is a condition in which there is a descent of the pelvic organs into or through the vaginal or anal canal. This can present as:
- a visible bulge in the above openings,
- pressure felt in the pelvic area,
- incomplete emptying of bladder or bowels,
- discomfort during intercourse.
The main reason for prolapse is increased pressure on the pelvic floor due to:
– Chronic constipation
– Bearing children
– Pelvic floor weakness due to hormonal imbalance
Conservative non-surgical management is the first line of treatment for POP.
Your pelvic floor physiotherapist will assess the severity of your symptoms, the strength of your pelvic floor and your ability to manage pressure and stresses to your pelvic floor. Treatment would include strengthening exercises for the core and pelvic floor muscles and coordination techniques for all the inner unit muscles.
The types of pelvic organ prolapse are:
- Anterior Wall Prolapse
- Posterior Wall Prolapse
- Rectal Prolapse
Depending on the grade and type of prolapse, you might be a candidate for a pessary fitting.

A pessary is a medical grade silicone device that is inserted into the vaginal canal in order to support the vaginal walls. If you are a candidate for a pessary, it must be fitted for you by a trained professional such as gynaecologists, nurses that have a certification in fittings or pelvic health physios that are specialized to do so.
We currently have 3 practitioners at Triangle Physiotherapy who are certified in pessary fittings.
Your pelvic floor deserves more than just kegels. Speak to a pelvic health physiotherapist today to get started!
Where can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Written by Roshni Ravi, Pelvic Health Physiotherapist
Have you ever experienced pain with sex? A burning sensation during or afterwards, a sharp pain or general discomfort? A lot of these symptoms point towards a common condition called dyspareunia. This is also known as pain with intercourse. It is a common condition postpartum, during menopause or even just due to general pelvic floor dysfunction.
But don’t worry, there are ways to alleviate the discomfort and enjoy a fulfilling sex life again! One of the most effective methods is through pelvic health physiotherapy.
Pelvic health physiotherapy involves working with a trained professional to strengthen and stretch the muscles in your pelvic floor, which can become weakened or tight due to a variety of factors. By doing so, you can improve your pelvic floor function and reduce pain during sex.
When it comes to sexual dysfunction, pelvic physiotherapy can be an effective treatment option for women. Pelvic physiotherapy can help address issues such as pain during intercourse, difficulty achieving orgasm, or vaginismus (involuntary contraction of the vaginal muscles).
What does a treatment session entail?
During a pelvic physiotherapy session, you’ll typically undergo an initial evaluation where your therapist will assess your pelvic floor muscles and create a personalized treatment plan. The exercises and techniques used will vary depending on your specific needs and goals, but they may include:

- Pelvic floor relaxation exercises
- Deep breathing
- Yoga based therapy
- Functional strengthening such as squats
- Biofeedback and/or muscle stimulation
It’s important to note that pelvic physiotherapy isn’t a quick fix and may take several sessions to see results. However, with dedication and commitment, it can significantly improve your quality of life and sexual function. So if you’re experiencing dyspareunia, don’t suffer in silence. Talk to your healthcare provider about pelvic physiotherapy and take the first step towards a happier, healthier you.
Book your consultation with a pelvic health physiotherapist today. We have pelvic health physiotherapists at all eight of our locations.
Where can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin
“Revitalizing your relationship and reclaiming your sex life can be achieved with the help of pelvic floor physiotherapy. Triangle Physiotherapy offers specialized services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can help you address pelvic floor issues and enhance intimacy through personalized treatment plans.”
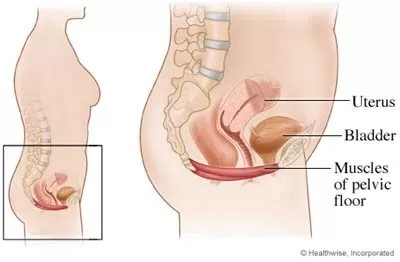
What is the Pelvic Floor?
The pelvic floor is a set of muscles that spread across the bottom of the pelvic cavity like a hammock. The pelvic floor has three openings that run through it, the urethra, the vagina, and the rectum. The functions of the pelvic floor include:
- Supporting the pelvic organs, specifically the uterus, the bladder, and the rectum
- To help provide sphincter control for the bladder and bowel
- Withstanding increases in pressure that occur in the abdomen such as coughing, sneezing, laughing, straining, and lifting
- To enhance the sexual response
What causes pelvic floor dysfunction?
The pelvic floor becomes dysfunctional in many women when there is an imbalance in the joints, muscles, and connective tissue integrity.
- Weak pelvic floor muscles: contributing to stress incontinence, urge incontinence, and pelvic organ prolapse.
- Tight pelvic floor muscles: contributing to Urinary and Fecal Urgency, Urge Incontinence, Chronic Pelvic Pain, Dyspareunia, Vaginismus, Vulvodynia, Pudendal Neuralgia, Interstitial Cystitis and Chronic Prostatits.
One of the most commonly seen conditions by pelvic physiotherapists is stress incontinence in women.

