Pelvic Health – Menstrual cups and menstrual discs are reusable feminine hygiene products designed to collect menstrual fluid.

What is a Menstrual Cup?
Menstrual cups are generally crafted from silicone or rubber.
Unlike tampons, which absorb blood, these cups collect it, reducing the risk of infection.
One advantage of the menstrual cup is its larger capacity compared to a tampon’s absorbency, allowing for less frequent changes. Most cups can be worn for up to 12 hours, depending on your flow.
What is a Menstrual Disc?
Unlike menstrual cups, menstrual discs sit higher in the vaginal canal, tucked behind the pubic bone. Here are some key features and benefits of menstrual discs:
- Design and Use:
- Shape: Menstrual discs are flat and round, resembling a small diaphragm, with a flexible rim and a thin, flexible body.
- Insertion: The disc is pinched and inserted into the vagina, where it is positioned horizontally and covers the cervix.
- Capacity: Like menstrual cups, discs can hold a significant amount of fluid and can be worn for up to 12 hours.
What are the benefits of a Menstrual Cup?
Benefits:
- Cost-Effective: While the initial purchase price may be higher than disposable products, menstrual cups can be reused for several years, saving money over time.
- Eco-Friendly: Reusable nature reduces waste compared to disposable tampons and pads.
- Health: Made from medical-grade materials that are safe and reduce the risk of Toxic Shock Syndrome (TSS) associated with tampons.
What are the benefits of a Menstrual Disc?
Benefits:
- Comfort: Positioned differently than cups, discs can be more comfortable for some users, especially during physical activities or sex.
- Mess-Free Intercourse: Many menstrual discs can be worn during intercourse without obstructing the vaginal canal, offering a mess-free experience.
- Eco-Friendly: Reusable menstrual discs reduce waste compared to disposable products. However, there are also single-use disposable options available.
Using a Menstrual Cup Vs. a Menstrual Disc
Using a menstrual cup involves a few steps to ensure proper insertion, positioning, and removal. Here’s a detailed guide on how to use a menstrual cup:Insertion
Wash Your Hands:
- C-fold: Press the sides of the cup together and then fold it in half to form a “C” shape.Punch-down fold: Push the rim of the cup down into the base, creating a narrower point for insertion.
Duration:
Wash Your Hands:
Sterilization:
Using a menstrual disc involves a few steps to ensure proper insertion, positioning, and removal. Here is a detailed guide on how to use a menstrual disc:Insertion
Wash Your Hands:
Duration:
Wash Your Hands:
Sterilization:
Menstrual discs and cups are both effective options for period management. Choose the one that suits you best based on factors like comfort, lifestyle, and size preference. Ultimately, neither a disc nor a cup might be the right choice for you, but they are both excellent alternatives to tampons for those seeking different options.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Choosing between a menstrual cup and a menstrual disc can depend on individual comfort and pelvic health needs. For expert advice on pelvic health and guidance on using these products, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these locations can provide personalized care and support for all your pelvic health concerns.
Pelvic pain is discomfort or pain experienced in the lower part of the abdomen, below the belly button and between the hips. This type of pain can affect both men and women and can arise from various conditions. The nature of pelvic pain can vary; it might be sharp, dull, intermittent, or constant, and can be acute (short-term) or chronic (lasting longer than six months).
What causes pelvic pain?

Common Causes of Pelvic Pain
In Women:
- Menstrual Cramps: Pain associated with menstruation (dysmenorrhea).
- Endometriosis: A condition where tissue similar to the lining inside the uterus grows outside of it.
- Ovarian Cysts: Fluid-filled sacs on the ovaries.
- Pelvic Inflammatory Disease (PID): An infection of the reproductive organs.
- Fibroids: Noncancerous growths in the uterus.
- Ectopic Pregnancy: A pregnancy occurring outside the uterus.
- Interstitial Cystitis: Chronic inflammation of the bladder.
In Men:
- Prostatitis: Inflammation of the prostate gland.
- Hernia: When an organ pushes through an opening in the muscle or tissue.
