Your pelvic floor may be out of sight, but its health plays a central role in how you move, feel, and live every day. From bladder control to core stability and postpartum recovery, pelvic health issues can affect all genders and age groups – often silently.
At Triangle Physiotherapy North York, we offer compassionate, specialized care for individuals experiencing pelvic floor dysfunction. Our goal is simple: help you understand what’s happening in your body, create a path toward recovery, and give you the tools to regain confidence in your daily life.
Signs It’s Time to See a Pelvic Health Physiotherapist
Pelvic health symptoms often get dismissed or misunderstood. But if left untreated, they can affect everything from your mobility to mental wellbeing. Here’s when you should consider seeing a pelvic physiotherapist:
- Ongoing pelvic pain or pressure
- Leaking urine when sneezing, laughing, or exercising
- Discomfort during sexual activity
- Constipation or painful bowel movements
- Difficulty resuming exercise after pregnancy or surgery
- A feeling of heaviness or instability in the hips or core
These symptoms are common, but they’re not normal. The earlier you address them, the more effective your treatment can be.
How Pelvic Physiotherapy Helps You Heal
At Triangle Physiotherapy North York, we take a whole-person approach. We look beyond just the symptoms and focus on recovery goals that matter to you – whether that’s returning to sport, managing chronic conditions, or simply feeling at ease in your body.
Here’s what our pelvic health treatments may include:
- Targeted pelvic floor exercises to build strength and control
- Manual therapy to reduce muscle tension or overactivity
- Education on movement, posture, and daily habits that support healing
- Breath and core coordination training for long-term stability
- Postpartum and post-surgical support tailored to your unique timeline
You’ll leave each session not just with progress, but with understanding – so you feel empowered between visits, too.
Why Choose Triangle Physiotherapy North York?

We know it’s not always easy to talk about pelvic health. That’s why our team creates a safe, welcoming environment where your questions are heard and your privacy respected.
Here’s what you can expect:
- One-on-one sessions in private rooms
- Experienced clinicians with advanced training in pelvic health
- Flexible hours including evenings and weekends
- Direct billing to most insurance providers
- A personalized treatment plan that evolves with your recovery
Our North York clinic is committed to making high-quality pelvic physiotherapy accessible, effective, and grounded in education.
Take the First Step Toward Lasting Relief
Whether you’re navigating postpartum recovery, managing chronic discomfort, or simply want to better understand your body – Triangle Physiotherapy North York is here to help. You deserve care that not only treats symptoms, but supports your journey toward lifelong pelvic health. Book your assessment today, and let’s start building your recovery plan – together.
As we age, staying active and maintaining independence becomes more important than ever. However, many seniors face challenges with mobility, balance, and everyday tasks that were once simple to perform. Whether it’s walking, climbing stairs, or even standing up from a chair, these activities can become increasingly difficult without the right care. At Triangle Physiotherapy North York, we provide specialized physiotherapy services tailored to seniors to improve movement, restore balance, and promote an active lifestyle.
Why Physiotherapy is Essential for Seniors
Aging naturally brings changes to our bodies, including reduced joint flexibility, weaker muscles, and slower reflexes. These changes can lead to decreased mobility and an increased risk of falls. Physiotherapy for seniors focuses on restoring function, increasing strength, and enhancing stability, which are essential for preserving independence and overall well-being.
At Triangle Physiotherapy North York, we offer targeted treatments to help address these age-related changes. Our expert physiotherapists create personalized rehabilitation plans focused on improving posture, mobility, strength, and balance, while also emphasizing fall prevention. We aim to not only address existing conditions but also help prevent future complications, allowing our senior patients to live with greater confidence and freedom.
Why Triangle Physiotherapy North York is the Right Choice for Seniors

Selecting the right clinic for physiotherapy is critical, particularly for seniors who may have unique health concerns. Here’s what makes Triangle Physiotherapy North York stand out as the ideal choice for senior rehabilitation:
1. Customized Treatment Plans for Every Individual
Each senior has different health needs. Whether you’re dealing with osteoarthritis, recovering from surgery, or simply experiencing stiffness from aging, our physiotherapists take the time to understand your condition and create a rehabilitation plan that’s specifically tailored to you.
At Triangle Physiotherapy North York, we offer services ranging from mobility exercises and manual therapy to strength-building activities and postural training. Our aim is to help seniors regain independence and enjoy a better quality of life by providing care that’s specifically aligned with their goals.
2. Expertise in Senior Health and Recovery
Our physiotherapists are skilled in treating conditions commonly associated with aging. With years of experience in senior care, we understand the physical challenges that come with age and use proven methods to address them. Whether through joint mobilization, strength training, or balance improvement techniques, our focus is on helping you recover safely and effectively.
The Triangle team is dedicated to offering the most up-to-date treatments, all while ensuring your comfort and safety throughout your recovery.
3. A Compassionate and Welcoming Clinic Atmosphere
The right environment is crucial for effective recovery. At Triangle Physiotherapy North York, we’ve designed our clinic to be a warm and supportive space where seniors feel comfortable and at ease. From your initial consultation to your final treatment session, our staff is here to guide and support you every step of the way.
Our physiotherapists create a collaborative, encouraging environment that fosters trust and empowers seniors to take control of their rehabilitation journey.
Key Advantages of Senior Physiotherapy at Triangle Physiotherapy North York
- Improved Stability and Balance: We use balance training techniques to reduce the risk of falls, an essential part of maintaining independence for seniors.
- Enhanced Range of Motion: Through targeted stretching and strengthening exercises, we help restore flexibility and movement, enabling seniors to carry out daily activities with greater ease.
- Pain Management: Our physiotherapists specialize in alleviating discomfort caused by arthritis, muscle tension, and other age-related conditions, promoting pain relief and improved function.
