Athletes push their bodies hard – every sprint, every rep, every game. But sometimes, the most challenging injuries are the ones you don’t see coming. Hairline fractures – also called stress fractures – can creep in quietly and sideline even the most elite performers.
If you’re searching for sports physiotherapy near me after a stress injury, or want to prevent future setbacks, this guide is for you.
At Triangle Physiotherapy, we understand the athlete’s mindset – and we’re here to get you back in the game, stronger than before.
What Is a Hairline Fracture?
Hairline fractures are tiny cracks in the bone, often caused by repetitive stress rather than a single traumatic event. They commonly affect:
- Runners (shins, feet)
- Basketball or soccer players (lower legs, hips)
- Gymnasts or dancers (feet, spine)
Unlike acute injuries, stress fractures develop over time – especially when there’s overtraining, poor biomechanics, or inadequate recovery.
Common Signs of a Stress Fracture in Athletes
- Localized pain that worsens with activity
- Pain that subsides with rest but returns with exertion
- Swelling or tenderness at a specific site
- In some cases, minor bruising
If you’re brushing off a nagging pain thinking it’s “just soreness,” stop. Early intervention is key.
The Role of Physiotherapy in Hairline Fracture Recovery

At Triangle Physiotherapy, our sports rehab specialists build a plan that supports bone healing, protects your performance, and prevents re-injury.
Here’s how we approach it:
1. Acute Phase: Protect + Heal
2. Rehabilitation Phase: Rebuild + Strengthen
3.Return-to-Sport Phase: Retrain + Prevent
Education on training volume, rest cycles, and warning signs
We believe in graduated return-to-play protocols, so you don’t bounce back too fast—and end up right back on the bench.
How to Prevent Hairline Fractures in Sports
Prevention isn’t about holding back – it’s about training smarter. Here’s how:
● Avoid sudden spikes in training volume/intensity
● Cross-train to reduce repetitive stress
● Warm up properly and stretch regularly
● Fuel your body with a balanced diet
● Get regular check-ins with a sports physiotherapist in Toronto (hi, that’s us!)
Ready to Get Back in the Game?
Being sidelined can be frustrating – but it’s also an opportunity. With the right guidance, your comeback can be stronger than your setback.
Whether you’re a weekend warrior or a competitive athlete, our team at Triangle Physiotherapy offers expert physiotherapy for hairline fractures and stress injury rehab that puts your long-term health first.
Serving athletes across the GTA | ⚕️Triangle Physiotherapy Toronto 📞 Book an appointment with the best physiotherapist in Toronto today and let’s rebuild your game – one smart step at a time. 💪
If you’re an athlete, fitness enthusiast, or just someone who enjoys staying active, you know how frustrating sports injuries can be. Whether it’s a sprained ankle from a quick pivot, shoulder pain from weightlifting, or chronic knee strain from running, these injuries don’t just affect your physical performance – they impact your daily life. At Triangle Physiotherapy North York, our mission is to help you recover faster, move better, and prevent future injuries through personalized, expert care.
Why Physiotherapy Is Crucial in Sports Injury Recovery
Physiotherapy plays a vital role in every stage of sports injury rehab – from initial pain relief to long-term performance enhancement. At Triangle Physiotherapy North York, we take a full-body, functional approach to healing. Our experienced team doesn’t just treat your symptoms – we identify the root cause of the injury and build a custom rehab plan around your goals.
We combine advanced techniques like manual therapy, therapeutic exercise, soft tissue release, and even dry needling, all designed to get you back to doing what you love – whether that’s playing a sport, hitting the gym, or enjoying a pain-free walk.
Choosing the Right Sports Rehab Clinic: Why Triangle Stands Out

Much like choosing a clinic for back pain relief, selecting the right physiotherapy clinic for sports injuries is crucial to your recovery. Here’s how Triangle Physiotherapy North York makes the process easy and effective:
1. We Understand Your Unique Needs
No two injuries – or patients – are alike. Are you recovering from a torn ligament, muscle strain, or joint overuse? Are you prepping for a marathon or trying to get through your workday pain-free?
At Triangle, we take the time to understand your activity level, movement goals, and pain points. Our North York clinic offers everything from sports injury rehab and mobility training to preventative care and performance optimization – all tailored to your needs.
