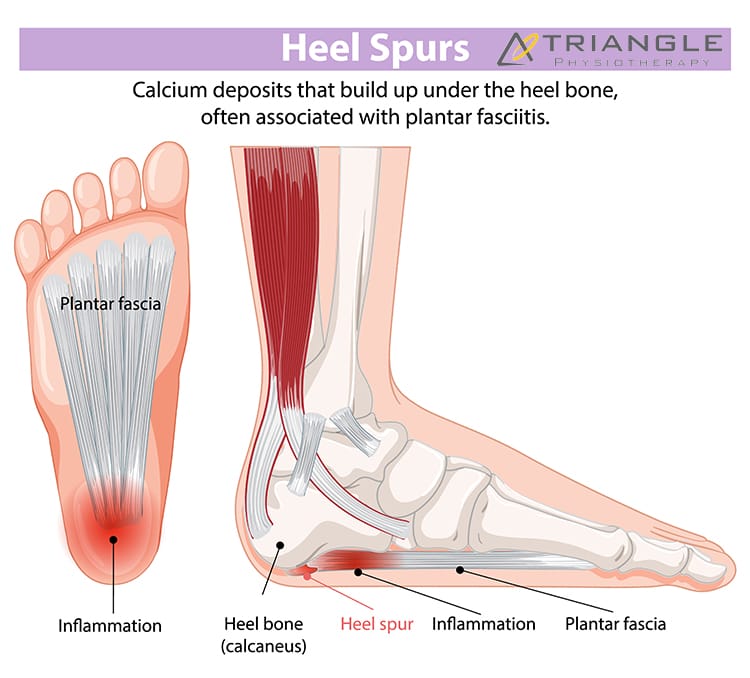
A heel spur is a bony protrusion that forms where the plantar fascia (a thick band of tissue running along the bottom of the foot) attaches to the heel bone. Heel spurs develop gradually over time due to repeated stress on the foot, which causes calcium deposits to accumulate in the affected area. Although many people with heel spurs don’t experience pain, others may feel sharp or aching pain, particularly when standing or walking.

If you have a heel spur, our physiotherapists at Triangle Physiotherapy can help!
What Causes Heel Spurs?
The primary cause of heel spurs is chronic strain and stress on the plantar fascia. Several factors can contribute to this, including:
- Overuse or excessive pressure on the foot: High-impact activities like running, jumping, or prolonged standing can increase the strain on the heel.
- Poor footwear: Wearing shoes that lack proper arch support or cushioning can put added stress on the heel and plantar fascia.
- Obesity: Carrying excess weight can strain the feet, leading to inflammation and potential heel spur formation.
- Flat feet or high arches: Both conditions can alter the mechanics of the foot and contribute to heel pain and spur development.
- Age: As we age, the fat pad that cushions the heel tends to thin, increasing pressure on the heel bone.
Common Symptoms of Heel Spurs
Heel spurs don’t always cause pain, but when they do, the symptoms can include:
- Sharp, stabbing pain: Most often felt in the morning with the first few steps, as the foot moves after resting overnight.
- A dull ache: This pain can persist throughout the day, especially after prolonged standing or walking.
- Tenderness: The bottom of the heel may feel tender to the touch, especially around the spur’s location.
- Swelling and inflammation: In some cases, the area around the spur may become swollen and inflamed.
Treatment for Heel Spurs
Thankfully, there are several treatment options available to alleviate the pain associated with heel spurs and help with recovery.
- Rest and Ice: Giving your foot time to rest and applying ice to the affected area can help reduce inflammation and relieve pain.
- Stretching Exercises: Stretching the calf muscles, Achilles tendon, and plantar fascia can help relieve tension and reduce heel pain. A physical therapist can recommend specific stretches.
- Shockwave Therapy: ESWT is a non-invasive treatment option for heel spurs, where high-energy sound waves are directed at the affected area to stimulate healing and alleviate pain associated with the heel spur.
- Orthotic Inserts: Custom or over-the-counter arch supports can help redistribute pressure on the foot and reduce strain on the heel.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen, can help reduce pain and swelling.
- Corticosteroid Injections: For more persistent pain, a doctor may recommend an injection to reduce inflammation and relieve discomfort.
- Surgery: In rare cases, when conservative treatments do not provide relief, surgery may be necessary to remove the spur or release tension on the plantar fascia.

Preventing Heel Spurs
Preventing heel spurs involves addressing the underlying causes. To avoid developing heel spurs:
- Wear supportive shoes with cushioning.
- Avoid overuse or excessive pressure on the feet.
- Maintain a healthy weight to reduce stress on the feet.
- Stretch before and after physical activity.
Conclusion
Heel spurs can be a painful and frustrating condition, but with the right treatment and preventive measures, most people can find relief and return to their normal activities. If you’re experiencing heel pain, it’s important to consult with a healthcare provider to determine the cause and develop an appropriate treatment plan. With the right care, heel spurs can be managed effectively, allowing you to walk and move comfortably again. Connect with us at Triangle Physiotherapy and we can get you started on your road to recovery from heel spurs!