- Chronic Pelvic Pain Syndrome (CPPS): Persistent pain in the pelvic region.
Both Genders:
- Urinary Tract Infections (UTIs): Infections in any part of the urinary system.
- Appendicitis: Inflammation of the appendix.
- Gastrointestinal Issues: Conditions such as irritable bowel syndrome (IBS) or diverticulitis.
- Musculoskeletal Issues: Problems with muscles, ligaments, or joints in the pelvic area.
What are the symptoms related to pelvic pain?
Symptoms of pelvic pain can vary widely depending on the underlying cause and the individual. Here are common symptoms associated with pelvic pain:
General Symptoms of Pelvic Pain
- Aching or Discomfort: Persistent or intermittent pain in the lower abdomen or pelvis.
- Sharp or Stabbing Pain: Sudden, severe pain that can come and go.
- Cramping: Muscle cramps or spasms in the pelvic region.
- Pressure: A feeling of heaviness or pressure in the pelvis.
- Burning or Stinging Sensation: Particularly during urination or bowel movements.
- Pain During Physical Activity: Pain that worsens with movement, exercise, or sexual intercourse.
Additional Symptoms in Women
- Menstrual Irregularities: Pain associated with periods (dysmenorrhea), heavy bleeding, or spotting between periods.
- Pain During Ovulation: Mid-cycle pain known as mittelschmerz.
- Pain During Sexual Intercourse: Discomfort or pain during or after sex (dyspareunia).
- Vaginal Discharge: Unusual discharge that might indicate infection.
- Pain with Urination: Particularly if associated with urinary tract infections or interstitial cystitis.
Additional Symptoms in Men
- Pain in the Testicles or Scrotum: Discomfort that can radiate to the pelvic region.
- Urinary Symptoms: Difficulty urinating, frequent urination, or pain during urination.
- Pain with Ejaculation: Discomfort during or after ejaculation.
Symptoms Related to Specific Conditions
- Endometriosis: Severe menstrual cramps, pain during intercourse, and infertility.
- Pelvic Inflammatory Disease (PID): Fever, unusual vaginal discharge, and pain during sex.
- Ovarian Cysts: Sudden, severe pain if a cyst ruptures or causes twisting of the ovary (torsion).
- Ectopic Pregnancy: Sharp, stabbing pain, vaginal bleeding, dizziness, or fainting.
- Interstitial Cystitis: Chronic pelvic pain, urinary urgency and frequency, and pain during intercourse.
- Prostatitis: Pain in the pelvis, genitals, or lower back; difficulty urinating; flu-like symptoms.
- Appendicitis: Sudden, sharp pain that starts near the belly button and moves to the lower right abdomen, accompanied by fever, nausea, and vomiting.
- Hernia: A noticeable bulge in the groin or abdomen, pain that worsens with lifting or bending.
How is pelvic pain diagnosed?
Diagnosing the cause of pelvic pain typically involves:
- Medical History and Physical Examination: Initial evaluation by a healthcare provider.
- Imaging Tests: Ultrasound, CT scans, or MRI to visualize internal structures.
- Laboratory Tests: Blood tests, urine tests, or cultures to check for infections.
- Laparoscopy: A minimally invasive surgical procedure to look inside the pelvic cavity.
How is pelvic pain treated?
Treatment depends on the underlying cause and may include:
- Medications: Pain relievers, antibiotics (for infections), or hormonal treatments.
- Physiotherapy: A pelvic health physiotherapist can help with pelvic pain and related symptoms.
- Surgery: In some cases, surgical intervention may be necessary.
- Lifestyle Changes: Dietary adjustments, stress management, and other modifications.
If you or someone you know is experiencing persistent or severe pelvic pain, it’s important to seek medical attention to determine the underlying cause and appropriate treatment.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Pelvic pain can significantly impact daily life, but targeted physiotherapy can help alleviate discomfort and improve quality of life. If you are looking for professional physiotherapy services to manage pelvic pain, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and personalized treatment plans to support your pelvic health and overall well-being.