2. Experience and Evidence-Based Care
With a strong team of skilled and licensed physiotherapists, we deliver care that’s grounded in science and focused on results. Our treatment plans often include strength training, mobility work, posture correction, and ergonomic education – designed not only for short-term relief but long-term success.
Whether you’re recovering from a recent injury or managing chronic pain from overuse, our team in North York is ready to help you rebuild and return stronger.
3. A Supportive Environment That Motivates You
Healing doesn’t happen in a vacuum. That’s why the environment at Triangle Physiotherapy North York is designed to be welcoming, calm, and encouraging. From the front desk to your treatment sessions, our team ensures you feel heard, supported, and empowered throughout your recovery journey.
Ready to Get Back in the Game?
At Triangle Physiotherapy North York, we believe that recovery isn’t just about healing – it’s about thriving. Whether you’re aiming to return to sport, improve your performance, or simply move without pain, our personalized physiotherapy services are here to help.
Book your consultation today and take the first step toward a stronger, healthier, and more confident you.
For athletes, whether they’re professional competitors or weekend warriors, massage therapy isn’t just a luxury—it’s a crucial part of their training and recovery routine. While the soothing effects of a massage might seem like a simple indulgence, its benefits extend far beyond relaxation.

Here are five compelling reasons why athletes should incorporate massage therapy into their regimen:
1. Enhanced Recovery and Reduced Muscle Soreness
After an intense workout or a grueling competition, muscles can feel sore and fatigued. This is where massage therapy shines. By increasing blood flow and enhancing circulation, massage helps to deliver essential nutrients and oxygen to tired muscles, facilitating quicker recovery. Additionally, it helps to flush out metabolic waste products like lactic acid, which can accumulate and contribute to soreness. Regular massages can reduce muscle stiffness and speed up the recovery process, allowing athletes to get back to training faster and more efficiently.
2. Injury Prevention and Improved Flexibility
Injuries are an unfortunate part of an athlete’s life, but many can be prevented with proper care. Massage therapy plays a critical role in maintaining flexibility and preventing injuries. By working on tight or imbalanced muscles, massage helps to release tension and improve range of motion. This not only reduces the risk of strains and sprains but also helps athletes maintain proper biomechanics, which is essential for both performance and injury prevention.
3. Improved Performance and Reduced Muscle Tension
Massage therapy is not just about recovery; it also contributes to enhanced performance. By addressing muscle tension and promoting relaxation, massage can improve an athlete’s overall sense of well-being and focus. This relaxation helps in reducing the mental and physical stress that can negatively impact performance. Furthermore, a well-tuned muscle system can lead to better coordination, agility, and strength, giving athletes a competitive edge.
4. Stress Relief and Enhanced Mental Clarity
The pressures of training, competition, and performance expectations can take a toll on an athlete’s mental health. Massage therapy provides an opportunity for relaxation and stress relief. The act of being touched and the calming environment of a massage session can reduce levels of the stress hormone cortisol while boosting the release of endorphins, which are natural mood lifters. This not only helps athletes manage stress more effectively but also contributes to better mental clarity and focus, which are essential for peak performance.
5. Better Sleep Quality
Quality sleep is vital for recovery, performance, and overall health. However, athletes often struggle with sleep issues due to the physical demands of their training and competitions. Massage therapy can improve sleep quality by promoting relaxation and reducing physical discomfort that might interfere with rest. Enhanced relaxation and reduced muscle tension can lead to deeper, more restorative sleep, which is crucial for muscle repair, cognitive function, and overall well-being.
Incorporating Massage Therapy into Your Routine
To reap the maximum benefits of massage therapy, it’s important for athletes to incorporate it into their regular training regimen. Working with a skilled therapist who understands the specific needs of athletes can make a significant difference. Whether it’s a post-workout recovery session, a pre-competition tune-up, or a routine maintenance massage, finding the right type of massage and frequency that works best for your body can help you achieve optimal performance and maintain overall health.
In conclusion, massage therapy offers a wealth of benefits for athletes, from speeding up recovery and preventing injuries to enhancing performance and improving mental clarity. By integrating massage into their training and recovery routines, athletes can better support their physical and mental well-being, paving the way for sustained success and peak performance.