Take the First Step Towards Better Mobility
At Triangle Physiotherapy North York, we believe that aging doesn’t have to mean sacrificing mobility or independence. With the right physiotherapy treatment, seniors can maintain an active and fulfilling life. Our experienced team is committed to improving your physical health and helping you stay independent. If you or someone you know is looking for dedicated, expert care, book a consultation with us today and take the first step toward a healthier, more mobile future.
Breastfeeding can be a fulfilling and bonding experience, but it sometimes comes with challenges such as mastitis and blocked milk ducts. These conditions can be painful and stressful for new mothers, but understanding and managing them can significantly improve your breastfeeding journey. In this blog, we’ll explore what mastitis and blocked milk ducts are, their symptoms, causes, and how physiotherapy, particularly in the pelvic health domain, can help. This information is especially valuable for mothers in North York looking for local resources and support.
What is Mastitis?
Mastitis is an inflammation of breast tissue that often involves an infection. This condition can cause breast pain, swelling, warmth, and redness. In some cases, mothers might experience fever and chills. It typically occurs in breastfeeding women when milk ducts become blocked or when bacteria enter the breast through a cracked nipple.

Symptoms of Mastitis
Common symptoms of mastitis include:
- Breast pain or tenderness
- Swelling and warmth in the affected area
- Redness, often in a wedge-shaped pattern
- Fever and chills
- Fatigue
Causes of Mastitis
Mastitis is often caused by:
- Blocked milk ducts: When milk isn’t fully drained from the breast, it can cause a blockage, leading to inflammation.
- Bacterial infection: Bacteria from the baby’s mouth or the mother’s skin can enter the breast through a cracked nipple.
Understanding Blocked Milk Ducts
Blocked milk ducts are a common issue for breastfeeding mothers. When a duct is blocked, it prevents the milk from flowing freely through the breast, leading to a backup of milk and potential inflammation.
Symptoms of Blocked Milk Ducts
- A small, hard lump in the breast that may be tender to the touch
- Discomfort or pain in one area of the breast
- A decrease in milk supply from the affected breast
- Milk blebs or blisters on the nipple
Causes of Blocked Milk Ducts
- Infrequent breastfeeding or pumping
- Poor latch or ineffective sucking by the baby
- Pressure on the breast from tight clothing or a poorly fitting bra
- Stress and fatigue
How Physiotherapy Can Help
Physiotherapy can be an effective treatment for mastitis and blocked milk ducts. Specialized techniques used by physiotherapists in the pelvic health domain can alleviate symptoms and prevent recurrence. Here are some ways physiotherapy can help:
Therapeutic Ultrasound
Therapeutic ultrasound is a non-invasive treatment that uses sound waves to reduce inflammation and pain. It can help to clear blocked ducts and promote milk flow.
Breast Massage Techniques
Our Physiotherapists in North York can teach you proper breast massage techniques to relieve blocked ducts. This includes:
- Gentle circular motions around the lump
- Moving the lump towards the nipple
- Massage before and during breastfeeding to aid milk flow
Education and Support
Our Physiotherapists in North York provide education on proper breastfeeding techniques, ensuring a good latch and advising on optimal breastfeeding positions. They also offer support and strategies to manage stress and fatigue, which are crucial for overall well-being.
Local Resources in North York
For mothers in North York, Triangle Physiotherapy North York specializes in pelvic health and offers targeted treatments for breastfeeding-related issues. Our clinic provides a supportive environment where mothers can receive personalized care and practical advice.
Prevention Tips
Preventing mastitis and blocked milk ducts involves:
- Frequent breastfeeding or pumping to keep the milk flowing
- Ensuring the baby has a good latch
- Varying breastfeeding positions
- Wearing loose-fitting, comfortable bras
- Staying hydrated and maintaining a balanced diet
Mastitis and blocked milk ducts can be challenging, but with the right understanding and support, they are manageable. Physiotherapy offers effective treatments and strategies to help mothers overcome these issues and continue their breastfeeding journey with confidence. If you’re in North York and experiencing breastfeeding challenges, consider reaching out to a local pelvic health physiotherapist for specialized care.
For more information or to book an appointment, contact our clinic today and take the first step towards a pain-free breastfeeding experience.
“For those dealing with mastitis or blocked milk ducts, Triangle Physiotherapy provides expert care across various locations including Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village.”
Managing mastitis and blocked milk ducts can be challenging, but with the right care, recovery is possible. For comprehensive support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Skilled physiotherapists in these areas can help you manage symptoms effectively and promote healing.