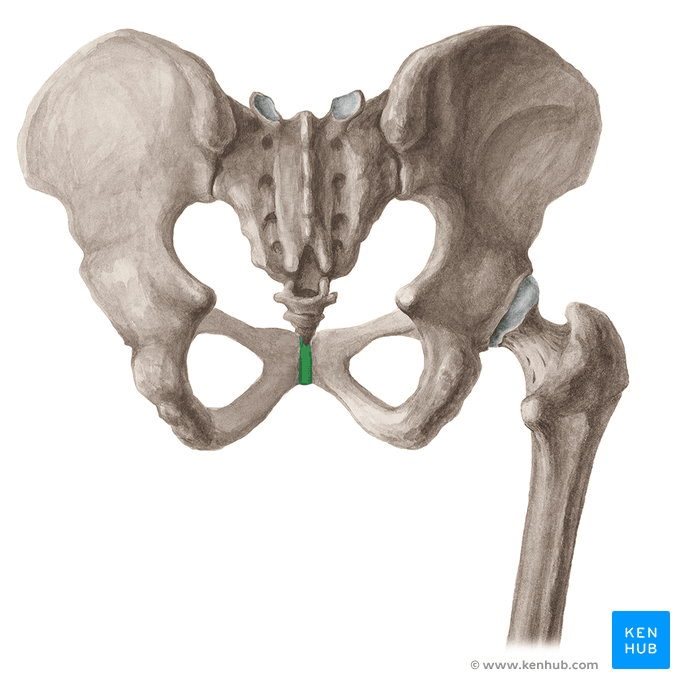
Pubic bone pain after giving birth, also known as postpartum pubic symphysis diastasis or symphysis pubis dysfunction (SPD), is a condition that affects some women following childbirth. This pain is usually centered around the pubic symphysis, the joint at the front of the pelvis where the two halves of the pelvic bone meet.
What are the causes of post-partum pubic bone pain?
- Hormonal Changes: During pregnancy, the body releases the hormone relaxin, which loosens the ligaments in the pelvis to prepare for childbirth. This can sometimes lead to instability or separation of the pubic symphysis.
- Physical Stress: The process of labor and delivery can put significant strain on the pelvic area, particularly if the baby is large, labor is prolonged, or delivery involves interventions such as forceps or vacuum extraction.
- Pre-existing Conditions: Women who had SPD or pelvic girdle pain during pregnancy are more likely to experience pubic bone pain postpartum.
What are the symptoms of symphysis pubis dysfunction (SPD)?
Pain:
- Burning, shooting, grinding or stabbing
- Mild or prolonged
- Usually relieved by rest
- Radiating to the back, abdomen, groin, perineum and legs
- Disappears commonly after giving birth (not in every case)
- Discomfort sense onto the front of the joint
- Clicking of the lower back, hip joints and sacroiliac joints when changing position
- Difficulty in movements like abduction and adduction
Locomotor difficulty:
- Walking
- Ascending or descending stairs
- Rising from a chair
- Weight-bearing activities
- Standing on one leg
- Turning in bed
- Depression, possibly due to the discomfort
How is pubic bone pain treated?
- Rest and Activity Modification: Reducing activities that exacerbate pain, such as standing for long periods, lifting heavy objects, or walking long distances.
- Pelvic Physiotherapy: A physiotherapist can provide exercises to strengthen the pelvic floor, abdominal, and hip muscles, and help stabilize the pelvic area. Manual therapy may also be used to realign the pelvis.
- Pain Relief: Over-the-counter pain medications such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) may be recommended. Always consult with a healthcare provider before taking any medication, especially if breastfeeding.
- Supportive Devices: Wearing a pelvic support belt can help stabilize the pelvis and reduce pain.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce pain and inflammation.
How can a pelvic health physiotherapist help with pubic bone pain?
A pelvic health physiotherapist can be of immense help with symphysis pubis dysfunction (SPD). A pelvic health physiotherapist can provide:
- Guidance on movement techniques for daily activities such as climbing stairs, bending, lifting, and feeding the baby.