Massage Therapy Mississauga
We have 2 locations with massage therapists in Mississauga to help you.
Massage therapy involves the manipulation of the body’s soft tissues, including muscles, connective tissues, tendons, ligaments, and skin, to improve a person’s health and well-being. This practice has been used for thousands of years across various cultures and is widely recognized for its numerous benefits.

What is Deep Tissue Massage?
Deep tissue massage is a type of massage therapy that focuses on the deeper layers of muscle and connective tissue. It is especially beneficial for individuals who suffer from chronic pain, muscle tension, or are recovering from an injury. This technique involves the use of slow, deliberate strokes and deep pressure to target specific areas of tension and tightness.
What is Swedish Massage?
Swedish massage is a popular and widely practiced form of massage therapy known for its gentle and relaxing techniques. It focuses on promoting overall relaxation, improving blood flow, and relieving muscle tension. Swedish massage is an excellent choice for those new to massage therapy or looking for a general wellness treatment.
What is the difference between Deep Tissue Massage and Swedish Massage?
Swedish Massage:
- Relaxation: Promotes overall relaxation and reduces stress.
- Circulation: Enhances blood flow and oxygen delivery.
- Muscle Relief: Eases muscle tension and soreness.
- Flexibility: Improves range of motion and flexibility.
- General Wellness: Suitable for maintaining overall health and well-being.
Deep Tissue Massage:
- Pain Relief: Addresses chronic pain and conditions such as lower back pain and neck pain.
- Muscle Tension: Releases deeper layers of muscle tension and knots.
- Injury Recovery: Aids in rehabilitation from injuries by promoting healing and reducing scar tissue.
- Posture Improvement: Corrects muscle imbalances and postural issues.
- Specific Problem Areas: Focuses on targeted areas rather than the whole body.
What are some other types of Massage therapy?
1. Sports Massage
- Focus: Enhances athletic performance and recovery.
- Techniques: Combines Swedish massage, deep tissue, and stretching techniques.
- Benefits: Reduces muscle soreness, improves flexibility, and prevents injuries.
- Ideal For: Athletes and active individuals.
2. Trigger Point Therapy
- Focus: Relieves pain by targeting specific trigger points.
- Techniques: Applies direct pressure to trigger points (knots in the muscles).
- Benefits: Reduces localized pain and referred pain in other areas.
- Ideal For: People with chronic pain and tension.
3. Shiatsu
- Focus: Balances the body’s energy flow.
- Techniques: Uses finger pressure on specific points along the body’s meridians.
- Benefits: Promotes relaxation, reduces stress, and improves energy flow.
- Ideal For: Individuals seeking holistic health benefits and stress relief.
4. Reflexology
- Focus: Stimulates reflex points on the feet, hands, or ears.
- Techniques: Applies pressure to specific points believed to correspond to other body parts.
- Benefits: Enhances overall health and well-being, relieves stress, and improves circulation.
- Ideal For: People looking for non-invasive therapy and overall wellness.
5. Prenatal Massage
- Focus: Supports the health and well-being of pregnant women.
- Techniques: Gentle techniques to relieve pregnancy-related discomfort.
- Benefits: Reduces back pain, improves sleep, and decreases stress and anxiety.
- Ideal For: Pregnant women experiencing discomfort and seeking relaxation.
6. Hot Stone Massage
- Focus: Deep relaxation and muscle tension relief.
- Techniques: Uses heated stones placed on the body and integrated into massage strokes.
- Benefits: Enhances relaxation, improves circulation, and alleviates muscle stiffness.
- Ideal For: Individuals looking for a deeply relaxing experience.
7. Thai Massage
- Focus: Combines acupressure, stretching, and assisted yoga postures.
- Techniques: Performed on a mat, involves rhythmic pressure and stretching.
- Benefits: Increases flexibility, relieves muscle tension, and boosts energy levels.
- Ideal For: People seeking an active and invigorating massage experience.
8. Lymphatic Drainage Massage
- Focus: Stimulates the lymphatic system to remove toxins and waste.
- Techniques: Gentle, rhythmic strokes and light pressure.
- Benefits: Reduces swelling, improves immune function, and detoxifies the body.