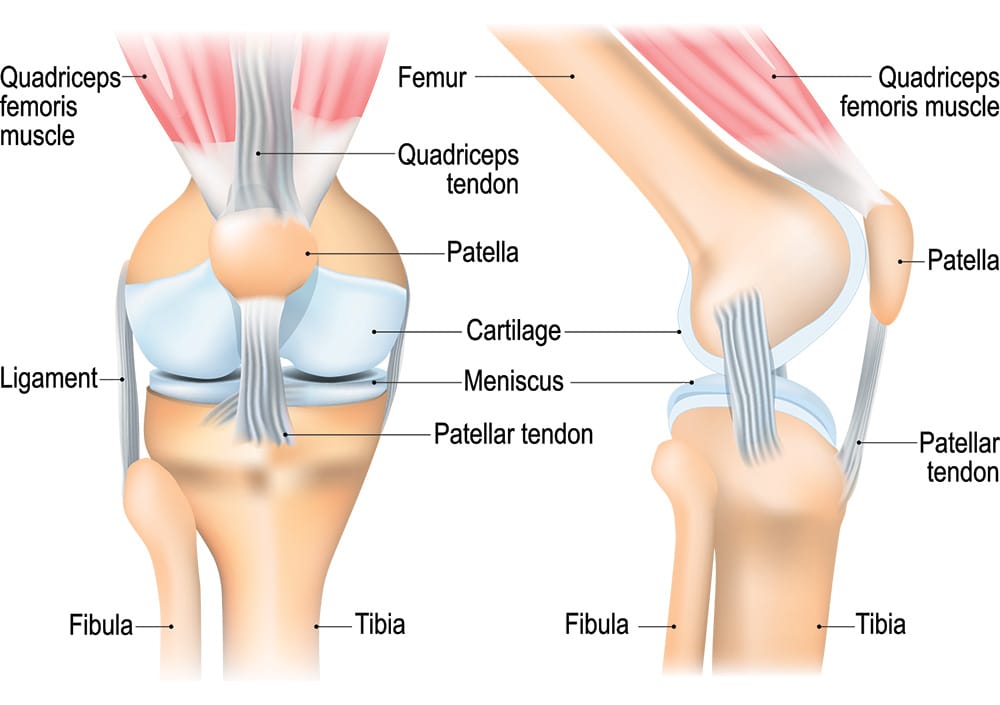
Knee pain can significantly impact your daily activities and overall quality of life. Whether it’s due to an injury, arthritis, or overuse, finding effective relief is essential. Physiotherapy is a valuable tool in managing knee pain, providing strategies to alleviate discomfort and improve function. Whether your knee pain is from a fall, a sports injury, arthritis or everyday aches and pains, our physiotherapists at Triangle Physiotherapy are here to help you navigate your recovery.
Understanding Knee Pain
Knee pain can arise from various conditions, including ligament injuries, tendonitis, bursitis, post-surgery or osteoarthritis. The pain may manifest as sharp, dull, or throbbing sensations, making it challenging to perform everyday tasks. Understanding the underlying cause is crucial for effective treatment. Physiotherapy takes a comprehensive approach to address not only the symptoms but also the root cause of the pain.
The Role of Physiotherapy
Physiotherapy offers a structured treatment plan tailored to your specific needs. A physiotherapist will conduct a thorough assessment, reviewing your medical history and evaluating your knee’s function. Based on this assessment, they will develop an individualized treatment plan focused on relieving pain, restoring mobility, and strengthening the muscles around the knee.
Pain Management Techniques for Knee Pain
Physiotherapists employ various techniques to manage knee pain effectively. These can include:
- Manual Therapy: Hands-on techniques to mobilize the knee joint and surrounding tissues, reducing stiffness and improving range of motion.
- IMS: Intra muscular Stimulation is an effective tool to trace and treat the root cause, reducing recurrence.
- Modalities: Methods such as ultrasound, heat, or cold therapy can help alleviate pain and inflammation. Read about PEACE and LOVE protocol instead of PRICE.
- Education: Learning about your condition, including proper body mechanics and strategies to avoid aggravating your knee, is vital for long-term management.
Strengthening Exercises
Strengthening the muscles surrounding the knee is crucial for stability and pain relief. Physiotherapists will guide you through targeted exercises that focus on the quadriceps, hamstrings, and calves. These exercises help improve strength and support the knee joint, reducing strain and preventing further injuries.
Mobility and Flexibility
Maintaining mobility and flexibility in the knee is essential for functional movement. Physiotherapy includes stretching exercises and gentle range-of-motion activities to help restore flexibility and reduce stiffness. This focus on mobility not only alleviates pain but also enhances your overall physical activity levels.
Knee Pain Prevention Strategies
Preventing future knee pain is a key aspect of physiotherapy. Your physiotherapist will educate you on proper techniques for daily activities, including walking, climbing stairs, and exercising. They will also address any risk factors, such as muscle imbalances or poor posture, to help you avoid re-injury.
FAQs
Can a physiotherapist help with my knee pain?
Yes, physiotherapists specialize in treating knee pain through tailored rehabilitation programs that target the underlying causes and symptoms.
What should I expect during my first visit to Triangle Physiotherapy?
During your first visit, you’ll undergo a comprehensive assessment, where your physiotherapist will evaluate your knee’s condition, discuss your medical history, and outline your treatment goals. A personalized plan will be created based on this information.
How many sessions will I need?
The number of sessions varies depending on the severity of your knee pain and your progress. Some patients may notice improvement in a few sessions, while others may require ongoing treatment. Your physiotherapist will provide an estimate during your assessment.
Do I need a referral to see a physiotherapist?
No, you do not need a referral to access physiotherapy services. You can book an appointment directly, unless required by your insurance for billing purposes.
How soon can I expect pain relief?
Many patients report relief within a few sessions, but the timeline may vary based on individual circumstances and the underlying cause of the knee pain.
How can I ensure effective management of my knee pain?
Engaging in physiotherapy, adhering to your rehabilitation plan, and performing prescribed exercises regularly are vital for managing knee pain effectively. Open communication with your physiotherapist will also help track your progress.
Conclusion
Physiotherapy is a powerful resource for managing knee pain. By understanding the nature of your condition and engaging in a tailored treatment plan, you can alleviate pain, restore function, and improve your quality of life. If you’re struggling with knee pain, consider the benefits that physiotherapy can provide in your recovery journey. To get help for your knee pain, you can call any of the locations of Triangle Physiotherapy or simply Book An Appointment online.
When you’re dealing with pain, injury, or chronic conditions like arthritis, choosing the right physiotherapist can make all the difference in your recovery. Physiotherapy is an essential part of managing pain, improving mobility, and enhancing your quality of life. However, with so many options out there, how do you know which physiotherapist is the best fit for your needs? At Triangle Physiotherapy in Toronto we have physiotherapists with varying specialties – from musculoskeletal to pelvic health to kid’s rehab.
In this blog, we’ll explore key factors to consider when selecting a physiotherapist.
1. Specialization Matters
Physiotherapy is a broad field, and different physiotherapists specialize in different areas. Whether you’re recovering from surgery, managing arthritis, or dealing with a sports injury, finding a physiotherapist who specializes in your specific condition can speed up your recovery and improve outcomes.
- For Arthritis and Joint Pain: Look for a physiotherapist with experience in managing musculoskeletal conditions like osteoarthritis or rheumatoid arthritis. They will be skilled in using therapeutic exercises, manual therapy, and pain management techniques to help reduce stiffness and improve mobility.