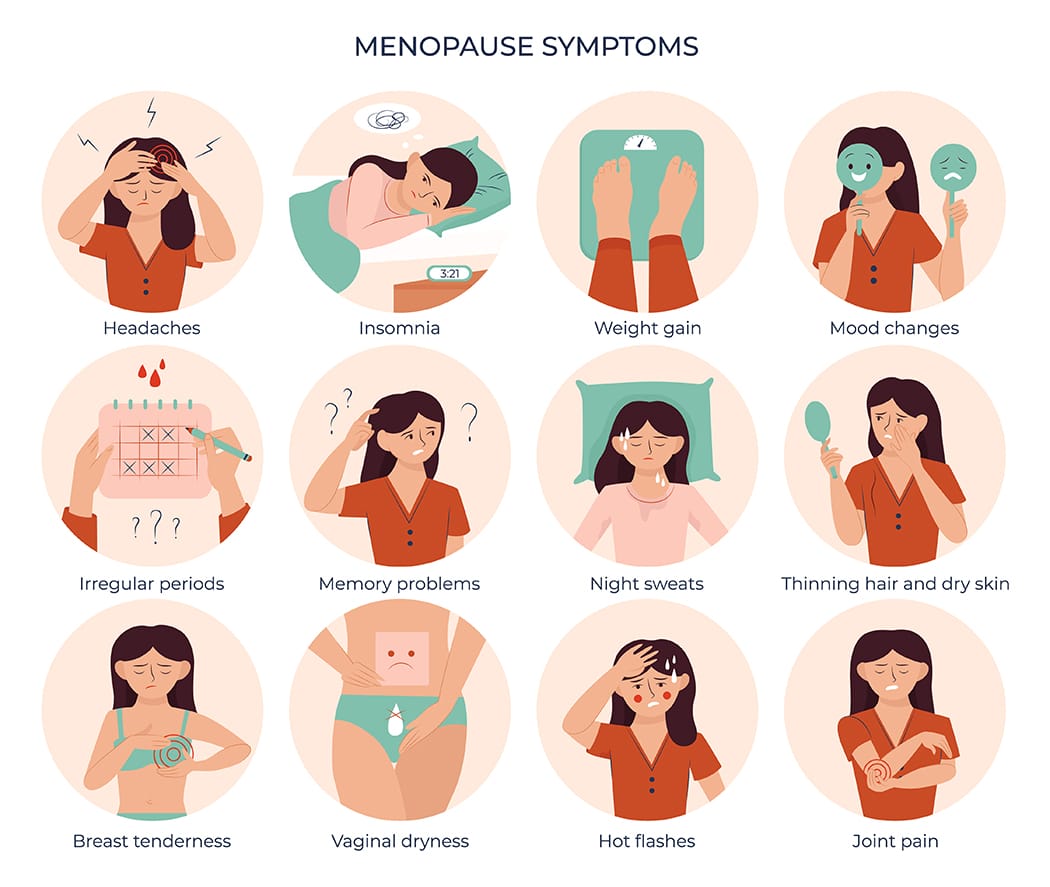
Vaginal atrophy, also known as atrophic vaginitis, is a condition that many women experience, especially after menopause. It involves changes in the vaginal area that can cause discomfort and other symptoms. Fortunately, our pelvic health physiotherapists in North York can help manage these symptoms and improve your quality of life.
What is Vaginal Atrophy?
Vaginal atrophy often happens during menopause when the levels of estrogen, a hormone in a woman’s body, decrease. When this happens, it can lead to:
- Dryness: The vagina becomes less moist, leading to dryness and irritation.
- Thinning of Vaginal Walls: The walls of the vagina become thinner and less flexible.
- Inflammation and Redness: The vaginal area can become inflamed and red, causing pain.
- Urinary Symptoms: You might experience more frequent urination, a strong urge to urinate, or urinary tract infections (UTIs).
These changes can make everyday activities uncomfortable and affect your sex life.
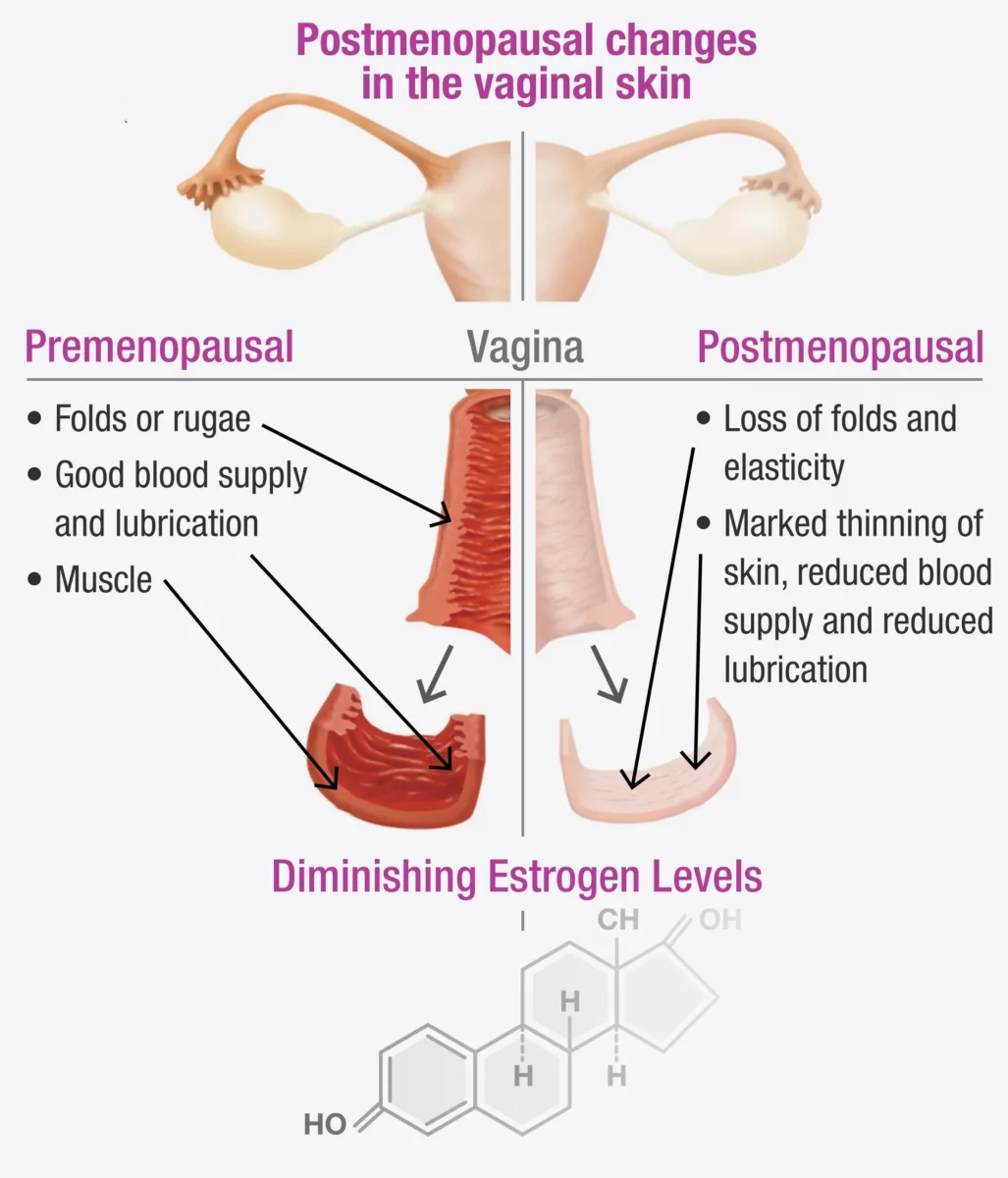
If vaginal atrophy is not treated and a woman continues to experience painful intercourse, the vaginal muscles may react by tightening to protect the body. Over time, this tightening can become an automatic response (vaginismus) that continues even after the atrophy has been treated.