- Ideal For: Individuals with lymphedema, post-surgery recovery, or those wanting detoxification.
9. Craniosacral Therapy
- Focus: Works on the craniosacral system to relieve tension.
- Techniques: Gentle touch to manipulate the skull and sacrum.
- Benefits: Reduces stress, alleviates pain, and improves nervous system function.
- Ideal For: People with chronic pain, headaches, or stress-related conditions.
10. Aromatherapy Massage
- Focus: Enhances the massage experience using essential oils.
- Techniques: Combines Swedish or other massage techniques with aromatherapy.
- Benefits: Promotes relaxation, reduces stress, and improves mood.
- Ideal For: Individuals seeking relaxation and mood enhancement.
Click here to book an appointment with a massage therapist at one of our eight locations.
- Massage therapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Massage Therapy Clinic – Triangle Physiotherapy Oakville
- Massage Therapy North York – Triangle Physiotherapy North York
- Mississauga Massage Therapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Massage Therapy Clinics – Triangle Physiotherapy King West
- Uptown Massage Therapy Clinics – Triangle Physiotherapy Lawrence Park
- Massage Therapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- RMT Mississauga – Triangle Physiotherapy Erin Mills
Whether you choose deep tissue or Swedish massage, both can offer significant benefits for relaxation and pain relief. If you’re looking for expert advice on which massage therapy is best for you, consider visiting a physiotherapy clinic in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Professional physiotherapists and massage therapists in these areas can provide the right treatment to help you achieve your wellness goals.
Golf is known for its emphasis on skill, strategy, and etiquette, and it is enjoyed by millions of people worldwide. Apart from the swing, optimal golf performance involves perfect coordination between physical fitness, technique, and mental focus. Physiotherapy is increasingly used by golfers to enhance their game, to optimize golf performance.
What are the key physical attributes essential to a good golf game?
- Core Strength and Stability for Swing Power
- Spine and Cervical Rotation for Swing Rotation
- Wrist and Forearm Mobility for Control
- Lower Body Mobility for Distance
- Pelvic Tilt for Power and Control
- Single Leg Balance for Stability
What are the most common golf injuries?
The most common Golf injuries are:
Tendinitis:
Tendinitis is caused by overuse or repetitive movements, especially during activities such as sports, gardening, or typing, notably in elbows (tennis elbow and golfer’s elbow) and wrists. The symptoms are: aching, tenderness, and swelling around the affected joint during and after play.
How to prevent tendinitis:
- Warm-up and cool-down: stretch before and after each round.
- Proper form: Ensure that you use proper technique and form. Improper technique can put excessive stress on tendons and increase the risk of tendinitis.
- Listen to your body: Pay attention to any signs of discomfort or pain during physical activity. If you experience persistent pain or discomfort in a tendon, stop the activity and rest. Continuing to push through pain can exacerbate the injury and lead to more severe problems.
Shoulder Injuries:
Shoulder injuries related to golfing are relatively common, particularly among avid golfers or those who engage in the sport frequently without proper technique or conditioning. The golf swing involves complex movements that can place stress on various parts of the body, including the shoulders.
How to prevent shoulder injuries:
- Warm-up: perform a thorough warm-up routine that includes dynamic stretches and exercises to prepare your muscles and joints for the golf swing.
- Maintain good posture: PWork with a golf instructor to ensure that your golf swing technique is sound and biomechanically efficient. Proper swing mechanics can help reduce stress on the shoulders and decrease the risk of injury. Pay attention to your posture, grip, and rotation throughout the swing.
- Gradual progression: Pace yourself during your round of golf and avoid swinging too forcefully, especially if you’re fatigued.
Back Pain:
The repetitive motion of the golf swing, combined with the rotational forces generated by the movement, can place stress on the muscles, ligaments, and joints of the back, leading to discomfort or injury. The symptoms are: Aching, stiffness, or sharp pain in the lower back, sometimes radiating down the legs.
How to prevent back injuries:
- Core strengthening exercises
- Posture: Avoid excessive rounding or arching during swings.
- Proper lifting techniques: Avoid bending from the back during activities.
Knee Problems:
Knee problems are caused by pivoting motions and uneven terrain stress knees, causing tendonitis, patellar instability, and arthritis. The symptoms are:
- Symptoms: Knee pain, swelling, and stiffness, especially during weight-bearing activities.
