Foot pain is a common complaint that can significantly impact our daily lives. From discomfort while walking to more severe conditions, understanding the underlying causes can help us prevent and manage this issue effectively. In this blog post, we’ll explore the most common reasons for foot pain and discuss effective strategies for prevention and treatment.
The team of physiotherapists at Triangle Physiotherapy have the training and expertise to diagnose the problem and help you a customized treatment plan and get your recovery journey started.
Common Causes of Foot Pain

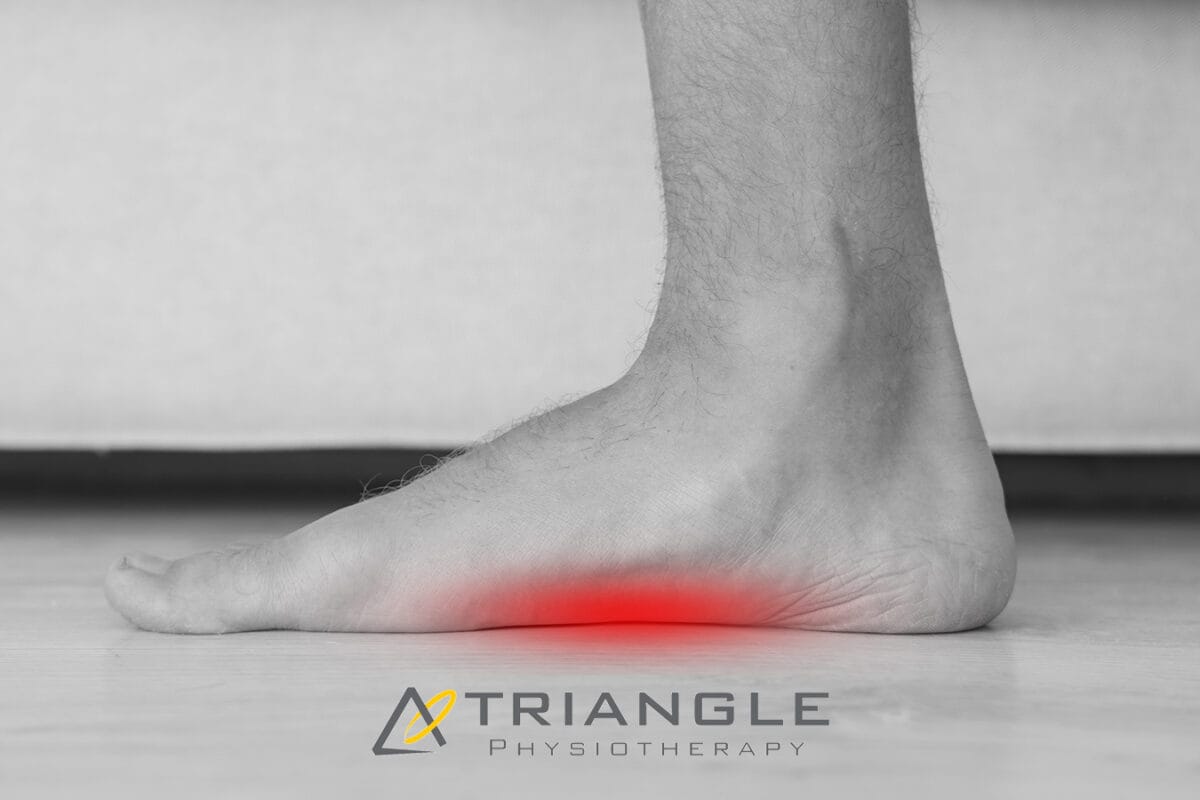
- Plantar Fasciitis: This condition occurs due to inflammation of the plantar fascia, a tissue that connects the heel bone to the toes. Symptoms often include sharp pain in the heel, especially upon waking up.
- Achilles Tendinitis: The Achilles tendon, the largest tendon in the body, can become inflamed due to overuse, improper footwear, or sudden increases in activity. This leads to pain and stiffness in the back of the heel.
- Stress Fractures: These tiny breaks in bones can occur due to repetitive stress or sudden increases in activity. Common locations for stress fractures in the foot include the metatarsals and the navicular bone.
- Bunions: Bunions are bony bumps that form at the base of the big toe, often causing pain and discomfort. They can be caused by genetic factors, tight-fitting shoes, or biomechanical issues.
- Neuromas: These are benign growths that occur between the toes, often causing a burning or tingling sensation. They are more common in women and can be caused by high-heeled shoes or other factors.
Prevention of Foot Pain

- Proper Footwear: Choose shoes that fit well and provide adequate support and cushioning. Avoid wearing high heels or shoes that are too tight or too loose.
- Stretching and Strengthening: Regular stretching exercises can help to improve flexibility and reduce the risk of injury. Strengthening exercises can help to build the muscles that support the feet and ankles.
- Maintain a Healthy Weight: Excess weight can put additional stress on the feet, increasing the risk of pain and injury.
- Take Breaks: If you have a job that requires you to stand or walk for long periods, take regular breaks to rest your feet.