Fortunately, both conditions can be treated with the help of a pelvic health Physiotherapist in North York. In fact, it is often necessary to treat vaginal atrophy and vaginismus together, as addressing one without the other can be challenging.
Symptoms to Watch For
You might have vaginal atrophy if you notice:
- Pain During Sex: Painful intercourse (called dyspareunia) is a common symptom.
- Itching or Burning: These sensations can be uncomfortable and persistent.
- Frequent UTIs: More urinary tract infections than usual.
- Vaginal Bleeding or Discharge: Unusual bleeding or discharge can occur.
- Difficulty Urinating: Problems with urination, such as a strong urge or pain.
Recognizing these symptoms early can help you get the treatment you need sooner.
How a Pelvic Health Physiotherapist Can Help with Menopause and Vaginal Atrophy
A pelvic health physiotherapist is a specialist who focuses on the muscles and tissues in the pelvic area. They can provide various treatments to help manage vaginal atrophy. Here’s how they can assist:
1. Assessment and Diagnosis
The first step is a thorough check-up, which includes:
- Reviewing Your Medical History: Discussing your symptoms, medical history, and any medications you are taking.
- Physical Examination: Checking the condition of your vaginal walls, pelvic floor muscles, and surrounding tissues.
2. Customized Exercise Programs
These physiotherapists create specific exercise programs to strengthen and relax your pelvic floor muscles. These exercises can:
- Improve Muscle Tone: Making the vaginal muscles stronger and more flexible.
- Boost Blood Flow: Increasing circulation to help with healing and tissue health.
3. Manual Therapy and Techniques
Hands-on techniques are used to improve the flexibility and function of your pelvic area, such as:
- Myofascial Release: Reducing tension in the pelvic muscles.
- Scar Tissue Mobilization: Addressing any scarring or adhesions in the vaginal area.
4. Education and Lifestyle Advice for Menopause
Education is a key part of therapy, including advice on:
- Diet and Hydration: Eating a balanced diet and staying hydrated for overall health.
- Relaxation Techniques: Learning how to relax your pelvic floor muscles to reduce discomfort.
5. Use of Devices and Modalities
They might suggest using certain devices and techniques, such as:
- Vaginal Dilators: These help gently stretch the vaginal walls, making them more flexible.
- Electrostimulation: Using mild electrical impulses to strengthen pelvic muscles.
How do I find a pelvic health physiotherapist in North York?
We have 8 locations with pelvic health physiotherapists to help you. If you are going through menopause and are seeing signs of vaginal atrophy, Book an Appointment today!
Pelvic Health Physiotherapists in North York:
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
At Triangle Physiotherapy, we understand that conditions like menopause and vaginal atrophy can significantly impact your quality of life. Our team of experienced professionals is here to help you through specialized physiotherapy treatments designed to address these and other related concerns. Whether you’re seeking Physiotherapy in Etobicoke, Physiotherapy in Oakville, Physiotherapy in North York, or Physiotherapy in Toronto, we have clinics conveniently located across the region. Visit us at Physiotherapy Lawrence Park, Physiotherapy Clinic Queens Quay, Physiotherapy Erin Mills, Physiotherapy Mississauga, or Physiotherapy Liberty Village to start your journey towards better health and well-being.
Spinal fusion surgery is a medical procedure used to permanently join two or more vertebrae in the spine, eliminating motion between them. The goal of the surgery is to reduce pain, correct deformities, or improve stability in the spine.
When would I need Spinal Fusion Surgery?
Spinal fusion surgery is typically recommended for various spine conditions, including:
- Degenerative disc disease: When the discs between vertebrae break down, causing pain.
- Spondylolisthesis: When one vertebra slips forward over the one below it.
- Spinal stenosis: Narrowing of the spinal canal, leading to nerve compression.
- Scoliosis: Abnormal curvature of the spine.
- Fractures: Vertebrae that are broken or dislocated.
- Tumors: Removal of tumors that affect spinal stability.
- Infections: Infections that have caused damage to the vertebrae.
When do I start physiotherapy after surgery?
The timing of when to start physiotherapy after spinal fusion surgery depends on several factors, including the specifics of the surgery, the patient’s overall health, and the surgeon’s recommendations.
What does post-surgery rehab involve?
Immediate Postoperative Period (0-6 Weeks)
- Initial Phase: Physiotherapy may start in the hospital within a day or two after surgery. The focus is on gentle movements and exercises to improve circulation and prevent complications.
- Activities:
- Breathing exercises to prevent lung complications.
- Gentle leg movements like ankle pumps to improve blood flow.
- Log rolling technique for safe movement in and out of bed.
- Short, frequent walks to promote circulation and reduce stiffness.
Early Rehabilitation Phase (6-12 Weeks)
- When: Typically, more structured physical therapy begins around 4 to 6 weeks after surgery, depending on the surgeon’s assessment.
- Goals: Gradually increase mobility, start gentle strengthening exercises, and improve functional movements.
- Activities:
- Range of motion exercises.
- Gentle strengthening exercises for the core and lower extremities.
- Walking programs to gradually increase distance and duration.
- Education on proper body mechanics and posture.
Late Rehabilitation Phase (3-6 Months)
- When: Around 3 months post-surgery, assuming there are no complications.
- Goals: Restore full function, enhance strength and endurance, and improve posture and body mechanics.
- Activities:
- More advanced strengthening exercises using resistance bands or light weights.
- Low-impact aerobic exercises like swimming or cycling.
- Balance and coordination exercises.
- Functional training for daily activities.