How to prevent knee problems:
- Strengthening exercises: Target hamstrings, quads, and calves for knee stability.
- Proper footwear: Select supportive shoes with good traction for uneven surfaces.
- Warm-up and cool down: Prepare knee joints before play and stretch after the game.
How do I prevent golf injuries?
Seeing a physiotherapist before golfing season is highly recommended. Your physiotherapist will help you with:
- Strengthening: Strengthen core, shoulder, and leg muscles with planks, lunges, and rotator cuff exercises. A strong foundation makes your body resilient to swing demands.
- Flexibility: Maintain spine, hip, and shoulder range of motion for a smoother swing. Incorporate gentle stretches and yoga poses to reduce muscle strains.
- Balance and Proprioception: Improve balance and body awareness with single-leg stances and wobble board exercises. Prevent awkward falls on the course.
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Improving your golf game this spring can greatly benefit from the right physical conditioning and expert guidance. For personalized support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas can help you enhance your strength, flexibility, and overall performance on the golf course.
Biking injuries can occur due to various reasons, including accidents, overuse, improper bike setup, or poor riding technique. It’s important to address injuries promptly and seek professional medical advice if needed.

Here are common biking injuries and general tips on how to manage them:
- Sprains and Strains:
- Management: Rest, ice, compression, and elevation (R.I.C.E.) can help alleviate pain and swelling.
- Prevention: Warm up before riding, stretch regularly, and ensure proper bike fit.
- Road Rash:
- Management: Clean the wound thoroughly, apply an antiseptic ointment, and keep it covered with a sterile dressing.
- Prevention: Wear appropriate protective gear, including gloves, long-sleeved shirts, and pants.
- Fractures:
- Management: Seek immediate medical attention. Immobilize the affected area and avoid putting weight on it.
- Prevention: Wear protective gear, including a helmet, and follow proper safety guidelines.
- Cuts and Abrasions:
- Management: Clean the wound with mild soap and water, apply an antiseptic, and cover with a sterile dressing.
- Prevention: Wear protective clothing, such as long sleeves and pants, and use gloves.
- Overuse Injuries:
- Management: Rest, ice, and anti-inflammatory medications can help. Physical therapy may be beneficial.
- Prevention: Gradually increase your riding intensity and distance, cross-train to strengthen supporting muscles, and maintain a proper bike fit.
- Neck and Back Pain:
- Management: Rest, gentle stretching, and over-the-counter pain medications can provide relief. If persistent, consult a healthcare professional.
- Prevention: Ensure proper bike fit, maintain good posture while riding, and incorporate core-strengthening exercises.
- Nerve Compression (Cyclist’s Palsy):
- Management: Rest, anti-inflammatory medications, and adjusting bike setup. Consult a healthcare professional if symptoms persist.
- Prevention: Change hand positions regularly while riding, wear padded gloves, and maintain a proper bike fit.
- Dehydration and Heat-Related Issues:
- Management: Rehydrate, rest in a cool place, and use electrolyte solutions. Seek medical attention for severe cases.
- Prevention: Stay well-hydrated, wear appropriate clothing, and avoid riding in extreme heat.
Always remember to consult with a healthcare professional for accurate diagnosis and treatment. If in doubt about the severity of an injury, seek medical attention promptly. Additionally, consider taking preventive measures to minimize the risk of injuries during biking activities.
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Biking injuries can be challenging, but with the right management and physiotherapy, you can get back on track. Triangle Physiotherapy offers specialized care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our expert team is here to help you recover from biking injuries and improve your performance.”
What is the ACL?
The ACL, or Anterior Cruciate Ligament, is one of the four major ligaments in the knee joint. It is located in the center of the knee and runs diagonally, connecting the femur (thigh bone) to the tibia (shin bone). Its primary function is to prevent excessive forward movement of the tibia relative to the femur and control rotational movements of the knee.
What is an ACL Injury?