- Education on gradually advancing exercises aimed at neuromuscular re-education, core stability, and proper posture.
- Hands-on therapy, including pelvic evaluations and muscle energy techniques to correct pelvic alignment.
- Evaluations to identify tissue dysfunction or lack of coordination.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Recovering from pubic bone pain after giving birth can be supported through targeted physiotherapy. If you’re looking for specialized care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can help you manage pain and regain strength and mobility through personalized treatment plans.
Physiotherapy is a vital field in healthcare. Physiotherapists are healthcare professionals that can help people of all ages live a healthy lifestyle.

Here are seven common myths about physiotherapy debunked:
1. Myth: Physiotherapy is only for injuries.
Reality: While physiotherapy is indeed crucial for injury recovery, it is also beneficial for managing chronic conditions, post-surgical rehabilitation, preventive care, and enhancing athletic performance. Physiotherapists work with patients across various stages of life and health conditions to improve mobility and quality of life.
2. Myth: Physiotherapy is just about exercise.
Reality: Physiotherapy encompasses a wide range of treatments beyond exercises, including manual therapy, electrical stimulation, ultrasound therapy, dry needling, and patient education. These modalities are tailored to address specific conditions and patient needs.
3. Myth: Physiotherapy is painful.
Reality: While some discomfort might be involved, especially when working through injuries or stiffness, physiotherapists aim to minimize pain and improve function. They use techniques that manage pain effectively and strive to make the rehabilitation process as comfortable as possible.
4. Myth: You need a referral to see a physiotherapist.
Reality: In Ontario, you can directly access physiotherapy services without a doctor’s referral. This direct access allows for quicker intervention and treatment, which can be crucial for recovery and pain management. However, you must check with your insurance provider if they need a doctor’s referral to reimburse any treatment fees.
5. Myth: Physiotherapy is only for older people.
Reality: Physiotherapy benefits people of all ages. Children with developmental issues, athletes needing performance enhancement, adults recovering from surgeries, and elderly individuals managing arthritis all benefit from physiotherapy.
6. Myth: Once you start physiotherapy, you’ll need it forever.
Reality: Physiotherapy aims to empower patients with the knowledge and exercises to manage their conditions independently. Many patients achieve their goals and maintain their progress through self-management techniques learned during therapy.
7. Myth: All physiotherapists are the same.
Reality: Physiotherapists specialize in different areas such as sports physiotherapy, pediatric physiotherapy, pelvic health physiotherapy, geriatric physiotherapy, cardiopulmonary physiotherapy, and more. Their training and expertise can vary widely, and it’s essential to find a therapist whose specialization aligns with your specific needs.
Understanding these myths helps in recognizing the comprehensive and essential role of physiotherapy in healthcare, encouraging individuals to join Physiotherapy Oakville for appropriate care and optimal health outcomes.
How do I book an appointment at a Triangle Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Debunking myths about physiotherapy helps more people understand its benefits for pain management and overall health. If you’re looking for reliable physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are qualified physiotherapists available to provide expert care and help you achieve your wellness goals.
It’s great when sex feels natural and pleasurable, but what happens when that stops happening? Let’s dive into a topic that affects many men but is often shrouded in silence: erectile dysfunction (ED). It’s a sensitive subject, but an important one to address. Did you know that your pelvic floor muscles play a significant role in erectile function? In this blog, we’ll explore how the pelvic floor impacts ED and what can be done to restore function and sexual confidence.
What is the pelvic floor?
Picture the pelvic floor as a team of strong muscles located in your pelvic area. These muscles form the base of the pelvis and support your bladder, rectum, and prostate. These muscles can also face challenges in strength, endurance, or overall quality of muscle tone. This can happen for several reasons, but once it occurs the pelvic floor gets used to these patterns. This can be overwhelming and frustrating.
How does the pelvic floor relate to erectile dysfunction?
