Back pain? You are not alone. Over 80 % of Canadians will experience back pain atleast once in their life. However, about 90% of back pain is not caused by any serious injury or disease. That being said, it doesn’t make it any less painful or debilitating. For a lot of people, traditional physiotherapy and massage therapy works well, but if it doesn’t don’t be discouraged… there is still hope! As a physiotherapist myself that has suffered from back pain, yoga has changed my life! It has helped me increase my flexibility, core strength, improve my posture and overall enhance my life.

Why Yoga?
1. Stretching
The spine is meant to move in lots of different ways. If we don’t move or stretch it gets stiff and rusty. This can start to cause some aches and pains which can get worse over time if it is not addressed. It can also make you more susceptible to becoming that 10% of people that suffer from a more significant injury. “But it hurts to move,” you say… Yes, oftentimes it does cause some discomfort to move especially if you haven’t tried to move in certain directions for a long time but science now tells us that it is far better for your back to move in a controlled and safe way rather than not moving. This is where yoga can help…. Yoga is a very gentle and proven way to help loosen up your back and make sure it moves smoothly within all its normal ranges of motion.
2. Strengthening
All of us have heard that if you have back pain you should strengthen your core, right? Yoga creates a great way of functionally strengthening your core. What that means is instead of isolating certain muscles, the yoga poses (asanas) that you are taken through will help you learn how to use all the muscles of your core together (including your diaphragm and pelvic floor!). If you continue strengthening your core on the ground then your body doesn’t get stronger in the positions it needs for everyday activities. For example, vacuuming your house requires you to be slightly bent over and pushing/pulling. Yoga poses that can simulate will force you to strengthen your core muscles in the positions it is needed so that once you get stronger, vacuuming won’t be painful.
There are many other benefits of yoga that can help with pain from breathing techniques (if it works for women in labour then it can work for your back pain too!) Also, mind-body awareness and connection is developed to help you realize if there are postures or positions that you are doing out of habit that you don’t realize can be harming your body. Yoga can correct imbalances of your musculoskeletal system that you didn’t even know existed.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Yoga can be a powerful tool for improving back health, enhancing flexibility, and reducing pain when combined with physiotherapy. For those seeking professional physiotherapy services to complement their yoga practice, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans to help you maintain a healthy back and overall well-being.
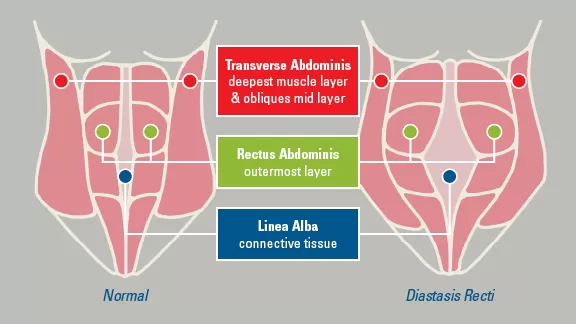
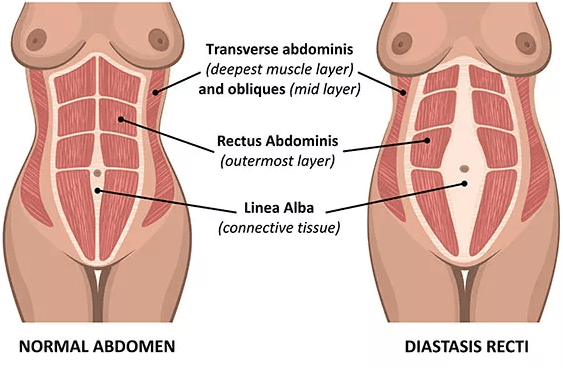
A Diastasis Recti Abdominus is a separation in the 6-pack muscle, the rectus abdominis.
How does it occur?
It most often occurs during pregnancy. Sometimes it will spontaneously correct following birth, but it does not always.
It can also occur with overstretch of abdominal musculature.
Why is it a problem?
There is no pain with this condition.
However, the abdominal wall and the core will become weak. Your abdominals work with your pelvic floor, so a separation of your rectus abdominis muscles can make your pelvic floor less efficient and may result in prolapse and incontinence.Your abdominals also work with your lower back musculature, therefore it can lead to lower back pain.
How do I know if I have a Rectus Diastasis?
If you lift your head while lying on your back and the center of your belly protrudes out, you may have a rectus diastasis. It is measured by the number of fingers you can fit between the muscle when lying on your back and lifting your head. Normal is 1/2 a finger above and below the belly button, and one finger at the belly button.
How do I treat it?
If the abdominal separation is greater than 4 fingers, an abdominal binder is recommended. If you use an abdominal binder, it should be from your hip bones to your rib cage, you need to keep the binder on 24/7. You can only take the binder off when you do your correction exercise below, or when you take a shower. You should keep it on at bedtime.
To get your pelvic health assessed, schedule a consultation with a pelvic floor physiotherapist at Triangle Physiotherapy!
Written by: Kamand Zendeganidoost, Registered Physiotherapist
Managing rectus diastasis effectively often involves specialized physiotherapy to strengthen the core and improve abdominal function. If you are seeking professional physiotherapy services for abdominal separation, consider visiting clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide expert care and personalized treatment plans to help you restore core stability and strength.