- For Sports Injuries: If you’re recovering from a sports-related injury, you might want a physiotherapist with experience in sports rehabilitation. They can tailor exercises that enhance strength and flexibility, preventing future injuries.

2. Physiotherapist Credentials and Experience
Check for credentials, such as a degree in physiotherapy (e.g., DPT or MSc in Physiotherapy) and any additional certifications related to your condition (e.g., orthopedic manual therapy or pelvic floor rehabilitation). More importantly, consider their experience: a physiotherapist with years of hands-on experience will likely be more adept at handling complex cases.
- Ask about their track record: How many patients have they treated with conditions like yours? Do they have experience working with people of your age group or fitness level?
3. Personalized Approach
Physiotherapy isn’t a one-size-fits-all treatment. It’s essential to find a physiotherapist who tailors treatment plans to your unique needs, rather than offering a generic approach. A skilled physiotherapist will conduct a thorough assessment of your physical condition, history, and goals before recommending treatment. This personalized approach ensures that you’re getting the care you need.
- Look for a physiotherapist who listens: A good physiotherapist will ask about your symptoms, lifestyle, and preferences to develop a treatment plan that works for you. They should be willing to adjust the plan if something isn’t helping or if new issues arise.
4. Approach to Communication
Effective communication is key to a successful physiotherapy experience. You’ll need to feel comfortable discussing your symptoms, goals, and progress with your physiotherapist. Clear communication helps ensure you understand your treatment plan and feel empowered to follow it.
- Ask about the treatment philosophy: Some physiotherapists emphasize hands-on techniques like manual therapy, while others focus on exercise-based rehabilitation. Ensure that the therapist’s methods align with your preferences and comfort levels.
- Check their availability: Some physiotherapists may be available for short, frequent sessions, while others may offer longer, less frequent appointments. Be sure that their schedule works with yours and that they are accessible for follow-up questions.
5. Physiotherapist Reputation and Reviews
One of the best ways to evaluate a physiotherapist is by asking for recommendations or reading online reviews. Hearing from others who have experienced similar conditions can give you insight into the therapist’s expertise and the quality of care they provide.
- Ask for recommendations: Your doctor, friends, or family members may have personal experiences to share. Word-of-mouth can often lead to finding a trusted physiotherapist.
- Online reviews: Patient reviews can provide valuable insights into a physiotherapist’s approach, professionalism, and success in treating various conditions.
6. Location and Accessibility
Convenience is important when committing to regular physiotherapy sessions. Look for a clinic that is easily accessible, whether it’s near your home or workplace. Consider the hours of operation and the availability of appointments that fit your schedule.
- Travel and parking: Make sure the location is convenient, and check whether there are parking facilities or easy access via public transport.
If you’re unsure of the type of physiotherapy you need, contact us at Triangle Physiotherapy. Our committed team is here to support you in reaching your health and wellness goals—whether you’re a seasoned athlete, a casual enthusiast, or embarking on your fitness journey for the first time.
As parents, ensuring the well-being and development of your child is a top priority. When a child faces physical challenges, whether due to an injury, developmental delay, or congenital condition, pediatric physiotherapy can play a crucial role in their recovery and overall health. But what exactly does pediatric physiotherapy entail, and how can it help your child? This guide will provide you with the information you need to understand this vital area of care.
Our kid’s physiotherapists at Triangle Physiotherapy Erin Mills have the expertise and experience to help children and their parents navigate these challenges.
What is Pediatric Physiotherapy?

Pediatric physiotherapy is a specialized branch of physiotherapy that focuses on assessing, diagnosing, and treating physical issues in children from birth through adolescence. It addresses a wide range of conditions, from mobility problems in infants to rehabilitation following sports injuries in teenagers. Pediatric physiotherapists work with children to improve movement, strength, coordination, and balance, helping them reach developmental milestones and recover from injuries or surgeries.
Why is it Important?
Children’s bodies are constantly growing and changing, and their needs are quite different from those of adults. Physiotherapy for children takes into account their unique developmental stages and physical capabilities. Whether it’s helping a newborn with a condition like torticollis or guiding a toddler through developmental delays, pediatric physiotherapists offer tailored interventions that focus on the individual child.
Here are some common reasons parents seek pediatric physiotherapy for their children:
- Developmental Delays: Some children may experience delays in reaching key milestones, such as sitting, walking, or speaking. Physiotherapists can help address these delays through targeted exercises and strategies to support physical development.
- Musculoskeletal Conditions: Conditions such as scoliosis (curvature of the spine), cerebral palsy, or flat feet may require physical therapy to improve mobility, strength, and posture.
- Injuries: Children are naturally active, and accidents or sports injuries can happen. Physiotherapy is essential for rehabilitation, helping your child recover safely and effectively from fractures, sprains, or strains.
- Neurological Conditions: For children with neurological conditions, such as cerebral palsy or brain injuries, pediatric physiotherapists use specific techniques to help with movement, coordination, and strength, assisting in the development of motor skills.
What Happens During Pediatric Physiotherapy Sessions?
A pediatric physiotherapy session is designed to be engaging and fun, helping your child feel comfortable while addressing their specific needs. Here’s what you can expect during a typical session:
- Initial Assessment: The physiotherapist will begin by conducting a thorough evaluation of your child’s medical history, current symptoms, and physical development. They may observe your child’s movement patterns and perform physical tests to assess strength, flexibility, coordination, and balance.
- Personalized Treatment Plan: Based on the assessment, the physiotherapist will create a customized treatment plan that includes specific exercises and interventions to help your child. The plan will focus on improving the areas that need attention and may involve activities designed to develop motor skills, increase strength, and improve mobility.
- Therapeutic Techniques: Treatment often includes exercises, stretches, and play-based activities that target your child’s specific needs. The physiotherapist may also use modalities such as massage, heat, or cold therapy, depending on the condition being treated.
- Family Involvement: Pediatric physiotherapists understand that a child’s care requires support from parents or caregivers. They will guide you on how to continue the exercises at home and offer advice on how to encourage your child’s progress outside of therapy sessions.
How Can Pediatric Physiotherapy Help Your Child?
Pediatric physiotherapy offers numerous benefits to children, including:
- Improved Mobility and Strength: Whether your child has a musculoskeletal condition, developmental delay, or injury, physiotherapy can enhance their movement abilities, making everyday tasks easier and promoting independence.