Well, the pelvic floor muscles are responsible for a range of functions, including blood flow regulation, maintaining erections, and controlling ejaculation. When these muscles become weak or tense, it can lead to difficulties in achieving or sustaining an erection. Imagine as though there is cement in your muscles, it makes them look strong but they’re not actually functional. These tight muscles can prevent arousal and effective orgasms. It takes more than just strengthening to improve the quality of contraction in these muscles. It is important for a strong muscle to be able to relax, as well as contract for optimal function. Pelvic physiotherapy treatment is focused on restoring that function.
How is the pelvic floor strengthened?
The good news is that you have the power to strengthen your pelvic floor muscles and potentially improve erectile function. A start to strengthening can be kegel exercises, however these are not the answer for everyone. Kegels are similar to a bicep contraction, and the strength plateaus if strengthening only involves kegels. True strength will take more than just 100 kegels. It takes functional training and pelvic floor strengthening in different ranges. It also involves strengthening the other muscles in the inner unit such as the deep core, diaphragm, and multifidi.
Relaxation Techniques:
Sometimes, it’s not just about strength but also about letting go of tension. Stress and anxiety can have a significant impact on your sexual performance. Learning relaxation techniques, such as deep breathing exercises and mindfulness, can help release the tension in your pelvic floor muscles and create a more relaxed and conducive environment for sexual experiences. Another powerful tool is learning how to effectively reverse kegel and strengthen the pelvic floor in the lengthened range.
While self-help exercises are a great start, seeking professional guidance from a pelvic floor physiotherapist can take your journey to the next level. These knowledgeable experts can assess your specific situation, provide tailored exercises, and guide you through techniques that target your pelvic floor muscles. They understand the challenges you may face and approach the topic with empathy and professionalism, creating a safe space for discussion.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Improving pelvic floor health can play a significant role in managing erectile dysfunction. If you’re seeking expert guidance, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas can provide personalized care to help you improve pelvic floor function and overall well-being.
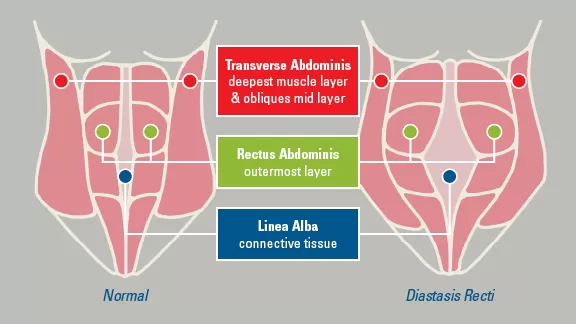
What is Diastasis Recti?
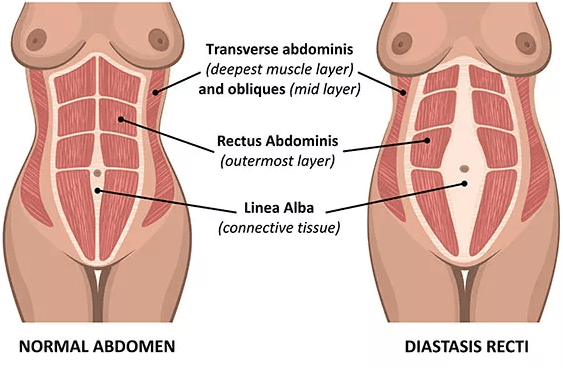
Diastasis recti is a condition where the right and left sides of the rectus abdominis (the “six-pack” muscles) separate, causing a gap in the abdominal wall. This condition is relatively common, especially among pregnant women and newborns, but it can affect individuals of any age or gender.
What are the causes of Diastasis Recti?
Diastasis recti often occurs during pregnancy due to the expanding uterus putting pressure on the abdominal muscles. It can also result from rapid weight gain or loss, improper lifting techniques, excessive abdominal exercises, or genetics.
What are the symptoms of Diastasis Recti?
The most noticeable symptom of diastasis recti is a visible bulge or ridge running down the midline of the abdomen, particularly noticeable when the person tries to sit up or strain. Other symptoms may include lower back pain, poor posture, and difficulty with core strength and stability.