Long-Term Rehabilitation Phase (6-12 Months)
- When: After 6 months, the patient should continue with physiotherapy based on individual progress and goals.
- Goals: Achieve optimal strength, flexibility, and functional ability, and prevent recurrence of symptoms.
- Activities:
- Progressive resistance training.
- Gradual reintroduction of higher-impact activities, if appropriate.
- Sport-specific training for athletes.
- Ongoing education on maintaining spine health.
Key Points to Consider
- Surgeon’s Recommendations: Always follow the specific guidelines and timelines provided by the surgeon, as they know the details of the surgery and individual patient needs.
- Listen to Your Body: Avoid pushing through pain. Pain is a signal that something might be wrong, and it’s important to communicate any discomfort to the physiotherapist or surgeon.
- Individual Variation: Each patient’s recovery is unique. Factors such as age, overall health, and the complexity of the surgery will influence the timing and intensity of physiotherapy.
Starting physiotherapy at the right time is crucial for a successful recovery, and adhering to a structured rehabilitation program can significantly enhance outcomes after spinal fusion surgery.
Click here to book an appointment for post-surgery rehab with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
General Information: The information provided on this blog is for general informational purposes only. While we strive to ensure the accuracy and relevance of our content, we make no guarantees about the completeness, reliability, or accuracy of the information.
Not Professional Advice: The content on this blog does not constitute professional advice. It is not a substitute for professional medical, legal, financial, or other professional advice. Always seek the guidance of a qualified professional with any questions you may have regarding your specific situation.
Recovering from spinal fusion surgery requires careful physiotherapy to restore mobility and strength. Whether you need physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are expert physiotherapists available to guide your recovery journey and help you regain your quality of life.
Hiking is a fantastic way to enjoy the great outdoors and stay fit, but it can also pose some risks. Whether you’re new to hiking or a seasoned backpacker, there are numerous factors to take into account before heading out on the trails. You need to evaluate your backpack’s weight, choose appropriate footwear, plan your food and hydration, check the weather, and map out your routes. Additionally, since hiking often takes you off the beaten path, it’s essential to take precautions against three common hiking injuries: knee pain, ankle sprains, and sore feet.
Is it necessary to warm up before hiking?
Yes, it is necessary to warm up before hiking. Warming up helps prepare your muscles and joints for physical activity, reducing the risk of injury. Here are some reasons why warming up is important before hiking:
Benefits of Warming Up Before Hiking
- Increases Blood Flow: A proper warm-up increases blood flow to your muscles, delivering oxygen and nutrients that help them perform better.
- Enhances Flexibility: Warming up loosens your muscles and increases your range of motion, making it easier to navigate uneven terrain.
- Reduces Injury Risk: Warm muscles are less prone to strains, sprains, and other injuries.
- Prepares Your Heart: Gradually increasing your heart rate helps prepare your cardiovascular system for the more strenuous activity of hiking.
- Improves Performance: A good warm-up can improve your overall performance, making your hike more enjoyable and less exhausting.
What are some effective warm up exercises to do before hiking?
Effective Warm-Up Exercises
- Walking or Light Jogging: Start with 5-10 minutes of brisk walking or light jogging to get your blood flowing.
- Dynamic Stretches: Perform dynamic stretches like leg swings, arm circles, and torso twists to loosen up your muscles and joints.
- Ankle Rotations: Rotate your ankles in circles to prepare them for the uneven terrain.
- Hip Circles: Rotate your hips to loosen the hip joints, which are crucial for hiking.
- Calf Raises: Perform calf raises to warm up your calves, which are heavily used during hiking.
Taking a few minutes to warm up before you start your hike can make a significant difference in your overall hiking experience and help prevent injuries.
What are the most common hiking injuries?
Some of the most common hiking injuries are:
- Knee Pain
- Ankle Sprain
- Foot Pain
Knee Pain when Hiking
Knee pain is a common issue among hikers, especially on longer or more challenging trails. Here’s a comprehensive approach to understanding, preventing, and managing knee pain when hiking:
Causes of Knee Pain While Hiking
- Overuse and Strain: Continuous stress on the knee joint from uphill climbs, downhill descents, or long sessions of hiking.
- Improper Biomechanics: Poor hiking technique, such as improper foot placement or stride, can strain the knee joint.
- Previous Injuries: Past knee injuries or conditions like arthritis can flare up during hiking.
- Improper Gear: Worn-out or inappropriate footwear lacking proper cushioning and support.
Ankle Sprain when Hiking
An ankle sprain can be a painful and frustrating injury, especially when hiking in rugged terrain. Here’s how to understand, prevent, and manage ankle sprains while hiking:
Causes of Ankle Sprains While Hiking
- Uneven Terrain: Stepping on uneven surfaces, rocks, or roots can twist or roll the ankle.
- Fatigue: Muscles that support the ankle can become tired, leading to less stability and increased risk of injury.
- Inadequate Footwear: Wearing shoes or boots without proper ankle support or that are worn out.
Foot Pain when Hiking
Foot pain while hiking can be uncomfortable and distracting. Here’s how to understand, prevent, and manage foot pain effectively:
Causes of Foot Pain While Hiking
- Improper Footwear: Shoes or boots that are too tight, loose, worn out, or lacking proper cushioning and support.
- Overuse or Strain: Prolonged walking or hiking, especially on challenging terrain, can strain the muscles and joints of the feet.
- Blisters: Friction from improperly fitting shoes or moisture buildup can lead to painful blisters.
If you get injured while hiking, consult one of our physiotherapists who can help you with treating the injuries as well as advise and educate you on prevention so you can enjoy your outdoor activities without pain and discomfort.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
A rotator cuff tears are common injuries to the shoulder, involving a tear in one or more of the tendons of the rotator cuff muscles. It is one of the leading causes of shoulder pain and disability. The rotator cuff is a group of four muscles and their tendons that stabilize the shoulder and allow for its wide range of motion.