- Address Biomechanical Issues: If you have underlying biomechanical problems, such as flat feet or high arches, consider orthotics or other interventions to correct these issues.
The Importance of Physiotherapy for Foot Pain
A physiotherapist can play a crucial role in diagnosing and treating foot pain. They can assess your condition, provide targeted exercises and stretches, and recommend appropriate footwear or orthotics. Physiotherapy can help to reduce pain, improve mobility, and prevent future injuries.
Neuromuscular Exercises for Foot Pain
Neuromuscular exercises focus on improving the coordination between your muscles and nerves, which can help to stabilize your feet and ankles. Examples of neuromuscular exercises include balance exercises, proprioceptive training, and plyometric drills.
Progressive Resistance Exercises for Foot Pain
Progressive resistance exercises gradually increase the strength and endurance of the muscles in your feet and ankles. This can help to improve stability and reduce the risk of injury. Examples of resistance exercises include calf raises, toe curls, and resistance band exercises.
Incorporating Mobility into Daily Life
Mobility is essential for maintaining healthy feet and ankles. Incorporate mobility exercises into your daily routine, such as walking, swimming, or yoga. These activities can help to improve flexibility, strength, and overall foot health.
Tips for Safety
- Listen to Your Body: If you experience pain or discomfort, take a break and rest.
- Avoid Overdoing It: Gradually increase the intensity and duration of your activities to avoid injury.
- Seek Professional Help: If you have persistent foot pain or concerns, consult with a physiotherapist to get it resolved.
Locations of Triangle Physiotherapy Clinics:
If you have had achilles tendon repair surgery or are scheduled for a procedure, you are likely going to need post-surgery rehabilitation to recover completely. It is also advisable to do physiotherapy pre-surgery to maximize the outcomes of the surgery. This is also known as prehab or pre-surgery rehab. At Triangle Physiotherapy, our physiotherapists are skilled and experienced at helping their patients reach their optimal level of recovery. If you’re looking for expert guidance in post-surgery rehab near you or post-operative physiotherapy in Toronto, you’ve come to the right place.
Achilles tendon injuries are common, particularly among athletes and active individuals. The Achilles tendon, the largest and strongest tendon in the body, connects the calf muscles to the heel bone, playing a crucial role in walking, running, and jumping. When this tendon is torn or ruptured, Achilles repair surgery is often necessary. However, surgery is only the first step toward recovery. Effective rehabilitation is essential for restoring function, strength, and mobility. In this blog, we’ll guide you through the stages of Achilles repair surgery rehab, providing insights and tips to ensure a successful recovery.
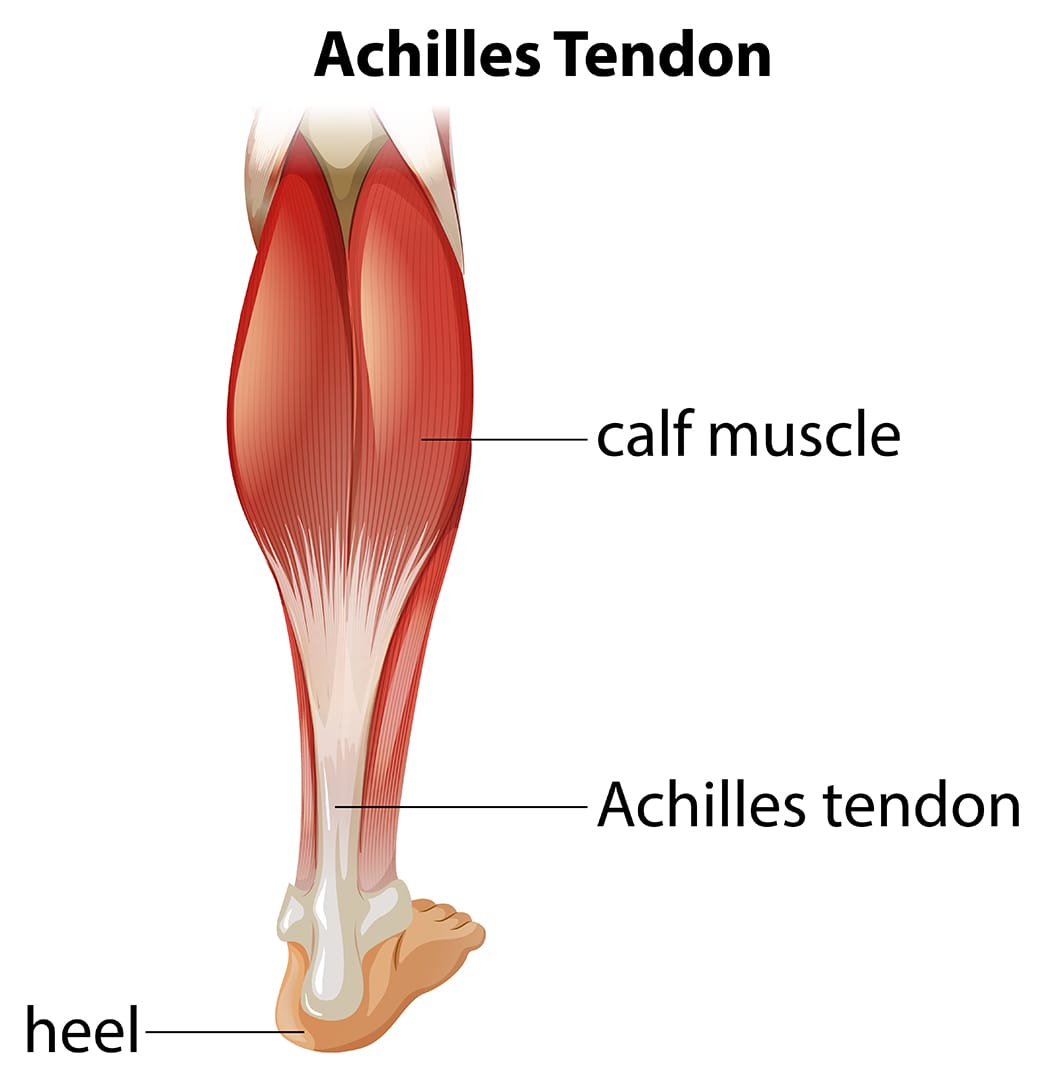
Understanding Achilles Tendon Injuries
What is the Achilles Tendon?