- Enhanced Coordination: Through targeted exercises, physiotherapy helps improve coordination and balance, which is essential for physical activities, sports, and even basic movements like walking or running.
- Pain Relief: If your child is experiencing pain due to an injury or condition, physiotherapy can help reduce discomfort by addressing the root cause and improving strength and mobility.
- Better Posture: Pediatric physiotherapists can help with postural issues, such as scoliosis or flat feet, improving alignment and preventing future complications.
- Increased Confidence: As children progress in their physical development and reach milestones, they often gain greater confidence in their abilities, which can positively impact other areas of their lives.
Kids physiotherapy in Mississauga is an essential service that can support your child’s physical development, recovery, and overall well-being. Whether your child is dealing with an injury, a developmental delay, or a specific condition, pediatric physiotherapists provide individualized care to help them reach their fullest potential. If you believe your child may benefit from physiotherapy, consult a pediatric physiotherapist who can assess their needs and develop a tailored treatment plan. By doing so, you’ll be supporting their physical growth and ensuring they thrive in every stage of life.
Get in touch with us at Triangle Physiotherapy Erin Mills to see how we can help you and your child!
Chemotherapy is an essential treatment for many types of cancer, but it often comes with side effects that can vary widely from person to person. While chemotherapy works to eliminate cancer cells, it can also affect healthy cells, leading to a range of physical symptoms. These side effects can be temporary, but they may be uncomfortable and affect your daily life.
When it comes to the side effects of cancer treatment, the cancer rehabilitation physiotherapists at Triangle Physiotherapy are knowledgeable and trained in helping you regain function and get back your quality of life.

In this post, we’ll cover 5 common symptoms to expect after chemotherapy and tips on how to manage them.
1. Fatigue
Fatigue is one of the most common side effects following chemotherapy. Unlike typical tiredness, this type of exhaustion can be overwhelming and persistent, making even the smallest tasks feel like a major effort. Chemotherapy can affect your red blood cells, which are responsible for carrying oxygen throughout your body, leading to feelings of extreme tiredness.
- What you can do: Try to rest when needed, but don’t forget to incorporate light activity into your day, like short walks or stretching. Small, frequent activities can boost your energy levels and help prevent muscle weakness. Additionally, make sleep a priority, and aim for a balanced diet to ensure your body has the nutrients it needs to recover.
2. Nausea and Vomiting
Chemotherapy drugs can trigger nausea and vomiting, which are especially common right after treatment. These symptoms occur because the chemotherapy affects the gastrointestinal tract, leading to discomfort in your stomach. The severity of nausea can vary depending on the drugs used, but it’s one of the most common concerns for many patients undergoing treatment.
- What you can do: Your doctor may prescribe anti-nausea medications, so make sure to take them as directed. Drinking small sips of water, ginger tea, or clear broths can help settle your stomach. Also, eating smaller, more frequent meals—rather than larger meals—can prevent your stomach from feeling overwhelmed. Avoiding heavy, greasy, or spicy foods may also reduce nausea.
3. Hair Loss
Hair loss is often one of the more noticeable side effects of chemotherapy. The powerful medications used during chemotherapy target rapidly dividing cells, including those in your hair follicles, which can cause your hair to fall out. Hair loss can begin within a few weeks of starting chemotherapy and can affect not just the scalp, but eyebrows, eyelashes, and body hair as well.
- What you can do: While hair loss is difficult to avoid, there are ways to manage it emotionally. Many people choose to wear wigs, scarves, or hats to help them feel more comfortable. If hair loss is affecting your self-esteem, consider talking to a counselor or joining a support group to help cope with the emotional impact. The good news is that hair usually starts to grow back once treatment is complete, though it might have a different texture or color temporarily.
4. Sensation Loss (Neuropathy)
Chemotherapy can cause nerve damage, leading to sensations of numbness, tingling, or weakness, particularly in the hands and feet. This condition, known as peripheral neuropathy, can be distressing and affect your ability to perform daily tasks like buttoning a shirt or walking. It happens because chemotherapy can damage the nerves responsible for sending signals to the brain, leading to these sensations.
- What you can do: While there’s no quick fix for neuropathy, there are ways to manage it. Talk to your doctor about medications that can help with nerve pain or discomfort. You might also benefit from physical therapy, which can help you improve balance and coordination. Taking care of your feet and hands by avoiding injury and wearing comfortable, well-fitting shoes can also reduce the impact of neuropathy. If you’re struggling with these symptoms, your healthcare provider can suggest exercises or tips to help alleviate the discomfort.
5. Changes in Appetite and Taste
Another side effect many chemotherapy patients experience is a shift in their appetite or the way food tastes. Chemotherapy can alter your sense of taste, often causing food to have a metallic or bitter flavor. In some cases, you might feel a loss of appetite, making it harder to eat enough to maintain your strength.
- What you can do: Try eating smaller meals more often throughout the day. If your appetite is low, experiment with foods that have strong flavors, such as citrus fruits or savory herbs, to help stimulate your taste buds. If food tastes off, using plastic utensils or drinking through a straw can sometimes help reduce the metallic taste. Additionally, staying hydrated and maintaining a balanced diet is important to ensure you’re getting enough nutrients.
Chemotherapy can be a life-saving treatment, but it often comes with side effects that may affect your quality of life. Fatigue, nausea, hair loss, sensation loss, and changes in appetite or taste are common symptoms that many patients face, but they are manageable with the right care and support. It’s important to communicate openly with your healthcare team about any symptoms you’re experiencing so they can adjust your treatment plan or provide supportive care to ease discomfort.
Cancer rehab will help you get back on your feet and help get rid of your neuropathy gradually. For breast cancer rehab, please remember to consult our expert physios who will help you get rid of the tight inelastic cords that formed due to radiation. You may notice it as shoulder restriction, but it needs to be treated by a physiotherapist over time.
Remember, recovery from chemotherapy is a gradual process, and many of these side effects will improve after treatment ends. Focus on taking care of your body, staying connected with your medical team, and reaching out for support when needed.
Reach out to us at Triangle Physiotherapy to book an assessment to get help managing Cancer Treatment side effects.
