Every journey to a new country comes with its own challenges – physical, emotional, and social.
At Triangle Physiotherapy, we believe that caring for your health means more than just treating pain. For many newcomers and refugees in Toronto, physiotherapy plays a crucial role in helping them rebuild, restore, and thrive in their new lives.
From stress-induced muscle tension to injuries sustained during migration or early work experiences, the physical toll of relocation is often underestimated. That’s why we offer care that’s not just effective – but personalized to every individual’s story, needs, and goals.
Unique Challenges Faced by Newcomers & Refugees
The path to settling in Canada isn’t always easy. Many people arrive after long flights, extended travel, or even physically dangerous circumstances. Once here, they may face:
- Lingering pain from old or untreated injuries
- Postural issues from long hours of travel or manual work
- Chronic stress that manifests physically in the neck, shoulders, or back
- Language barriers when accessing healthcare
- Lack of awareness about available support systems
- Mental and emotional strain that affects the body
At Triangle Physiotherapy Toronto, we understand these unique layers – and we tailor our treatment accordingly.
Why Personalized Physiotherapy Matters

A one-size-fits-all approach simply doesn’t work. Your body, your background, and your goals are unique – and your care plan should reflect that.
We focus on understanding:
- The physical impact of your migration journey
- Cultural comfort with therapy and bodywork
- Your daily routine, work type, and movement patterns
- Past medical or injury history
- Emotional stress and how it may be showing up in your body
Our Personalized Approach to Physiotherapy for Newcomers
Step 1: Comprehensive, Culturally Sensitive Assessment
We begin with a thorough evaluation, including:
- A conversation about your journey, stressors, and pain
- Review of any old injuries or chronic issues
- Functional movement tests to assess posture, strength, and mobility
- Multilingual support when possible, and patience always
Our goal is to meet you where you are – both physically and emotionally.
Step 2: A Customized Recovery Plan
Based on your assessment, we’ll create a treatment plan that may include:
- Manual therapy to release tension and improve mobility
- Exercises tailored to your physical demands (work, caregiving, etc.)
- Education on body mechanics and posture
- Pain relief modalities like ultrasound or TENS
- Resources for additional wellness or community care
Step 3: Ongoing Support for Lasting Recovery
As you settle into life in Toronto, your needs may evolve. We adjust your plan accordingly, tracking progress and ensuring you feel supported every step of the way.
The Benefits of Individualized Physiotherapy for Newcomers
- Faster Recovery from Stress & Injury
- Improved Body Awareness and Confidence
- Supportive, Respectful Care in a New Environment
- Tools to Stay Healthy in Work and Daily Life
A Safe Space to Heal and Grow
Whether you’re recovering from an old injury or simply trying to adjust to the physical toll of a new life, you don’t have to do it alone. At Triangle Physiotherapy Toronto, we’re proud to support newcomers and refugees with compassionate, expert care – one step at a time.
Book your assessment today and let us support your journey to a stronger, healthier future in your new home.
Your recovery journey made simple at Triangle Physiotherapy Toronto
Starting physiotherapy can feel overwhelming – especially if you’re dealing with pain, a new diagnosis, or recovery from surgery. At Triangle Physiotherapy Toronto, we believe your treatment plan should feel like a roadmap, not a maze.
Whether it’s your first session or you’re resuming after a gap, this step-by-step guide breaks down what to expect so you can feel confident and informed at every stage of your care.
Step 1: Your Initial Assessment
Your first appointment is all about understanding you – your body, your pain points, and your goals. During this one-on-one session, your physiotherapist will:
- Review your medical history and lifestyle
- Assess movement, strength, and alignment
- Ask about your symptoms, concerns, and expectations
- Identify the root cause of the issue – not just the symptoms
This assessment forms the foundation of your personalized physiotherapy treatment plan. No two bodies are alike, so we tailor everything to your specific needs.
Step 2: Goal Setting and Planning
Once we know what we’re working with, we’ll talk about realistic recovery goals – both short-term (like reducing pain) and long-term (like returning to work, sports, or daily activities).
You’ll be part of every decision, so your treatment plan fits your schedule, comfort level, and lifestyle. Some plans may be a few weeks long, others more depending on the condition.