Understanding Rotator Cuff Tears: Causes and Symptoms
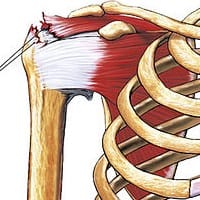
The rotator cuff is a group of four muscles and their tendons that stabilize the shoulder and allow for its wide range of motion. These muscles are:
- Supraspinatus
- Infraspinatus
- Teres minor
- Subscapularis
Types of Rotator Cuff Tears
- Partial Tear: This type of tear damages the tendon but does not completely sever it.
- Complete Tear: Also known as a full-thickness tear, this type involves the tendon being split into two pieces or pulled completely off the bone.
Causes
- Acute Injury: Sudden injuries, such as a fall on an outstretched arm or lifting something heavy with a jerking motion.
- Degenerative Wear and Tear: Gradual wear over time due to aging, repetitive stress from activities (like sports or certain jobs), or poor shoulder mechanics.
Symptoms
- Pain at rest and at night, particularly if lying on the affected shoulder
- Pain when lifting and lowering your arm or with specific movements
- Weakness in the shoulder
- Crackling sensation when moving the shoulder in certain positions
Importance of Physiotherapy in Rotator Cuff Tear Treatment
Physiotherapy plays a crucial role in the treatment and rehabilitation of rotator cuff tears. It can help in several ways, whether as a primary treatment for less severe tears or as a post-surgical rehabilitation strategy for more significant injuries. Here are some key points highlighting the importance of physiotherapy in rotator cuff tear treatment:
Pain Reduction
- Manual Therapy: Techniques such as massage and joint mobilization can help reduce pain and improve shoulder function.
- Modalities: Use of heat, ice, ultrasound, and electrical stimulation can help manage pain and inflammation.
Restoring Range of Motion
- Stretching Exercises: Specific stretches help maintain and gradually improve shoulder flexibility.
- Mobilization Techniques: Gentle mobilization can help increase the range of motion without causing further injury.
Strengthening Shoulder Muscles
- Strengthening Exercises: Focused on the rotator cuff and surrounding muscles, these exercises help restore strength and function to the shoulder.
- Progressive Resistance: Gradual increase in resistance helps to build muscle strength over time.
Improving Shoulder Stability
- Proprioceptive Training: Exercises that improve the body’s ability to sense the position and movement of the shoulder, enhancing stability.
- Functional Training: Exercises tailored to improve stability during daily activities and specific movements required in sports or work.
Enhancing Surgical Outcomes
- Pre-Surgical Physiotherapy (“Prehabilitation”): Strengthening and conditioning the shoulder before surgery can lead to better post-surgical outcomes.
- Post-Surgical Rehabilitation: Structured physiotherapy is essential to restore function, strength, and range of motion after surgery. It also helps minimize scar tissue formation and adhesions.
Preventing Further Injury
- Education: Teaching proper shoulder mechanics and ergonomic principles to avoid movements that can exacerbate the injury.
- Exercise Regimen: Developing a long-term exercise plan to maintain shoulder health and prevent future injuries.
Tailored Rehabilitation Programs
- Individualized Plans: Physiotherapists create personalized treatment plans based on the specific nature of the tear, the patient’s overall health, and their functional goals.
- Goal Setting: Setting realistic and progressive goals to keep the patient motivated and track progress.
Long-Term Shoulder Health
- Maintenance Exercises: Developing a routine of exercises to be continued even after formal physiotherapy ends to maintain shoulder health.
- Lifestyle Modifications: Advice on modifications to daily activities and sports techniques to protect the shoulder.
In summary, physiotherapy is an integral part of the comprehensive management of rotator cuff tears, offering a non-invasive approach to pain relief, functional restoration, and long-term shoulder health. It provides a structured and supportive environment for recovery, whether used alone or in conjunction with surgical treatments.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Rotator cuff tears require expert treatment and rehabilitation to restore function and reduce pain. Triangle Physiotherapy offers specialized care across the GTA. Whether you’re seeking Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, our experienced team is here to help you on your recovery journey.”
The choice between physiotherapy and massage therapy depends on your specific needs, goals, and health conditions. Here’s a detailed comparison to help you decide which might be better for you:
Physiotherapy

What it is:
- A healthcare profession focused on diagnosing, managing, and preventing movement disorders.
- Uses exercises, manual therapy, education, and modalities like ultrasound and electrical stimulation.
Benefits:
- Rehabilitation: Effective for recovering from injuries, surgeries, and chronic conditions like arthritis.
- Pain Management: Addresses the root cause of pain through various techniques and exercises.
- Improved Mobility: Helps restore function and movement, particularly after injury or surgery.
- Preventive Care: Offers strategies to prevent future injuries or manage chronic conditions.
- Customized Treatment: Tailors plans based on individual assessments and needs.
Common Conditions Treated:
- Musculoskeletal injuries (e.g., sprains, fractures)
- Neurological conditions (e.g., stroke, multiple sclerosis)
- Cardiopulmonary issues (e.g., chronic obstructive pulmonary disease)
- Post-surgical rehabilitation
Massage Therapy

What it is:
- A practice involving the manipulation of soft tissues (muscles, tendons, ligaments) to enhance well-being.
- Uses techniques like stroking, kneading, and applying pressure.
Benefits:
- Relaxation: Promotes overall relaxation and stress relief.
- Pain Relief: Alleviates muscle tension and pain.
- Improved Circulation: Enhances blood flow, which can aid in healing.
- Flexibility: Increases range of motion and reduces stiffness.
- Mental Health: Can improve mood and reduce symptoms of anxiety and depression.
Common Conditions Treated:
- Muscle tension and soreness
- Stress-related conditions
- Chronic pain (e.g., back pain, fibromyalgia)
- Sports injuries
- Headaches and migraines
Which is Better for You?
- For Injury Rehabilitation or Chronic Conditions:
- Physiotherapy is typically more suitable as it provides a structured approach to recovery, addressing the underlying causes of your condition.