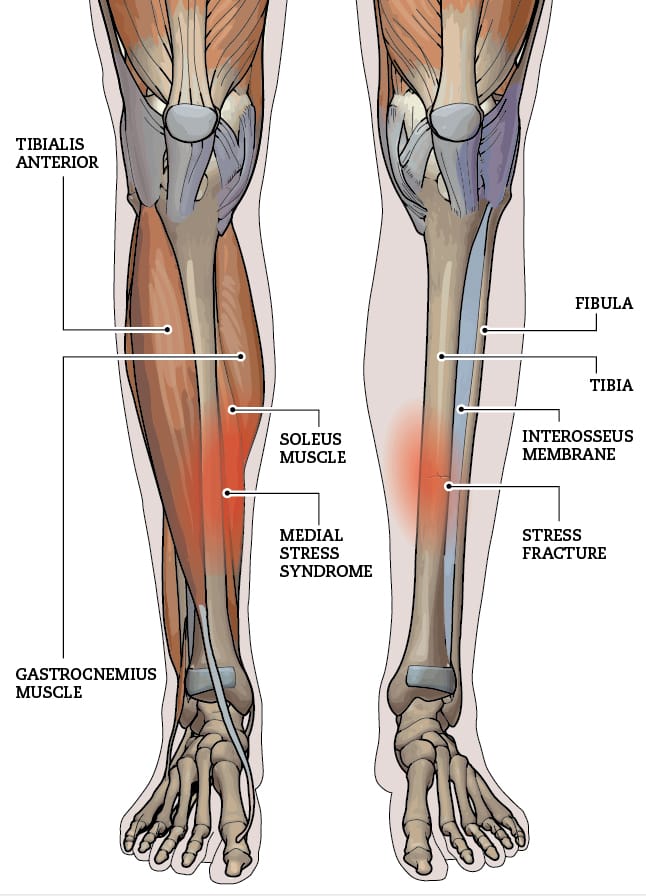
Tibial stress fractures are a common injury among runners, often arising from overuse and repetitive impact on the lower legs. These small discontinuous fractures in the tibia can lead to significant pain and time spent off the tracks, making understanding, recovery, and prevention crucial for athletes. Let’s explore the nature of tibial stress fractures, how to recover effectively, and strategies to prevent future injuries.
Our physiotherapists at Triangle Physiotherapy have the expertise and experience to help with injuries such as these.

FAQs on Tibial Stress Fractures
Q: What are the symptoms of a tibial stress fracture?
A: Common symptoms include localized pain along the shin, swelling, and tenderness that worsens with activity.
Q: How long does it take to recover from a tibial stress fracture?
A: Recovery time can vary, typically ranging from 6 to 12 weeks, depending on the severity of the fracture and adherence to a proper recovery plan.
Q: Can I still run with a tibial stress fracture?
A: It’s essential to avoid running until cleared by a healthcare professional, as continuing to run can worsen the injury.
Q: What type of shoes should I wear to prevent tibial stress fractures?
A: Look for shoes that offer good cushioning and support, tailored to your foot type and running style.
Q: Are there any specific exercises I should avoid during recovery?
A: High-impact exercises should be avoided initially; focus on low-impact activities until fully recovered. By understanding tibial stress fractures and employing the right recovery and prevention strategies, runners can bounce back stronger and continue enjoying their sport safely.
Understanding Recovery of Tibial Stress Fractures
Recovering from a tibial stress fracture involves a multifaceted approach that emphasizes rest and gradual rehabilitation. Initially, it’s essential to reduce weight-bearing activities to allow the bone to heal properly. Depending on the severity of the fracture, this may require crutches or a walking boot. Once the initial pain subsides, a structured recovery plan should include a gradual return to activity, typically guided by a Physiotherapist. Monitoring pain levels during this phase is critical; any increase in pain may indicate that you are pushing too hard, too soon.
Neuromuscular Exercises for Tibial Stress Fractures
Neuromuscular exercises play a vital role in recovery by enhancing coordination, balance, and muscle strength. These exercises can help to correct any biomechanical issues that may have contributed to the injury. Examples include: Balance training: Improve balance and strengthen stabilizing muscles. Agility drills- Help enhance neuromuscular control and prevent future injuries. Proprioception training- Activities like balance boards can improve body awareness and stability. Incorporating these exercises into your routine can significantly aid in the healing process and prepare your body for a return to running.
Mobility Incorporation
Restoring mobility is another critical aspect of recovery. Restricted movement can lead to stiffness and further complications. Gentle stretching and mobility exercises can help maintain flexibility in the surrounding muscles and joints. Key mobility exercises can include working on key muscles like Calf, Hip flexor mobility to name a few. Regularly integrating these mobility exercises will not only aid in recovery but also improve overall performance in the long run.
Progressive Resistance Exercises
Once you are pain-free and have regained some mobility, incorporating progressive resistance exercises is essential for rebuilding strength. This phase focuses on strengthening the muscles surrounding the tibia to provide better support and prevent future stress fractures. Examples include strengthening the calves and improving ankle stability, build strength in the quadriceps, hamstrings, and glutes. Start with light resistance and gradually increase intensity as your strength improves, always prioritizing proper form to prevent re-injury.
Prevention
Preventing tibial stress fractures is all about maintaining a balanced training regimen. Pay attention to warning signs such as persistent pain or fatigue and adjust your training accordingly. Integrating a proper rehab plan under the supervision of a physiotherapist along with proper relaxation techniques provided by Massage therapist can significantly reduce the risk of developing a tibial stress fracture and maintain your running routine.
Suffered a Tibial Stress Fracture Injury? Book an appointment with us to get on the road to recovery.
At Triangle Physiotherapy, we believe in offering comprehensive care that addresses the root causes of pain and discomfort, not just the symptoms. One of the key components of our holistic approach to rehabilitation and wellness is chiropractic care. Chiropractic treatments can be incredibly effective for a range of musculoskeletal issues, from back pain to headaches and joint stiffness. By integrating chiropractic care with physiotherapy, we provide a multidimensional approach to improve mobility, reduce pain, and enhance your overall quality of life.
What is Chiropractic Care?
Chiropractic care is a non-invasive form of treatment that focuses on diagnosing and managing musculoskeletal disorders, particularly those involving the spine. Chiropractors primarily work with spinal manipulation (also known as spinal adjustments) to correct misalignments in the spine and improve the function of the nervous system. By restoring proper alignment to the spine and joints, chiropractic care can help alleviate pain, improve mobility, and reduce inflammation.