Step 3: Active Treatment Begins
Your sessions may include a combination of:
- Manual therapy: Hands-on techniques to improve mobility and reduce tension
- Exercise therapy: Strength, flexibility, and balance training
- IMS : Regaining neuromuscular function
- Modalities: Heat, ice, ultrasound, or electrical stimulation
- Postural or movement corrections: Guidance on how to move better and avoid re-injury
Each visit builds on the last, with your therapist monitoring progress and adjusting techniques as needed.
Step 4: Home Exercises & Self-Care
A major part of your recovery happens outside the clinic. You’ll be given a home exercise plan – designed to reinforce progress and keep you moving safely between sessions.
We’ll also help you understand:
- How to manage flare-ups
- When to rest vs. when to move
- Everyday habits that support healing
Think of your therapist as a coach – giving you the tools to take charge of your own recovery.
Step 5: Progress Reviews and Plan Adjustments
Every few sessions, we’ll assess how things are going. Are you stronger? More mobile? Less reliant on pain meds? Based on the progress, your treatment plan may:
- Stay the course
- Introduce more advanced exercises
- Shift focus if a new issue surfaces
We adjust your care as you grow – because healing isn’t always linear, and that’s okay.
Step 6: Discharge Planning and Maintenance
Once you’ve met your goals, we’ll prepare you for a safe, confident discharge. You’ll receive a maintenance plan that includes:
- Exercises to continue at home
- Tips for staying injury-free
- Follow-up options if anything returns
Our goal is to empower you – not make you dependent on us.
Your Path to Better Movement Starts Here

At Triangle Physiotherapy Toronto, we take pride in guiding patients through each step of their healing journey with transparency, care, and expert support. If you’re ready to take control of your recovery, we’re here to walk with you – every step of the way.
Book your first appointment today and let’s build your path to pain-free living.
When you’re dealing with sudden pain or mobility issues – like a stiff neck, lower back spasm, or a sports injury – waiting days for care isn’t ideal. That’s why more people are searching for same-day physiotherapy booking options that are fast, accessible, and reliable.
At Triangle Physiotherapy Toronto, we understand that urgent physiotherapy needs can’t always wait. Our clinic offers same-day appointments for patients experiencing sudden discomfort, post-injury flare-ups, or worsening chronic pain. Here’s what you need to know about booking and receiving urgent physiotherapy care in Toronto.
What Counts as an Urgent Physiotherapy Need?
You don’t need to be in a medical emergency to require same-day care. If your pain or movement restriction is disrupting your daily activities – or you’ve had a recent injury – it’s worth seeking immediate help. Some common reasons people book same-day physiotherapy include:
- Sudden neck or back pain
- Sports injuries like ankle sprains or knee twists
- Post-surgical soreness or complications
- Sciatica flare-ups
- Muscle spasms or joint locking
- Work-related strain injuries
Even if you’re unsure how serious the issue is, early assessment can prevent the condition from worsening.
Same-Day Physiotherapy Toronto Booking: How It Works

At Triangle Physiotherapy Toronto, we do our best to offer same-day bookings for patients who need urgent care. Here’s how to increase your chances of securing a same-day spot:
- Call early in the day: Morning calls typically have the best availability
- Be flexible with time and location: We’ll help match you with the earliest possible opening, including other nearby Triangle clinics if needed
- Mention it’s urgent: Let our front desk team know the nature of the issue so they can prioritize accordingly
Our goal is to get you seen quickly, without compromising quality care.
What to Expect at Your First Visit
During your same-day visit, our physiotherapist will:
- Conduct a focused assessment to understand the cause of the problem
- Provide immediate relief techniques such as manual therapy, taping, or modalities
- Recommend follow-up treatment if needed
- Offer guidance on how to manage pain at home (stretches, ice/heat, etc.)
Even one session can make a big difference in calming inflammation, restoring movement, and preventing further injury.
Ongoing Support After Your Urgent Visit
While same-day treatment can offer relief, most conditions benefit from a short course of follow-up sessions. We’ll work with you to build a treatment plan that fits your schedule, goals, and lifestyle.
You’ll also receive education around injury prevention, ergonomic tips, and home exercises to help you heal and stay strong.