- For Stress Relief and Muscle Tension:
- Massage Therapy can be highly effective if your primary goal is relaxation and relief from muscle tightness.
- For Pain Management:
- Both can be effective, but the choice depends on the cause of the pain. Physiotherapy is often better for pain related to injury or chronic conditions, while massage therapy can be great for muscle-related pain.
- For Improved Mobility and Function:
- Physiotherapy focuses on restoring function and movement, making it the better choice for mobility issues.
- For Preventive Care:
- Physiotherapy provides long-term strategies to prevent injuries and manage chronic conditions.
- For Overall Well-being and Relaxation:
- Massage Therapy is beneficial for enhancing general well-being, reducing stress, and promoting relaxation.
Combination of Both:
- In some cases, a combination of physiotherapy and massage therapy can be beneficial. For example, physiotherapy can address the underlying issues, while massage therapy can help manage symptoms and improve overall well-being.
Conclusion:
Consult with a healthcare professional to get a personalized recommendation based on your specific health needs and goals. They can help you decide the best course of action and whether one or a combination of both therapies is ideal for you.
Click here to book an appointment with a physiotherapist and massage therapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Choosing between physiotherapy and massage therapy depends on your specific needs and health goals. Both can be beneficial for pain relief and overall wellness. For those looking for physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are skilled practitioners available to help you decide the best approach for your situation.
Physiotherapy can be highly beneficial for individuals suffering from knee osteoarthritis (OA) by addressing pain, improving function, and enhancing the overall quality of life.
What is Knee Osteoarthritis (OA)?
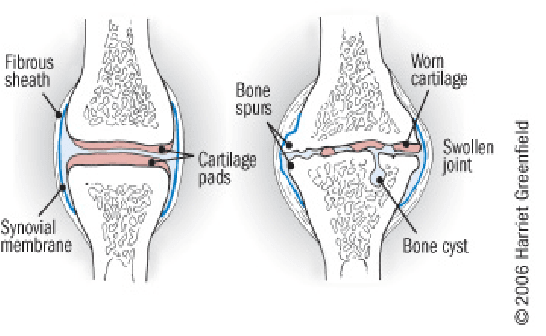
Knee OA is a degenerative joint disease that is typically a result of wear and tear and causes progressive loss of the articular cartilage of the joint.
What are the causes of Knee OA?
Knee osteoarthritis (OA) is a complex condition influenced by a variety of factors. Here are the primary causes and contributing factors:
1. Aging
- Natural Wear and Tear: As people age, the cartilage that cushions the knee joint gradually wears away, leading to OA.
- Decreased Ability to Heal: Older cartilage has a reduced ability to repair itself, making it more susceptible to damage.
2. Genetics
- Family History: Genetic predisposition can play a significant role. If OA runs in your family, you might be more likely to develop it.
- Genetic Mutations: Certain genetic mutations can affect cartilage production and maintenance.
3. Joint Injuries
- Previous Injuries: Injuries such as fractures, ligament tears, or meniscus damage can increase the risk of OA.
- Repetitive Stress Injuries: Repeated stress or overuse of the knee joint, often due to occupational or recreational activities, can lead to OA.
4. Obesity
- Increased Joint Load: Excess body weight puts additional stress on the knee joints, accelerating cartilage breakdown.
- Inflammation: Fat tissue produces inflammatory chemicals that can contribute to joint damage.
5. Mechanical Factors
- Joint Alignment: Abnormal joint alignment, such as bowlegs or knock-knees, can increase stress on certain parts of the knee.
- Muscle Weakness: Weak muscles around the knee, particularly the quadriceps, can lead to increased joint stress.
6. Gender
- Higher Risk in Women: Women, especially those over 50, are more likely to develop knee OA compared to men. Hormonal differences might contribute to this increased risk.
7. Metabolic and Systemic Factors
- Metabolic Syndrome: Conditions like diabetes and metabolic syndrome are associated with an increased risk of OA due to systemic inflammation and metabolic disturbances.
- Inflammatory Diseases: Conditions such as rheumatoid arthritis can predispose individuals to secondary OA.
8. Lifestyle Factors
- Physical Activity: Both excessive and insufficient physical activity can affect joint health. High-impact sports can lead to joint injuries, while sedentary lifestyles can weaken muscles and joints.
- Diet: Poor nutrition can affect joint health. For example, deficiencies in vitamins D and C can impair cartilage maintenance and repair.
9. Joint Biomechanics
- Meniscus Tears: Damage to the meniscus can disrupt joint mechanics and contribute to OA.
- Ligament Damage: Injuries to ligaments, such as the ACL, can destabilize the knee and lead to abnormal wear patterns.
10. Inflammation
- Low-Grade Inflammation: Chronic low-grade inflammation can contribute to the breakdown of cartilage and other joint tissues.
Understanding these causes and contributing factors can help in the prevention and management of knee osteoarthritis, emphasizing the importance of maintaining a healthy lifestyle, avoiding joint injuries, and seeking early intervention for symptoms.
What are the most common symptoms of Knee OA?
Knee osteoarthritis (OA) typically presents with a range of symptoms that can vary in intensity from mild to severe. The most common symptoms include:
1. Pain
- Activity-Related Pain: Pain that worsens with activity or weight-bearing and improves with rest.
- Persistent Pain: Chronic pain that may be present even at rest or during the night in more advanced stages.
2. Stiffness
- Morning Stiffness: Stiffness in the knee that is usually worse in the morning or after periods of inactivity and typically lasts less than 30 minutes.
- Post-Activity Stiffness: Stiffness that occurs after prolonged sitting or resting.
3. Swelling
- Joint Swelling: Swelling around the knee joint due to inflammation or increased production of joint fluid.
- Effusion: Accumulation of excess fluid within the knee joint, leading to noticeable swelling.
4. Reduced Range of Motion
- Limited Flexibility: Difficulty bending or straightening the knee fully.
- Loss of Motion: Progressive decrease in the knee’s range of motion over time.