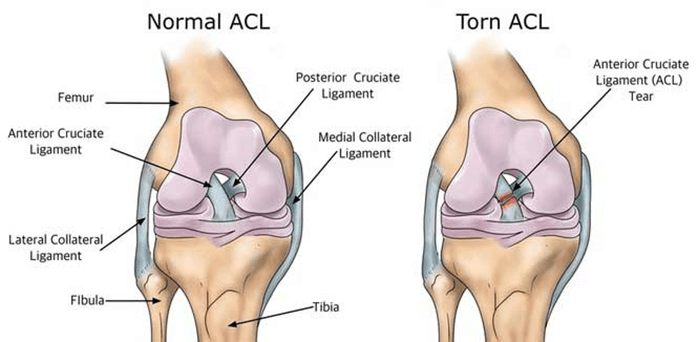
Injuries to the ACL are relatively common, often occurring during sports activities that involve sudden stops, changes in direction, or direct impact on the knee. ACL injuries can range from mild sprains to complete tears. When the ACL is torn, it can lead to instability in the knee, difficulty with weight-bearing, and a decreased ability to perform certain activities.
Consulting with a physiotherapist at Physiotherapy Oakville is crucial for recovery, as scientific research has shown that structured physiotherapy programs significantly improve outcomes for ACL injuries. These programs focus on strengthening the muscles around the knee, improving flexibility, and restoring stability. By joining Physiotherapy Oakville, you can benefit from evidence-based treatments and personalized exercise plans that enhance your recovery process, reduce the risk of further injury, and help you return to your normal activities with confidence.
What are the symptoms of an ACL injury?
Common symptoms of an ACL injury include:
- Pain: Individuals with an ACL injury often experience pain in the knee. The intensity of the pain can vary based on the severity of the injury.
- Swelling: Swelling typically occurs within a few hours of the injury and may be accompanied by a feeling of tightness or fullness in the knee.
- Instability: A sense of instability or a feeling that the knee is “giving way” is a common symptom. This instability may be particularly noticeable during activities that involve cutting, pivoting, or sudden changes in direction.
- Loss of Range of Motion: The injured knee may have a reduced range of motion, and it may be challenging to fully straighten or bend the knee.
- Audible “Pop” Sound: Some people report hearing or feeling a “pop” at the time of the injury. However, not everyone experiences this sensation.
- Difficulty Weight-bearing: Walking or putting weight on the affected leg may be difficult, especially immediately after the injury.
Can Physiotherapy help with an ACL Injury?
Yes, physiotherapy is a crucial component of the rehabilitation process for individuals with an ACL (Anterior Cruciate Ligament) injury, particularly those who undergo surgical intervention such as ACL reconstruction. Physiotherapy aims to address pain, swelling, muscle weakness, and joint instability while helping individuals regain normal function and return to their usual activities.
Here are some ways in which physiotherapy can help with an ACL injury:
- Post-operative Rehabilitation: After ACL reconstruction surgery, physiotherapy plays a vital role in the postoperative rehabilitation process. The early phases focus on managing pain and swelling, restoring range of motion, and preventing muscle atrophy.
- Strengthening Exercises: Physiotherapists prescribe specific exercises to strengthen the muscles around the knee, including the quadriceps, hamstrings, and calf muscles. Strengthening these muscles helps provide stability to the knee joint.
- Balance and Proprioception Training: ACL injuries can affect balance and proprioception (awareness of joint position). Physiotherapy incorporates exercises to improve balance and proprioception, reducing the risk of future injuries and enhancing overall joint stability.
- Range of Motion Exercises: Physiotherapists guide patients through a series of exercises to regain and maintain a normal range of motion in the knee. This is important for preventing stiffness and improving functional mobility.
- Functional Training: As the rehabilitation progresses, physiotherapy includes functional activities and sport-specific exercises to help individuals return to their normal activities or sports safely.
- Education and Home Exercise Programs: Physiotherapists educate patients about their condition, recovery process, and strategies for preventing future injuries. They often provide home exercise programs to continue rehabilitation between sessions.
- Gradual Return to Sports: For individuals aiming to return to sports or high-demand activities, physiotherapy guides a gradual progression of exercises to ensure a safe and effective return, taking into account factors like strength, agility, and neuromuscular control.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Starting physiotherapy at the right time after ACL surgery is crucial for optimal recovery. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can guide you through a personalized rehabilitation program to help you regain strength and mobility efficiently.”