Why Triangle Physiotherapy Toronto?
We combine clinical excellence with responsive care. Whether you’re a first-time visitor or a returning client, our same-day physiotherapy Toronto booking system ensures timely access without the hassle. With flexible hours, experienced clinicians, and personalized treatment, we’re here to support your health whenever you need it most.
If you’ve never been to physiotherapy before, it’s completely normal to feel unsure about what to expect. Maybe you’re dealing with pain, recovering from an injury, or just looking for support to move better. No matter the reason, your first physiotherapy evaluation is a relaxed, informative session designed to understand your body and set the foundation for recovery.
Here’s what typically happens during your first visit.
1. A Conversation About You
It all starts with a conversation. Your physiotherapist will take the time to learn about your symptoms, medical history, activity level, and personal goals. This helps build a complete picture of what might be causing your discomfort and how it’s affecting your daily life.
It’s not just about the pain – it’s about how that pain fits into your overall well-being.
2. A Physical Assessment
Once you’ve talked through your history and concerns, your physiotherapist will perform a physical assessment. This usually includes:
- Observing posture and alignment
- Checking your range of motion and flexibility
- Testing muscle strength and joint mobility
- Identifying areas of pain, tension, or restriction
This hands-on evaluation helps pinpoint the source of your symptoms and understand how your body is moving – or compensating.
3. Understanding What’s Going On
After the assessment, your physiotherapist will explain what they’ve found in simple, easy-to-understand language. You’ll get insight into what’s likely causing your symptoms and how physiotherapy can help. This is also a great time to ask questions or express any concerns.
There’s no pressure – it’s about creating clarity and building trust.
4. A Personalized Treatment Plan
You’ll then be given a tailored treatment plan based on your specific needs and goals. It may include:
- Targeted exercises to improve strength, flexibility, or stability
- Hands-on manual therapy to release tension or restore movement
- Movement education to improve posture and body mechanics
- Home exercises or tips to support recovery between sessions
In many cases, treatment will begin during this first appointment so you can start feeling the benefits right away.
5. Next Steps and Ongoing Support
Your physiotherapist will walk you through what to expect moving forward – how often you may need to come in, how to measure progress, and what milestones to watch for. Every plan is customized and flexible, based on how your body responds. A lot of people come to us asking for prevention tips and we are here for them. With the increase in remote jobs, we are bound to face some stress – mental and physical. The best way to debug it, is to reach out to us and book a consultation. We are the catalyst you need for pain free everyday movement.

Final Thoughts
Your first physiotherapy evaluation is the beginning of a partnership focused on helping you move better, feel stronger, and get back to doing what you love. It’s not just about treating pain – it’s about understanding your body and building a plan that works for you.
So if you’re considering physiotherapy but feel unsure about what the first step looks like, know that it’s a calm, supportive experience designed entirely around your needs.
As we age, staying active and maintaining independence becomes more important than ever. However, many seniors face challenges with mobility, balance, and everyday tasks that were once simple to perform. Whether it’s walking, climbing stairs, or even standing up from a chair, these activities can become increasingly difficult without the right care. At Triangle Physiotherapy North York, we provide specialized physiotherapy services tailored to seniors to improve movement, restore balance, and promote an active lifestyle.
Why Physiotherapy is Essential for Seniors
Aging naturally brings changes to our bodies, including reduced joint flexibility, weaker muscles, and slower reflexes. These changes can lead to decreased mobility and an increased risk of falls. Physiotherapy for seniors focuses on restoring function, increasing strength, and enhancing stability, which are essential for preserving independence and overall well-being.
At Triangle Physiotherapy North York, we offer targeted treatments to help address these age-related changes. Our expert physiotherapists create personalized rehabilitation plans focused on improving posture, mobility, strength, and balance, while also emphasizing fall prevention. We aim to not only address existing conditions but also help prevent future complications, allowing our senior patients to live with greater confidence and freedom.
Why Triangle Physiotherapy North York is the Right Choice for Seniors

Selecting the right clinic for physiotherapy is critical, particularly for seniors who may have unique health concerns. Here’s what makes Triangle Physiotherapy North York stand out as the ideal choice for senior rehabilitation:
1. Customized Treatment Plans for Every Individual
Each senior has different health needs. Whether you’re dealing with osteoarthritis, recovering from surgery, or simply experiencing stiffness from aging, our physiotherapists take the time to understand your condition and create a rehabilitation plan that’s specifically tailored to you.