How can it be treated?
Treatment options for diastasis recti may include physical therapy exercises to strengthen the abdominal muscles, wearing an abdominal binder or splint to provide support, and in severe cases, surgery to repair the separated muscles. It’s essential to consult a physiotherapist at Physiotherapy Oakville for personalized advice on treatment options.
Diastasis recti commonly occurs during pregnancy and may persist postpartum. Women who experience diastasis recti after childbirth should consult with a physiotherapist at Physiotherapy Oakville for guidance on safe exercises and techniques to promote healing and recovery. Joining Physiotherapy Oakville can provide you with the expert support needed to effectively manage and overcome diastasis recti.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Managing diastasis recti effectively often involves targeted physiotherapy to strengthen the core and restore function. If you’re looking for specialized care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these locations can provide tailored treatment plans to help you recover and regain strength.
Let’s talk about stretches to do when pregnant. Engaging in stretching exercises during pregnancy can contribute to the elongation of your muscles and overall body flexibility, providing increased comfort whether you’re strolling through the grocery store, engaging in a workout, or simply relaxing. The soothing effects of stretching are particularly helpful during pregnancy, offering significant benefits to your body. Moreover, incorporating stretching into your routine at this stage can aid in preparing your muscles and joints for the challenges of labor in the future.

What are the benefits of stretching during pregnancy?
Stretching during pregnancy can offer several benefits for expectant mothers. However, it’s crucial to consult with a healthcare provider before starting any new exercise routine during pregnancy. Assuming that the healthcare provider gives the green light, here are some potential benefits of stretching during pregnancy:
- Improved Flexibility
- Reduced Muscle Tension
- Enhanced Circulation
- Relief from Discomfort
- Prevention of Muscle Strain
- Promotion of Relaxation
- Preparation for Labor
- Posture Improvement
- Emotional Well-being
- Better Sleep
What can I do to stretch safely when I am pregnant?
- First and foremost, check with your doctor or midwife to ensure that it is safe for your pregnancy.
- Warm-up
- Do gentle and controlled movements
- Avoid over-doing it
- Listen to your body
- Maintain good posture
- Use the right breathing techniques
- Hydrate
What are some of the stretches I can do when pregnant?




Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Performing safe stretches during pregnancy can help manage discomfort and improve flexibility. For personalized prenatal care and guidance, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can create tailored exercise plans to support your comfort and well-being throughout pregnancy.
March 8th marks International Women’s Day and Triangle Physiotherapy is proud to be able to empower women to advocate for themselves and their health needs.
Our goal is to encourage women to focus on their health, both, physical and mental. Build your healthcare team and schedule regular visits, in addition to exercising regularly and eating healthy.
Women’s Health and the Pelvic Floor
Women’s health is intricately connected to the well-being of the pelvic floor, a group of muscles, ligaments, and tissues supporting the uterus, bladder, and rectum. Maintaining a healthy pelvic floor is crucial for various functions, including urinary and bowel control, sexual function, and providing support during pregnancy. Pregnancy, childbirth, hormonal changes, and aging can impact the pelvic floor, leading to issues like incontinence, pelvic organ prolapse, and sexual dysfunction.
Maintaining a healthy lifestyle, proper posture, and seeking guidance from a pelvic health physiotherapist are essential for women’s pelvic floor health. Awareness and proactive care contribute to overall well-being, enabling women to lead active and fulfilling lives while addressing potential pelvic floor challenges.
What are the symptoms of Pelvic Floor Dysfunction?
Pelvic Floor Dysfunction (PFD) can manifest through various symptoms, which may vary in intensity and duration. Common signs of PFD include:
- Urinary Issues:
- Urinary incontinence: Involuntary leakage of urine.
- Frequent urination: The need to urinate more often than usual.
- Difficulty emptying the bladder: Struggling to fully release urine.
- Bowel Issues:
- Constipation: Difficulty passing stools or infrequent bowel movements.
- Straining during bowel movements: Experiencing difficulty while trying to have a bowel movement.