What is Stress Urinary Incontinence?
Stress urinary incontinence is the involuntary release of urine during laughter, coughing, lifting of objects or any movement that increases pressure on your bladder. When the bladder is full, the muscles in the wall of your bladder contract forcing urine through the urethra and out of your body. Sphincter muscles and pelvic floor muscles keep the urethra closed to avoid leakage of urine. These muscles relax at the same time the bladder contracts in order to allow urine to exit your body.
Causes of stress incontinence:
Hormonal changes:
During the week before your menstrual cycle, estrogen levels fall, causing symptoms of stress urinary incontinence to worsen. Additionally, as a woman goes through menopause, estrogen levels also fall causing the pelvic floor muscles to weaken.
Pregnancy:
If you are pregnant, you may experience stress urinary incontinence due to hormonal changes and the enlarging size of the uterus. During pregnancy, estrogen levels are lower, leading to less muscular strength in the sphincter and pelvic floor muscles. Additionally, as the fetus grows extra weight is placed on your bladder.
Childbirth:
Vaginal delivery can damage your pelvic floor muscles making urine leakage more likely. The supporting tissues of your bladder can also be damaged during vaginal delivery causing a cystocele, or prolapse of your bladder, symptoms of which include urinary incontinence. You may not know you have suffered damage to your pelvic floor until after you have gone through menopause, when the pelvic floor muscles are further weakened due to a fall in estrogen levels.
Hysterectomy and other surgery:
The bladder and uterus are very close together and have common supporting ligaments and muscles. Surgery to, or removal of your uterus as in a hysterectomy, risks damage to the supporting structures of your bladder. If these supporting structures are damaged, a cystocele is likely to occur. Symptoms of a cystocele include urinary incontinence.
Illnesses:
When you are ill and suffering from severe coughing, the pelvic floor muscles may fatigue and allow temporary stress incontinence due to an increase in abdominal pressure experienced while coughing.
Obesity:
Obesity can increase the abdominal pressure on the bladder leading to urinary incontinence.
Neurological damage:
Any neurological disorder such as multiple sclerosis, Parkinson’s disease or stroke can cause urinary incontinence by interfering with the nerve signals that control your bladder. Additionally, if the nerves that supply your bladder or pelvic floor muscles are damaged, urinary incontinence may also result
How is Stress Urinary Incontinence treated?
Treatments of stress urinary incontinence are individual based. The following should be considered:
Pelvic floor muscle strengthening:
Strengthening the supporting muscles of your bladder is very effective inhelping stress urinary incontinence.
Bladder training
Bladder training involves learning to delay the urge to urinate. You areinstructed to breathe deeply, relax, and distract yourself with another activitywhen you feel the urge. The initial goal is to delay urination by increments and eventually once every2 to 4 hours.
Pessary
Pessaries can help when a cystocele or prolapsed bladder is the cause forurinary incontinence. A pessary is a device of various shapes and sizes that isplaced in the vagina to support the bladder and keep it in place.
Surgery
For severe cystoceles, or bladder prolapses, surgery is needed in order tocorrect the position of the bladder and help with urinary incontinence.
Important Tips
- Avoid constipation. Repeated straining can have a very damaging effect on the pelvic floor muscles.
- It’s important for women to be active. Regular exercise and recreational sporting activities play a key role in keeping women fit and healthy well into old age
- Drink plenty of water
- Learn to tighten your pelvic floor muscles before you cough, sneeze or lift heavy items.
To get your pelvic health assessed, schedule a consultation with a pelvic floor physiotherapist at Triangle Physiotherapy and Rehabilitation!
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Maintaining a strong pelvic floor is essential for overall health, especially in managing incontinence, pelvic pain, and postpartum recovery. For those seeking professional physiotherapy services to strengthen their pelvic floor, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and personalized treatment plans to help you achieve optimal pelvic health and well-being.