At Triangle Physiotherapy North York, we offer services ranging from mobility exercises and manual therapy to strength-building activities and postural training. Our aim is to help seniors regain independence and enjoy a better quality of life by providing care that’s specifically aligned with their goals.
2. Expertise in Senior Health and Recovery
Our physiotherapists are skilled in treating conditions commonly associated with aging. With years of experience in senior care, we understand the physical challenges that come with age and use proven methods to address them. Whether through joint mobilization, strength training, or balance improvement techniques, our focus is on helping you recover safely and effectively.
The Triangle team is dedicated to offering the most up-to-date treatments, all while ensuring your comfort and safety throughout your recovery.
3. A Compassionate and Welcoming Clinic Atmosphere
The right environment is crucial for effective recovery. At Triangle Physiotherapy North York, we’ve designed our clinic to be a warm and supportive space where seniors feel comfortable and at ease. From your initial consultation to your final treatment session, our staff is here to guide and support you every step of the way.
Our physiotherapists create a collaborative, encouraging environment that fosters trust and empowers seniors to take control of their rehabilitation journey.
Key Advantages of Senior Physiotherapy at Triangle Physiotherapy North York
- Improved Stability and Balance: We use balance training techniques to reduce the risk of falls, an essential part of maintaining independence for seniors.
- Enhanced Range of Motion: Through targeted stretching and strengthening exercises, we help restore flexibility and movement, enabling seniors to carry out daily activities with greater ease.
- Pain Management: Our physiotherapists specialize in alleviating discomfort caused by arthritis, muscle tension, and other age-related conditions, promoting pain relief and improved function.
Take the First Step Towards Better Mobility
At Triangle Physiotherapy North York, we believe that aging doesn’t have to mean sacrificing mobility or independence. With the right physiotherapy treatment, seniors can maintain an active and fulfilling life. Our experienced team is committed to improving your physical health and helping you stay independent. If you or someone you know is looking for dedicated, expert care, book a consultation with us today and take the first step toward a healthier, more mobile future.
Musculoskeletal pain – whether it’s from a recent injury, repetitive strain, or an ongoing condition – can quickly start to affect your everyday life. Simple tasks become challenging, and you may find yourself avoiding the activities you enjoy. So when’s the right time to take action and get help?
The Sooner, the Better
In most cases, the best time to start physiotherapy is sooner than you think. If you’ve been in pain for more than a few days and it’s not improving with rest or home remedies, it’s a good idea to see a physiotherapist. Early treatment helps prevent the issue from getting worse and speeds up your recovery.
At Triangle Physiotherapy in Mississauga, the team understands how important early intervention is. They offer expert care and a personalized approach to help you get back on track – whether you’re dealing with a sports injury, joint pain, or chronic stiffness.
Signs It’s Time to Start Physiotherapy

You don’t need to be in severe pain to benefit from physiotherapy. If you’re experiencing any of the following, it may be time to book an appointment:
- Pain that hasn’t gone away after a week or two
- Difficulty moving or using a joint properly
- Pain that comes and goes but keeps returning
- Recovery from surgery or a recent injury
- Long-term pain from conditions like arthritis or old injuries
Starting physiotherapy early at a trusted clinic like Triangle Physiotherapy Mississauga can make a big difference in both your short – and long-term recovery.
What to Expect at Triangle Physiotherapy
When you visit Triangle Physiotherapy, you’ll be welcomed by a team that takes the time to understand your concerns and goals. Your physiotherapist will assess your condition and create a tailored treatment plan that may include:
- Hands-on manual therapy
- Customized exercise programs including IMS
- Advanced approach to treatment
- Education to help prevent future injuries
They don’t just treat the symptoms – they help you understand what’s causing the pain and how to manage it.
Ready to Take the First Step?
If you’re looking to start physiotherapy in Mississauga, Triangle Physiotherapy is a great place to begin. Known for offering some of the best physiotherapy in Mississauga, their experienced team is committed to helping you feel and move better – without unnecessary delays or one-size-fits-all solutions.