- Pelvic Pain:
- Pelvic pain or discomfort: Discomfort in the pelvic region, which may be persistent or intermittent.
- Pain during sexual intercourse: Discomfort or pain during sexual activity.
- Muscle Tension:
- Tight or spasming pelvic muscles: Increased muscle tension in the pelvic floor.
- Pelvic Organ Prolapse:
- The feeling of pressure or fullness in the pelvic area: Sensation of something bulging or descending into the vagina.
- Lower Back Pain:
- Chronic lower back pain: Discomfort or pain in the lower back region.
- Changes in Posture:
- Altered posture: Changes in the alignment of the spine and pelvis.
How a Pelvic Health Physiotherapist can help and what to expect?
A Pelvic Health Physiotherapist specializes in assessing and treating conditions related to the pelvic floor and surrounding areas. Here’s how they can help and what to expect during a session:
- Assessment:
- A thorough assessment of your medical history, pelvic health, and relevant symptoms.
- Physical examination, which may include internal and external assessments to evaluate the strength, flexibility, and coordination of the pelvic floor muscles.
- Education:
- Detailed explanation of pelvic anatomy and the role of pelvic floor muscles in various functions.
- Guidance on lifestyle factors, posture, and habits that may contribute to pelvic health issues.
- Pelvic Floor Exercises:
- Prescribing personalized pelvic floor exercises, to strengthen or relax specific muscles based on the assessment findings.
- Teaching proper technique and ensuring exercises are performed correctly.
- Manual Therapy:
- Hands-on techniques to release tension in the pelvic floor muscles or surrounding tissues.
- Myofascial release and trigger point therapy to address muscle knots or tightness.
- Biofeedback:
- Using biofeedback tools to provide real-time information about pelvic floor muscle activity.
- Assisting individuals in learning how to control and coordinate their pelvic floor muscles.
- Behavioral Strategies:
- Implementing behavioral strategies for managing and improving bladder and bowel function.
- Developing strategies for optimizing pelvic health during daily activities.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
On International Women’s Day, let’s celebrate the strength and resilience of women everywhere. For those seeking expert support for their health and wellness, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas are committed to empowering women through personalized care and treatment plans.
When we think about pelvic health, we often think of women’s issues, but did you know that men also have a pelvic floor? That’s right! The male pelvic floor is a group of muscles that support the bladder, bowel, and sexual organs.
However, just like any other muscle group, the male pelvic floor can become weakened or tense, leading to a variety of issues. For example, pelvic pain, urinary or fecal incontinence, and erectile dysfunction can all be caused by pelvic floor dysfunction.

What are the Causes of Pelvic Floor Dysfunction in Men?
When we think about pelvic health, we often think of women’s issues, but did you know that men also have a pelvic floor? That’s right! The male pelvic floor is a group of muscles that support the bladder, bowel, and sexual organs.
However, just like any other muscle group, the male pelvic floor can become weakened or tense, leading to a variety of issues. For example, pelvic pain, urinary or fecal incontinence, and erectile dysfunction can all be caused by pelvic floor dysfunction.
The pelvic floor conditions we see in men are:
- Post-Prostatectomy Incontinence
- Post-prostatectomy Erectile dysfunction
- Pelvic Pain – Testicular & Penile pain, Chronic Prostatitis
How is Pelvic Floor Dysfunction diagnosed in Men?
Once you come in for an initial assessment, a qualified pelvic health physiotherapist will begin by taking a detailed medical history and a review of your symptoms, followed by an assessment of your symptoms and pelvis.
Once the cause of your pain or dysfunction has been diagnosed, your pelvic health physiotherapist will discuss the findings with you, as well as explain treatment options and expected outcomes.
What to Expect During Pelvic Floor Physiotherapy for Men?
Your pelvic floor physiotherapist will design an individual treatment plan that would aim to meet your goals, which may include one or more of the following; pelvic floor and pelvic muscle exercises, education, mindfulness and relaxation techniques, and bladder and bowel training.