While spinal adjustments are the cornerstone of chiropractic treatment, chiropractors at Triangle Physiotherapy also use a variety of other techniques such as soft tissue therapy, postural correction, and lifestyle education. The goal is to restore function, relieve pain, and optimize the body’s natural ability to heal itself.


The Role of Chiropractic Care in Your Wellness Journey
Chiropractic care at Triangle Physiotherapy is personalized to address your unique needs. Whether you’re dealing with acute pain from an injury, chronic conditions, or just looking to improve your overall mobility, chiropractic treatment can provide significant benefits. Here’s how chiropractic care can support your health and well-being:
1. Pain Relief and Improved Function
One of the primary reasons people seek chiropractic care is to find relief from pain, particularly in the back, neck, and joints. Spinal misalignments or subluxations can lead to pain, stiffness, and restricted movement. Chiropractic adjustments work to realign the spine and other joints, reducing pain, improving range of motion, and promoting better movement patterns. Many of our patients experience immediate relief from conditions such as sciatica, herniated discs, and whiplash.
Chiropractic care can also address issues with joint function in areas like the shoulders, hips, and knees. By improving joint mobility, chiropractic adjustments help alleviate discomfort caused by conditions such as arthritis, tendonitis, or muscle strains.
2. Headaches
Headaches, particularly tension headaches and migraines, are common complaints that can significantly impact daily life. Often, these types of headaches are triggered by muscle tension or misalignments in the neck and upper spine. Chiropractic care can address these issues by restoring proper alignment to the cervical spine, which can relieve pressure on nerves and muscles, reduce inflammation, and improve blood flow to the brain. Many patients report fewer and less severe headaches after incorporating chiropractic care into their wellness routine.
3. Sports Injury Rehabilitation
Whether you’re an athlete recovering from an injury or simply someone who enjoys staying active, chiropractic care can help speed up recovery and improve performance. Sports injuries, especially those related to the spine or joints, can be effectively treated with chiropractic adjustments, soft tissue techniques, and rehabilitative exercises. By restoring proper alignment and function, chiropractic care helps promote faster healing, reduce inflammation, and prevent future injuries.
Chiropractors at Triangle Physiotherapy work closely with physiotherapists to provide a combined approach to sports injury rehabilitation. This collaborative effort ensures that all aspects of recovery—pain management, mobility, strength, and flexibility—are addressed.
4. Postural Correction and Alignment
Over time, poor posture—whether from sitting at a desk, using electronic devices, or incorrect movement patterns—can lead to imbalances in the spine and musculoskeletal system. Misalignments in the spine can cause tension, discomfort, and long-term structural damage. Chiropractic care can help restore proper alignment, reduce tension, and improve overall posture.
At Triangle Physiotherapy, we provide postural assessments to identify areas where alignment may be contributing to pain or dysfunction. Chiropractic care, combined with physiotherapy exercises, can help improve posture and reduce the strain on the spine, shoulders, and neck. This, in turn, can lead to better movement, less discomfort, and improved overall health.
5. Stress Reduction and Relaxation
Chronic stress can take a toll on your body, causing muscle tension, headaches, and poor sleep. Chiropractic adjustments can help alleviate the physical effects of stress by reducing muscle tightness and promoting relaxation. By improving the function of the nervous system, chiropractic care can help the body respond more effectively to stress and tension. Many patients report feeling more relaxed and balanced after chiropractic treatments.
Integrating Chiropractic Care with Physiotherapy
At Triangle Physiotherapy, we offer a holistic, integrated approach to treatment. Our chiropractors and physiotherapists work together to create a comprehensive treatment plan that addresses your specific needs. While chiropractic care focuses on spinal and joint alignment, physiotherapy can complement this by strengthening muscles, improving flexibility, and providing rehabilitation exercises to support long-term recovery and injury prevention.
By combining chiropractic care with physiotherapy, we ensure that both the structure and function of your body are optimized for improved movement, reduced pain, and enhanced quality of life.
The Benefits of Chiropractic Care at Triangle Physiotherapy
- Personalized treatment plans tailored to your specific needs and goals.
- Non-invasive approach to pain relief, injury recovery, and overall wellness.
- Collaborative care that integrates chiropractic treatment with physiotherapy for maximum results.
- Long-term pain management for chronic conditions such as arthritis, back pain, and headaches.
- Posture correction and alignment strategies to prevent future injuries.
Chiropractic care is a powerful tool for improving mobility, relieving pain, and promoting overall wellness. At Triangle Physiotherapy, our experienced chiropractors work alongside our physiotherapy team to provide a comprehensive, personalized approach to your health. Whether you’re managing chronic pain, recovering from an injury, or simply looking to enhance your physical well-being, chiropractic care can help you achieve lasting results.
Key Takeaways:
- Chiropractic care addresses pain, injury, and dysfunction by restoring spinal and joint alignment.
- It can provide relief from conditions like back pain, headaches, and sports injuries.
- Combining chiropractic care with physiotherapy enhances recovery, mobility, and overall wellness.
- Regular chiropractic care promotes long-term health and injury prevention.
If you’re looking for an effective, non-invasive way to improve your health, reduce pain, and enhance your mobility, chiropractic care at Triangle Physiotherapy may be the solution you need. Contact us today to learn how we can help you feel your best!
Vestibular disorders are conditions that affect the inner ear and the brain’s ability to process balance and spatial information. These disorders can lead to symptoms like dizziness, vertigo, unsteadiness, and difficulty maintaining balance. They can significantly impact daily life, making it hard to perform routine tasks such as walking, driving, or even standing up without feeling lightheaded. Fortunately, physiotherapy can play a crucial role in managing vestibular disorders and helping patients regain their balance and quality of life.
At Triangle Physiotherapy Clinic, we understand how disruptive vestibular issues can be. In this blog, we’ll explore the role of physiotherapy in treating these conditions, the various treatment techniques involved, and how physiotherapists help patients manage their symptoms.