Final Thoughts
You don’t have to live with ongoing pain or limited movement. The right physiotherapy support can make a huge difference – and the earlier you start, the better the outcome. If you’re ready to feel stronger, move better, and take back control of your health, visit Triangle Physiotherapy in Mississauga and get started today.
Acute pain can appear without warning – whether it’s a strained back, a swollen knee, or a sharp twinge in your shoulder. When that happens, timely care can make all the difference. Instead of waiting days for an appointment, accessing a same-day physiotherapy appointment in Mississauga allows you to begin managing your pain right away – with the guidance of a skilled professional.
Why Early Treatment Matters
Acute pain often signals inflammation, muscle strain, or joint irritation that, if left untreated, can escalate or lead to compensatory movement issues. While rest may seem like the best solution, early intervention by a physiotherapist can reduce discomfort and help restore movement effectively.
At Triangle Physiotherapy’s Mississauga clinic, same-day appointments are available so you don’t have to delay care. Their team understands that pain disrupts your day, and they’re here to help you address it with calm, expert support.
Benefits of Same-Day Physiotherapy
Booking a same-day physiotherapy appointment in Mississauga provides several important benefits:
- Timely relief from discomfort through hands-on therapy and individualized care
- Early diagnosis of the cause of pain, helping to prevent it from becoming a long-term issue
- A focused recovery plan tailored to your condition and lifestyle
- Guidance on safe movement to avoid further aggravation of the injury
Triangle Physiotherapy’s approach is centered around evidence-based treatment that’s adapted to your unique needs. Whether you’ve experienced a sudden injury or an unexpected flare-up of pain, their team is equipped to help you take the right steps forward – starting today.
Care When You Need It

Triangle Physiotherapy Mississauga makes it easier to access high-quality care without unnecessary delays. Their clinic is known for delivering exceptional physiotherapy in Mississauga, and their commitment to same-day availability reflects a patient-first philosophy.
From your first visit, you’ll experience care that is not only professional but also compassionate. The therapists at Triangle take time to understand the nature of your pain, work with you to establish realistic goals, and support your recovery every step of the way.
Take the First Step Toward Relief
If you’re dealing with acute discomfort, don’t wait and hope it passes on its own. Starting treatment at the right time – ideally right when symptoms begin—can lead to faster recovery and fewer complications. Booking a same-day physiotherapy appointment in Mississauga at Triangle Physiotherapy allows you to begin that process with confidence.
Final Thoughts
Acute pain can interrupt your life, but it doesn’t have to define it. At Triangle Physiotherapy Mississauga, you’ll find prompt, professional care designed to get you moving comfortably again. If you need support today, their team is ready to help you begin the journey back to feeling your best – with expert physiotherapy that starts when you need it most.
When you’re dealing with pain, injury, or chronic conditions like arthritis, choosing the right physiotherapist can make all the difference in your recovery. Physiotherapy is an essential part of managing pain, improving mobility, and enhancing your quality of life. However, with so many options out there, how do you know which physiotherapist is the best fit for your needs? At Triangle Physiotherapy in Toronto we have physiotherapists with varying specialties – from musculoskeletal to pelvic health to kid’s rehab.
In this blog, we’ll explore key factors to consider when selecting a physiotherapist.
1. Specialization Matters
Physiotherapy is a broad field, and different physiotherapists specialize in different areas. Whether you’re recovering from surgery, managing arthritis, or dealing with a sports injury, finding a physiotherapist who specializes in your specific condition can speed up your recovery and improve outcomes.
- For Arthritis and Joint Pain: Look for a physiotherapist with experience in managing musculoskeletal conditions like osteoarthritis or rheumatoid arthritis. They will be skilled in using therapeutic exercises, manual therapy, and pain management techniques to help reduce stiffness and improve mobility.
- For Sports Injuries: If you’re recovering from a sports-related injury, you might want a physiotherapist with experience in sports rehabilitation. They can tailor exercises that enhance strength and flexibility, preventing future injuries.