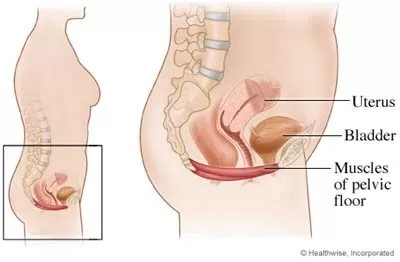
What is the Pelvic Floor?
The pelvic floor is a set of muscles that spread across the bottom of the pelvic cavity like a hammock. The pelvic floor has three openings that run through it, the urethra, the vagina, and the rectum. The functions of the pelvic floor include:
- Supporting the pelvic organs, specifically the uterus, the bladder, and the rectum
- To help provide sphincter control for the bladder and bowel
- Withstanding increases in pressure that occur in the abdomen such as coughing, sneezing, laughing, straining, and lifting
- To enhance the sexual response
What causes pelvic floor dysfunction?
The pelvic floor becomes dysfunctional in many women when there is an imbalance in the joints, muscles, and connective tissue integrity.
- Weak pelvic floor muscles: contributing to stress incontinence, urge incontinence, and pelvic organ prolapse.
- Tight pelvic floor muscles: contributing to Urinary and Fecal Urgency, Urge Incontinence, Chronic Pelvic Pain, Dyspareunia, Vaginismus, Vulvodynia, Pudendal Neuralgia, Interstitial Cystitis and Chronic Prostatits.
One of the most commonly seen conditions by pelvic physiotherapists is stress incontinence in women.

What is Stress Urinary Incontinence?
Stress urinary incontinence is the involuntary release of urine during laughter, coughing, lifting of objects or any movement that increases pressure on your bladder. When the bladder is full, the muscles in the wall of your bladder contract forcing urine through the urethra and out of your body. Sphincter muscles and pelvic floor muscles keep the urethra closed to avoid leakage of urine. These muscles relax at the same time the bladder contracts in order to allow urine to exit your body.
Causes of stress incontinence:
Hormonal changes:
During the week before your menstrual cycle, estrogen levels fall, causing symptoms of stress urinary incontinence to worsen. Additionally, as a woman goes through menopause, estrogen levels also fall causing the pelvic floor muscles to weaken.
Pregnancy:
If you are pregnant, you may experience stress urinary incontinence due to hormonal changes and the enlarging size of the uterus. During pregnancy, estrogen levels are lower, leading to less muscular strength in the sphincter and pelvic floor muscles. Additionally, as the fetus grows extra weight is placed on your bladder.
Childbirth:
Vaginal delivery can damage your pelvic floor muscles making urine leakage more likely. The supporting tissues of your bladder can also be damaged during vaginal delivery causing a cystocele, or prolapse of your bladder, symptoms of which include urinary incontinence. You may not know you have suffered damage to your pelvic floor until after you have gone through menopause, when the pelvic floor muscles are further weakened due to a fall in estrogen levels.
Hysterectomy and other surgery:
The bladder and uterus are very close together and have common supporting ligaments and muscles. Surgery to, or removal of your uterus as in a hysterectomy, risks damage to the supporting structures of your bladder. If these supporting structures are damaged, a cystocele is likely to occur. Symptoms of a cystocele include urinary incontinence.
Illnesses:
When you are ill and suffering from severe coughing, the pelvic floor muscles may fatigue and allow temporary stress incontinence due to an increase in abdominal pressure experienced while coughing.
Obesity:
Obesity can increase the abdominal pressure on the bladder leading to urinary incontinence.
Neurological damage:
Any neurological disorder such as multiple sclerosis, Parkinson’s disease or stroke can cause urinary incontinence by interfering with the nerve signals that control your bladder. Additionally, if the nerves that supply your bladder or pelvic floor muscles are damaged, urinary incontinence may also result
How is Stress Urinary Incontinence treated?
Treatments of stress urinary incontinence are individual based. The following should be considered:
Pelvic floor muscle strengthening:
Strengthening the supporting muscles of your bladder is very effective inhelping stress urinary incontinence.
Bladder training
Bladder training involves learning to delay the urge to urinate. You areinstructed to breathe deeply, relax, and distract yourself with another activitywhen you feel the urge. The initial goal is to delay urination by increments and eventually once every2 to 4 hours.
Pessary
Pessaries can help when a cystocele or prolapsed bladder is the cause forurinary incontinence. A pessary is a device of various shapes and sizes that isplaced in the vagina to support the bladder and keep it in place.
Surgery
For severe cystoceles, or bladder prolapses, surgery is needed in order tocorrect the position of the bladder and help with urinary incontinence.
Important Tips
- Avoid constipation. Repeated straining can have a very damaging effect on the pelvic floor muscles.
- It’s important for women to be active. Regular exercise and recreational sporting activities play a key role in keeping women fit and healthy well into old age
- Drink plenty of water
- Learn to tighten your pelvic floor muscles before you cough, sneeze or lift heavy items.
To get your pelvic health assessed, schedule a consultation with a pelvic floor physiotherapist at Triangle Physiotherapy and Rehabilitation!
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Maintaining a strong pelvic floor is essential for overall health, especially in managing incontinence, pelvic pain, and postpartum recovery. For those seeking professional physiotherapy services to strengthen their pelvic floor, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and personalized treatment plans to help you achieve optimal pelvic health and well-being.