5. Grinding Sensation (Crepitus)
- Audible Cracking or Popping: A sensation of grinding, cracking, or popping sounds when moving the knee, often due to roughened cartilage surfaces.
6. Weakness or Instability
- Feeling of Giving Way: A sensation that the knee might buckle or give out, often due to muscle weakness or joint instability.
- Muscle Weakness: Weakness in the muscles surrounding the knee, particularly the quadriceps.
7. Deformity
- Joint Deformities: Changes in the shape of the knee joint, such as bowlegged (varus) or knock-kneed (valgus) appearance, due to uneven wear and joint damage.
8. Tenderness
- Joint Tenderness: Tenderness or pain when pressing on or around the knee joint.
9. Functional Impairment
- Difficulty with Activities: Challenges with everyday activities such as walking, climbing stairs, sitting, or standing due to pain and stiffness.
- Reduced Mobility: Decreased ability to perform normal daily activities and exercise.
10. Fatigue
- General Fatigue: Feeling of tiredness and reduced energy levels, often due to chronic pain and sleep disturbances.
These symptoms can significantly impact an individual’s quality of life and ability to perform daily activities. Early recognition and management of knee OA symptoms can help slow disease progression and improve function and comfort.
What are the treatment options for Knee OA?
The number 1 treatment option is conservative management (ie. Patient education, therapeutic exercise, activity modification, weight loss, bracing), surgery should be considered after a conservative approach (talk to your orthopaedic specialist for more information).
Physiotherapy can help by providing you with education about osteoarthritis, tailor an exercise program that is suitable for you, help you consider the best options for activity modifications, provide you with education on bracing, address psychosocial factors such as fear-avoidance, promote patient autonomy and get you back to doing the things you love to do!
Manual therapy- joint mobilization to help with stiffness. Muscle energy technique to help stretch surrounding muscles.
Modalities – heat/ice for pain relief, TENs/IFC for pain relief and inflammation control. Ultrasound for pain relief.
Exercises – help with improving mobility, ROM, strength, balance, aerobic capacity, promoting physical function, reducing knee pain and inflammation.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy can be a highly effective treatment for managing knee osteoarthritis by improving mobility, reducing pain, and enhancing overall function. Whether you are looking for physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are experienced physiotherapists ready to help you manage osteoarthritis and improve your quality of life.
Physiotherapy and chiropractic care are both forms of manual therapy that focus on the treatment of musculoskeletal issues, but they have different approaches, philosophies, and techniques. Here’s a comparison of the two:
Physiotherapy

Approach:
- Holistic and comprehensive treatment aimed at restoring movement and function.
- Utilizes evidence-based practices.
Philosophy:
- Focuses on the body as a whole and treats a wide range of conditions, including musculoskeletal, neurological, and cardiovascular issues.
- Emphasizes rehabilitation, prevention, and overall well-being.
Techniques:
- Exercises and stretches to improve mobility and strength.
- Manual therapy, including massage and mobilization of joints.
- Electrotherapy, ultrasound, and other modalities for pain relief and inflammation reduction.
- Education and advice on posture, ergonomics, and lifestyle changes.
Conditions Treated:
- Musculoskeletal pain (e.g., back, neck, shoulder).
- Post-operative rehabilitation.
- Sports injuries.
- Pelvic Health
- Cancer Rehab
- Vestibular Conditions
- Neurological disorders (e.g., stroke, Parkinson’s disease).
- Chronic conditions (e.g., arthritis).
Qualifications:
- Requires a degree in physiotherapy and registration with provincial regulatory body.
- Involves extensive training in anatomy, physiology, and pathology.
Chiropractic

Approach:
- Primarily focuses on the diagnosis and treatment of mechanical disorders of the spine.
- Utilizes spinal adjustments and manipulations.
Philosophy:
- Based on the principle that spinal health affects overall health and well-being.
- Emphasizes the relationship between the spine and nervous system.
Techniques:
- Spinal manipulations and adjustments to restore joint function and support the nervous system.
- Manual adjustments often performed with a high-velocity thrust.
- May include advice on exercise, diet, and lifestyle.
Conditions Treated:
- Back and neck pain.
- Headaches and migraines.
- Joint pain (e.g., hips, knees).
- Sciatica and other nerve-related issues.
Qualifications:
- Requires a Doctor of Chiropractic (DC) degree and registration with provincial regulatory body.
- Involves training in anatomy, physiology, and specialized chiropractic techniques.
Key Differences between Physiotherapy and Chiropractic
- Scope of Practice:
- Physiotherapists: Treat a broader range of conditions affecting various body systems.
- Chiropractors: Primarily focus on spinal health and its impact on overall health but can also treat other musculoskeletal conditions.
- Techniques Used:
- Physiotherapists: Employ a wide variety of techniques including exercise, manual therapy, and electrotherapy.
- Chiropractors: Primarily use spinal adjustments and manipulations but are also trained in treating other joints.
- Philosophical Focus:
- Physiotherapists: Emphasize holistic rehabilitation and prevention.
- Chiropractors: Emphasize the importance of spinal alignment for overall health.
- Educational Path:
- Physiotherapists: Typically require a Bachelor’s or Master’s degree in physiotherapy.
- Chiropractors: Require a Doctor of Chiropractic degree.
When to Choose Each
- Physiotherapy: Suitable for a wide range of conditions, particularly when rehabilitation, exercise, and a holistic approach are needed.
- Chiropractic Care: Beneficial for conditions specifically related to spinal health and when spinal adjustments are indicated.
Ultimately, the choice between physiotherapy and chiropractic care may depend on the specific condition being treated, the patient’s preferences, and the recommendations of healthcare professionals. In some cases, a combination of both therapies might be the most effective approach.
Click here to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Deciding between physiotherapy and chiropractic care depends on your specific needs and conditions. Both can offer significant benefits for pain management and overall health. If you are considering physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are expert physiotherapists available to guide you toward the best treatment approach for your unique situation.