2. Physiotherapist Credentials and Experience
Check for credentials, such as a degree in physiotherapy (e.g., DPT or MSc in Physiotherapy) and any additional certifications related to your condition (e.g., orthopedic manual therapy or pelvic floor rehabilitation). More importantly, consider their experience: a physiotherapist with years of hands-on experience will likely be more adept at handling complex cases.
- Ask about their track record: How many patients have they treated with conditions like yours? Do they have experience working with people of your age group or fitness level?
3. Personalized Approach
Physiotherapy isn’t a one-size-fits-all treatment. It’s essential to find a physiotherapist who tailors treatment plans to your unique needs, rather than offering a generic approach. A skilled physiotherapist will conduct a thorough assessment of your physical condition, history, and goals before recommending treatment. This personalized approach ensures that you’re getting the care you need.
- Look for a physiotherapist who listens: A good physiotherapist will ask about your symptoms, lifestyle, and preferences to develop a treatment plan that works for you. They should be willing to adjust the plan if something isn’t helping or if new issues arise.
4. Approach to Communication
Effective communication is key to a successful physiotherapy experience. You’ll need to feel comfortable discussing your symptoms, goals, and progress with your physiotherapist. Clear communication helps ensure you understand your treatment plan and feel empowered to follow it.
- Ask about the treatment philosophy: Some physiotherapists emphasize hands-on techniques like manual therapy, while others focus on exercise-based rehabilitation. Ensure that the therapist’s methods align with your preferences and comfort levels.
- Check their availability: Some physiotherapists may be available for short, frequent sessions, while others may offer longer, less frequent appointments. Be sure that their schedule works with yours and that they are accessible for follow-up questions.
5. Physiotherapist Reputation and Reviews
One of the best ways to evaluate a physiotherapist is by asking for recommendations or reading online reviews. Hearing from others who have experienced similar conditions can give you insight into the therapist’s expertise and the quality of care they provide.
- Ask for recommendations: Your doctor, friends, or family members may have personal experiences to share. Word-of-mouth can often lead to finding a trusted physiotherapist.
- Online reviews: Patient reviews can provide valuable insights into a physiotherapist’s approach, professionalism, and success in treating various conditions.
6. Location and Accessibility
Convenience is important when committing to regular physiotherapy sessions. Look for a clinic that is easily accessible, whether it’s near your home or workplace. Consider the hours of operation and the availability of appointments that fit your schedule.
- Travel and parking: Make sure the location is convenient, and check whether there are parking facilities or easy access via public transport.
If you’re unsure of the type of physiotherapy you need, contact us at Triangle Physiotherapy. Our committed team is here to support you in reaching your health and wellness goals—whether you’re a seasoned athlete, a casual enthusiast, or embarking on your fitness journey for the first time.
Sprains vs. strains? Understanding the difference between sprains and strains is crucial for anyone engaged in physical activities or sports. Both are common injuries, but they affect different parts of the body and require distinct approaches for treatment and prevention. Here’s a comprehensive look at sprains and strains, including their causes, prevention strategies, and more.
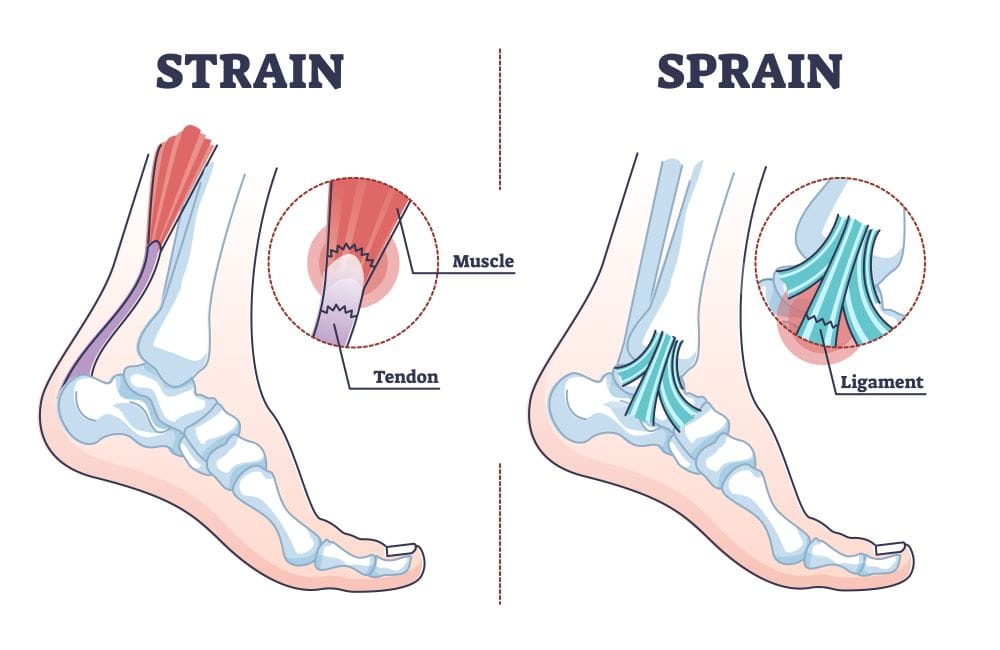
Picture Credit: Louisville Bones
Causes
Sprains occur when the ligaments, which are the tough bands of connective tissue that connect bones to each other, are stretched or torn. This usually happens due to a sudden twist or impact that forces a joint out of its normal range of motion. Common examples include rolling an ankle during a fall or twisting a knee while playing sports.