Understanding Vestibular Disorders
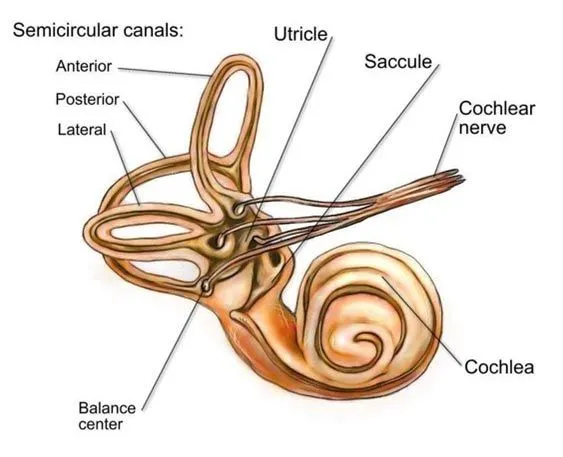
The vestibular system, located in the inner ear, is responsible for maintaining balance and spatial orientation.
When there is a disruption to this system, such as an infection, injury, or degenerative condition, it can lead to a variety of symptoms:
- Dizziness or vertigo: A sensation that the world is spinning or moving.
- Balance problems: Difficulty standing or walking without feeling unsteady.
- Nausea: Often occurring in response to dizziness or vertigo.
- Sensitivity to movement: Everyday actions like turning the head or standing up can trigger symptoms.
Common vestibular disorders include benign paroxysmal positional vertigo (BPPV), Meniere’s disease, vestibular neuritis, and labyrinthitis. While medication can help alleviate some symptoms, physiotherapy offers an effective, non-invasive solution to manage and improve vestibular function.
How Physiotherapy Helps with Vestibular Disorders
For patients with Benign Paroxysmal Positional Vertigo (BPPV), physiotherapists use canalith repositioning maneuvers to relieve vertigo. This condition occurs when small calcium crystals in the inner ear become dislodged, disrupting your balance.
1. Vestibular Rehabilitation Therapy (VRT)
Vestibular Rehabilitation Therapy uses targeted exercises to improve balance and reduce dizziness. It retrains your brain and vestibular system to process sensory information accurately. VRT proves highly effective for conditions like BPPV, where the inner ear’s balance organs are affected, and for other vestibular disorders.
- What it involves: VRT typically includes exercises that focus on head and eye coordination, balance training, and habituation (getting used to movements that trigger dizziness). These exercises help the brain compensate for the imbalance caused by the vestibular disorder and improve overall stability.
- How it works: For example, exercises may include specific head movements to treat BPPV, which involves repositioning tiny crystals in the inner ear that cause vertigo. Other exercises focus on improving gaze stability and postural control, helping you maintain balance during daily activities.
2. Canalith Repositioning Maneuvers
For patients with Benign Paroxysmal Positional Vertigo (BPPV), a common vestibular disorder, physiotherapists can use specific head movements called canalith repositioning maneuvers to help alleviate vertigo. BPPV occurs when small calcium crystals in the inner ear become dislodged and disrupt the balance system.
- What it involves: The therapist performs precise head and body movements designed to move the displaced crystals back to their correct position. One well-known technique used for BPPV is the Epley maneuver, which has been proven to significantly reduce or eliminate symptoms of vertigo.
- How it works: By repositioning the crystals, the inner ear’s ability to send accurate balance signals to the brain is restored, providing relief from dizziness and vertigo.
3. Balance and Postural Training
Improving balance and posture is a cornerstone of vestibular rehabilitation. Many patients struggle with standing, walking, or turning their head without feeling unsteady. Physiotherapists use exercises that strengthen core muscles, enhance coordination, and rebuild your confidence in movement.
- What it involves: Training may include balance exercises performed while standing, sitting, or moving. These exercises are designed to challenge the body’s stability and improve proprioception (the sense of where your body is in space). By improving core strength, posture, and coordination, these exercises help reduce the risk of falls and promote more controlled movements.
- How it works: Balance exercises may include standing on one foot, walking in a straight line, or practicing functional movements like bending down to pick up an object. These exercises help retrain the brain to process information more effectively, which leads to better balance during everyday activities.
4. Gaze Stabilization Exercises
For patients with vestibular disorders, focusing on objects while moving the head can be particularly challenging. Gaze stabilization exercises (using laser and vestibular charts) are designed to improve the ability to maintain visual focus while the head is in motion, which is essential for activities like reading, driving, or walking in a crowded place.
- What it involves: The physiotherapist may instruct the patient to follow a moving target with their eyes or perform head movements while keeping their gaze fixed on a target. Over time, these exercises help reduce symptoms like dizziness that occur when the head moves quickly or when visual tracking is required.
- How it works: Gaze stabilization exercises help retrain the vestibular system and visual pathways to work together, improving your ability to maintain focus and orientation in dynamic environments.
5. Education and Self-Management Strategies
An often overlooked part of vestibular rehabilitation is educating patients on how to manage their symptoms independently. Understanding your condition, learning how to modify certain movements, and incorporating strategies to reduce triggers can help you maintain a better quality of life.
- What it involves: Your physiotherapist will provide education on lifestyle modifications, including techniques for managing dizziness during daily activities, posture correction, and tips for improving overall health (such as hydration and proper nutrition).
- How it works: Knowledge is power—by learning about your condition and how it affects your body, you’ll be better equipped to handle potential flare-ups and manage symptoms on your own. Your physiotherapist will empower you to take control of your recovery through self-management strategies.
Final Thoughts
Vestibular disorders can significantly impact your daily life, but physiotherapy offers a highly effective, non-invasive treatment option to help manage symptoms and improve overall balance and stability. Whether you’re dealing with vertigo, dizziness, or balance problems, a tailored physiotherapy program can help you regain control and reduce the impact of these disruptive symptoms.
At Triangle Physiotherapy, our team of experienced physiotherapists is here to guide you through every step of your recovery. If you’re struggling with a vestibular disorder, don’t wait—reach out to us today to schedule an assessment and begin your journey towards better balance and well-being.
Pelvic Physiotherapy, a specialized form of physiotherapy, plays a vital role in helping men regain control, improve function, and enhance their quality of life after prostate cancer treatment.
Prostate cancer is one of the most common cancers affecting men worldwide. While advances in medical treatments like surgery, radiation, and chemotherapy have improved survival rates, the recovery process can often come with a range of physical challenges. One area that is often overlooked is the pelvic health of men post-prostate cancer treatment.