Where can I find a men’s pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Pelvic Health physiotherapists advocate the importance of educating individuals about their pelvic health. They are often asked by patients if an internal exam is necessary. Many patients refrain from seeking help for pelvic health issues because of the fear of internal examination. While internal exams are not a must, they can be very helpful to pelvic health physiotherapists in determining the condition of the pelvic floor.
What is an Internal Pelvic Exam?
A pelvic floor assessment, which may or may not include an internal pelvic exam, entails a pelvic health physiotherapist examining the pelvic floor muscles, tissues, and organs by inserting a gloved hand into the vagina or rectum. This examination is crucial for assessing the well-being and performance of the pelvic floor, allowing for the detection of any possible problems or issues.
Why is an internal pelvic exam important?
- Detailed Assessment of Pelvic Floor Muscles: An internal pelvic exam allows the physiotherapist to assess the tone, strength, flexibility, and coordination of the pelvic floor muscles. This information is crucial in developing an accurate understanding of the patient’s pelvic health.
- Identification of Muscle Imbalances: Through internal palpation, a physiotherapist can identify any muscle imbalances or asymmetries in the pelvic floor. This helps in tailoring the treatment plan to address specific issues, such as hypertonic (overactive) or hypotonic (underactive) muscles.
- Assessment of Pelvic Organ Function: Internal examination enables the physiotherapist to assess the function of pelvic organs, such as the bladder, uterus, and rectum. This is important in cases where dysfunction or weakness in the pelvic floor muscles may be contributing to issues such as urinary incontinence or pelvic organ prolapse.
- Evaluation of Connective Tissues and Nerves: The internal exam allows the physiotherapist to assess the condition of connective tissues, ligaments, and nerves in the pelvic region. Dysfunction in these structures can contribute to pelvic pain and other symptoms, and the internal exam helps in identifying such issues.
- Assessment of Trigger Points and Tenderness: The physiotherapist can identify trigger points and areas of tenderness within the pelvic floor muscles. This information is crucial in designing a targeted treatment plan, which may include manual therapy techniques to release muscle tension.
- Feedback on Exercise Performance: During an internal pelvic exam, the physiotherapist may guide the patient through specific exercises to assess the effectiveness of pelvic floor muscle contractions. Real-time feedback helps the patient learn proper muscle engagement and control.
- Patient Education and Empowerment: The internal exam provides an opportunity for the physiotherapist to educate the patient about their pelvic floor anatomy, function, and any specific issues identified during the assessment. This empowers the patient to actively participate in their treatment plan and make lifestyle changes that support pelvic health.

Do I have to have an internal exam during a pelvic health assessment?
It’s important to note that internal pelvic exams are conducted with the patient’s informed consent, and physiotherapists ensure a comfortable and respectful environment during the assessment. The goal is to provide comprehensive care and address the specific needs of individuals experiencing pelvic health issues. That being said, if you are not comfortable being internally examined, please let your physiotherapist know before the start of your assessment.
How do I prepare for an internal pelvic exam?
Preparing for an internal pelvic exam involves a combination of physical and mental preparation. It’s essential to communicate openly with your pelvic health physiotherapist and follow their instructions. Here are some general guidelines to help you prepare:
Comfortable Clothing: Wear comfortable, easy-to-remove clothing. You may be asked to undress from the waist down, so wearing a skirt or loose pants can be convenient.
Relaxation Techniques: Practice relaxation techniques such as deep breathing to help ease anxiety and tension. Relaxing your pelvic muscles can make the exam more comfortable.
Communicate with your Physiotherapist: Inform your pelvic health physiotherapist about any concerns, fears, or past traumatic experiences related to pelvic exams. They can adjust their approach and provide additional support.
Ask Questions: Feel free to ask any questions you may have about the procedure. Knowing what to expect can help alleviate anxiety.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Understanding the need for an internal exam during a pelvic health assessment can help you make informed decisions about your care. If you’re looking for specialized support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can provide comprehensive pelvic health assessments tailored to your comfort and needs.