Strains, on the other hand, involve injuries to muscles or tendons, which connect muscles to bones. They are typically caused by overstretching or overusing a muscle, often due to sudden movements or lifting heavy objects improperly. Strains can happen during activities that require a lot of physical effort, such as running, lifting weights, or engaging in sports.
Prevention
Preventing sprains and strains starts with proper preparation and conditioning.
- For Sprains: Wearing appropriate footwear and using supportive gear during activities can help reduce the risk. Strengthening the muscles around the joints and improving balance through exercises can also be beneficial. Additionally, warming up properly before engaging in physical activities is crucial to prepare the ligaments for stress.
- For Strains: To prevent strains, it’s important to use proper techniques when lifting or performing strenuous activities. Regular strength training and flexibility exercises can help maintain muscle balance and reduce the risk of overstretching. Ensuring you are adequately warmed up before exercising can also protect against strains.
Progressive Resistance
Progressive resistance training involves gradually increasing the weight or resistance in exercises to build strength and endurance over time. This method is effective in preventing both sprains and strains by:
- For Sprains: Strengthening the muscles around the joints can provide better support and stability, reducing the likelihood of ligaments being stretched or torn.Practice ankle exercises using resistance bands
For Strains: Progressive resistance training helps in building muscle strength and resilience, which can prevent overstretching and muscle fatigue.Peform isolated movements that help with day to day resilience.
Neuromuscular Exercises
Neuromuscular exercises focus on improving the communication between the brain and muscles, enhancing coordination and stability. These exercises are particularly effective for:
- For Sprains: They help improve joint stability and balance, reducing the risk of accidents that might lead to sprains. Exercises such as balance training and proprioceptive drills can be beneficial. Use BOSU ball
- For Strains: Neuromuscular exercises enhance the control and responsiveness of muscles, reducing the chances of strains by improving movement patterns and muscle coordination. Allow it to rest, knowing when to rest is equally important.Drink plenty of water, and practice unilateral movements.Stretch the lower limbs.
Mobility Exercises
Mobility exercises aim to improve the range of motion and flexibility of joints and muscles. They are crucial for:
- For Sprains: Increasing joint mobility can help maintain a healthy range of motion, which can reduce the risk of injuries. Regular stretching and joint mobility exercises can keep ligaments and surrounding tissues flexible.
- For Strains: Enhancing muscle flexibility through mobility exercises can help prevent strains by allowing muscles to stretch properly without being overstretched. Incorporating dynamic stretches and functional movements can be beneficial. Go into deeper joint ROM.
Safety Tips
- Warm Up: Always start with a proper warm-up to prepare your muscles and ligaments for activity.
- Use Proper Techniques: Whether lifting weights or engaging in sports, ensure you use the correct techniques to avoid unnecessary strain.
- Listen to Your Body: Pay attention to any signs of discomfort or pain, and avoid pushing through it.
- Rest and Recover: Allow adequate time for rest and recovery to prevent overuse injuries.