Get in touch with us at Triangle Physiotherapy, we have physiotherapists that are trained in cancer rehabilitation as well as pelvic health. We can help you recover from the side effects of cancer treatment and regain your quality of life.
Prostate Cancer and Its Impact
Prostate cancer typically develops in the prostate gland, a small organ located below the bladder. Treatment options can include surgery (prostatectomy), radiation therapy, hormone therapy, or chemotherapy. While these treatments are effective in managing cancer, they often lead to side effects, particularly in the pelvic region. Common issues that arise after prostate cancer treatment include urinary incontinence, erectile dysfunction, pelvic pain, and difficulty with bowel control.
These conditions can significantly affect a man’s physical and emotional well-being, leading to decreased quality of life, social withdrawal, and even depression. This is where pelvic rehabilitation comes in.
What Is Pelvic Rehabilitation?
Pelvic rehabilitation is a specialized form of physical therapy that focuses on restoring function to the pelvic floor muscles and addressing issues related to the pelvic organs. These muscles support the bladder, bowel, and reproductive organs. For men recovering from prostate cancer, pelvic rehabilitation can help restore strength, control, and coordination in the pelvic region, leading to improvements in urinary control, sexual function, and overall pelvic health.
A trained pelvic health physiotherapist will assess the patient’s specific symptoms and develop a personalized treatment plan. The goal is to reduce discomfort, improve mobility, and enhance the patient’s ability to resume normal daily activities.
How Pelvic Health Physiotherapy Helps After Prostate Cancer Treatment
1. Improving Urinary Control
Urinary incontinence is a common side effect after prostate cancer surgery or radiation. The pelvic floor muscles, which help control urine flow, can become weakened or damaged during treatment. Pelvic rehabilitation techniques, including exercises to strengthen these muscles, can help men regain bladder control and reduce the frequency of leaks. Kegel exercises and electrical stimulation are often used to retrain the pelvic floor muscles and improve urinary continence.
2. Enhancing Sexual Function
Erectile dysfunction (ED) is another common concern after prostate cancer treatment. Pelvic rehabilitation can help address ED by improving blood flow to the penis and strengthening the pelvic floor muscles that contribute to sexual function. Manual therapy, muscle retraining, and pelvic exercises can also help men regain confidence and improve their sexual health.
3. Relieving Pelvic Pain
Pelvic pain or discomfort can persist after treatment, especially if nerve tissue was affected during surgery or radiation. Manual therapy techniques such as myofascial release, soft tissue mobilization, and gentle stretching can help relieve pain, improve flexibility, and reduce tension in the pelvic area.
4. Improving Bowel Function
For some men, prostate cancer treatment can lead to bowel dysfunction, such as constipation or fecal incontinence. Pelvic rehabilitation techniques can help restore normal bowel function by strengthening the muscles involved in bowel control and improving coordination between the pelvic floor and the digestive system.
The Importance of Early Intervention
The sooner men begin pelvic rehabilitation after prostate cancer treatment, the better the outcomes. Early intervention can help prevent long-term complications, reduce recovery time, and improve overall quality of life. It’s important to consult a pelvic health physiotherapist who specializes in post-cancer recovery for a personalized treatment plan.
Call us today to book an appointment and learn about how we can help you.
Arthritis and joint pain are common conditions that can significantly affect daily life. These issues often lead to discomfort, stiffness, and decreased mobility, making everyday activities challenging. Fortunately, physiotherapy offers effective strategies to manage these symptoms and improve quality of life.
If you would like to learn more about how Triangle Physiotherapy can help you manage your arthritis pain, contact us today!
Understanding Arthritis and Joint Pain
Arthritis encompasses various conditions that cause inflammation in the joints, leading to pain and stiffness. Osteoarthritis and rheumatoid arthritis are two prevalent types. While arthritis can be caused by age, injury, or autoimmune disorders, the impact on an individual’s well-being can be profound. Beyond physical discomfort, arthritis can lead to emotional distress and social withdrawal, emphasizing the need for effective management strategies.
The Role of Physiotherapy for Arthritis

Physiotherapy is a cornerstone in managing arthritis and joint pain. A skilled physiotherapist can assess your condition and create a personalized treatment plan tailored to your specific needs. This plan may include various interventions, such as manual therapy, therapeutic exercises, and education about joint protection techniques.
Tailored Exercise Programs
Exercise is crucial for managing arthritis. A physiotherapist can guide you in developing a safe and effective exercise routine that enhances strength, flexibility, and range of motion. Low-impact activities such as swimming, cycling, and walking are often recommended, as they minimize stress on the joints while promoting movement.
Manual Therapy
Manual therapy techniques, such as joint mobilization and soft tissue massage, can help alleviate pain and improve joint function. These hands-on approaches can reduce stiffness and enhance circulation around the affected joints, providing immediate relief and promoting long-term recovery.
Education and Self-Management Strategies
An essential aspect of physiotherapy is educating patients about their condition. Understanding arthritis and its impact on the body empowers individuals to make informed choices. Physiotherapists teach joint protection strategies, ergonomic principles, and how to modify activities to minimize strain on the joints. This knowledge helps individuals take an active role in managing their pain.
Incorporating Lifestyle Changes
In addition to physiotherapy, adopting a healthy lifestyle can further alleviate arthritis symptoms. Maintaining a balanced diet rich in anti-inflammatory foods, such as fruits, vegetables, and omega-3 fatty acids, can support joint health. Staying hydrated and managing stress through relaxation techniques can also be beneficial.
Tips for Managing Arthritis and Joint Pain
- Stay Active: Engage in regular, low-impact exercise to keep joints moving and muscles strong.
- Listen to Your Body: Be aware of your pain levels and modify activities as needed.
- Use Supportive Devices: Braces, splints, or orthotics can provide additional support and stability.
- Prioritize Rest: Ensure you get adequate rest to allow your body to recover.
- Consult Professionals: Always seek guidance from healthcare providers or physiotherapists before starting new activities.
Managing arthritis and joint pain can be challenging, but physiotherapy offers effective tools to enhance your quality of life. Through personalized treatment plans, education, and lifestyle adjustments, individuals can regain control over their bodies and reduce the impact of pain. With the right support and commitment to an active lifestyle, it is possible to live a fulfilling life despite arthritis. Embracing physiotherapy can be a transformative step towards achieving better joint health and overall well-being.