If you suspect you have a sprain or a strain, give us a call or book an appointment to see one of our physiotherapists to get an assessment and treatment plan.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
As we age, maintaining mobility and independence becomes increasingly important for overall quality of life. For many elderly individuals, staying active and independent can be challenging due to various age-related factors. Physiotherapy emerges as a crucial tool in addressing these challenges, helping seniors preserve their physical function and improve their daily living. This blog explores the importance of physiotherapy for the elderly, highlighting causes of mobility issues, preventive measures, and effective exercises to support strength and mobility.
Our experienced practitioners at Triangle Physiotherapy can help you to stay active and prevent any mobility issues that may arise with age.
Call us today to learn more about how we can help you start moving better.
Causes
Several factors contribute to decreased mobility in elderly individuals. Common causes include:
- Muscle Weakness: Aging often leads to muscle loss, making it harder to perform everyday activities.
- Joint Stiffness: Reduced flexibility and joint pain can limit movement.
- Balance Problems: Deteriorating balance increases the risk of falls, which can lead to serious injuries.
- Chronic Conditions: Diseases such as arthritis, osteoporosis, and cardiovascular issues can impact physical ability.
Understanding these causes helps in designing targeted physiotherapy interventions to address specific challenges and improve overall function.
Prevention

Preventive measures play a vital role in maintaining mobility and independence as we age. Regular physical activity, a balanced diet, and routine medical check-ups can help mitigate some of the issues that arise with aging. Your Physiotherapist will help you incorporate the following into daily routines can be beneficial:
- Regular Exercise: Engaging in physical activities such as walking, swimming, or biking helps maintain muscle strength and joint flexibility.
- Healthy Diet: A diet rich in calcium and vitamin D supports bone health, while protein helps in muscle maintenance.
- Routine Check-ups: Regular visits to healthcare professionals can help manage chronic conditions and prevent complications.
Importance of Physiotherapy
Physiotherapy is essential for elderly individuals to address and manage mobility issues. It offers several benefits:
- Personalized Care: Physiotherapists design customized exercise programs based on individual needs and limitations.
- Pain Management: Through techniques like manual therapy and modalities such as heat or cold therapy, physiotherapy can help alleviate pain.
- Fall Prevention: Physiotherapy can enhance balance and coordination, reducing the risk of falls and related injuries.
- Enhanced Quality of Life: Improved mobility and independence contribute to a better overall quality of life and increased participation in social activities.
Strengthening and Mobility Exercises
Strengthening and mobility exercises are fundamental components of physiotherapy for seniors. These exercises help maintain and improve physical function:
- Strengthening Exercises: Focus on major muscle groups to enhance overall strength. Examples include seated leg lifts, wall push-ups, and resistance band exercises.
- Mobility Exercises: Improve joint flexibility and range of motion. Simple activities such as ankle circles, shoulder rolls, and gentle stretching can be beneficial.
- Additionally, the GLA:D Program for Knee and Hip Arthritis can be very beneficial because it provides education and targeted exercise that can be applied to movement in everyday activities.
Regular practice of these exercises helps prevent muscle atrophy and joint stiffness, promoting better movement and function.
Neuromuscular Exercises
Neuromuscular exercises target coordination, balance, and proprioception (the sense of body position). These exercises are crucial for fall prevention and overall stability:
- Balance Training: Activities such as standing on one leg, heel-to-toe walking, and balance board exercises enhance stability.
- Coordination Drills: Exercises like toe taps, marching in place, and dynamic movements help improve coordination and reaction times.
- Proprioceptive Exercises: Incorporate activities that challenge the senses and improve body awareness, such as using a wobble cushion or performing slow, controlled movements.
Safety Tips
Safety is paramount when performing exercises, especially for seniors. Consider these tips to ensure a safe and effective physiotherapy routine:
- Consult a Professional: Always seek guidance from a qualified physiotherapist before starting any new exercise program.
- Start Slowly: Begin with low-intensity exercises and gradually increase intensity to avoid overexertion.
- Use Proper Equipment: Ensure that any exercise equipment is appropriate and in good condition to prevent accidents.
- Listen to Your Body: Pay attention to any discomfort or pain and stop the activity if necessary.
Call us today to learn more and get started!