The Achilles tendon is a band of fibrous tissue that links the calf muscles to the heel bone. It enables activities that involve pushing off the foot, such as running and jumping.
Common Causes of Achilles Tendon Injuries
- Overuse: Repetitive stress from activities like running can lead to micro-tears.
- Sudden Increase in Activity: Rapid changes in activity levels can strain the tendon.
- Trauma: Direct impact or sudden, forceful movement can cause a rupture.
- Age and Degeneration: As people age, tendons become less flexible and more prone to injury.
Achilles Repair Surgery
Goals of Surgery
- Reattach the torn ends of the tendon.
- Restore the tendon’s length and tension.
- Enable the patient to return to their pre-injury level of activity.
Tips for a Successful Rehab
- Consistency: Adhere to the rehab program and attend all physiotherapy sessions.
- Listen to Your Body: Avoid pushing through pain; inform your therapist of any discomfort.
- Nutrition: Maintain a balanced diet to support tissue repair and overall health.
- Patience: Recovery takes time; focus on gradual progress rather than rushing the process.
Rehabilitating after Achilles repair surgery is a structured and multi-phased process that requires dedication and guidance from skilled physiotherapists. At Triangle Physiotherapy, we are committed to providing personalized rehabilitation programs to ensure our patients achieve optimal recovery and return to their active lifestyles. If you’ve undergone Achilles repair surgery or are scheduled for one, contact us to learn how our expert team can support you through every step of your recovery journey.
For those searching for physiotherapy in Toronto, post-surgery rehab in Toronto, or post-operative physiotherapy in Toronto, we offer comprehensive services tailored to your needs.
For more information or to schedule an appointment, or call us at 416.203.8622. Let us help you get back on your feet stronger and healthier.
“Recovering from Achilles repair surgery requires expert care and guidance. Triangle Physiotherapy offers comprehensive rehabilitation services at several locations across the GTA. Visit our clinics for Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village to ensure a smooth and effective recovery journey with the help of our specialized physiotherapy team.”
Hiking is a fantastic way to enjoy the great outdoors and stay fit, but it can also pose some risks. Whether you’re new to hiking or a seasoned backpacker, there are numerous factors to take into account before heading out on the trails. You need to evaluate your backpack’s weight, choose appropriate footwear, plan your food and hydration, check the weather, and map out your routes. Additionally, since hiking often takes you off the beaten path, it’s essential to take precautions against three common hiking injuries: knee pain, ankle sprains, and sore feet.
Is it necessary to warm up before hiking?
Yes, it is necessary to warm up before hiking. Warming up helps prepare your muscles and joints for physical activity, reducing the risk of injury. Here are some reasons why warming up is important before hiking:
Benefits of Warming Up Before Hiking
- Increases Blood Flow: A proper warm-up increases blood flow to your muscles, delivering oxygen and nutrients that help them perform better.
- Enhances Flexibility: Warming up loosens your muscles and increases your range of motion, making it easier to navigate uneven terrain.
- Reduces Injury Risk: Warm muscles are less prone to strains, sprains, and other injuries.
- Prepares Your Heart: Gradually increasing your heart rate helps prepare your cardiovascular system for the more strenuous activity of hiking.
- Improves Performance: A good warm-up can improve your overall performance, making your hike more enjoyable and less exhausting.
What are some effective warm up exercises to do before hiking?
Effective Warm-Up Exercises
- Walking or Light Jogging: Start with 5-10 minutes of brisk walking or light jogging to get your blood flowing.
- Dynamic Stretches: Perform dynamic stretches like leg swings, arm circles, and torso twists to loosen up your muscles and joints.
- Ankle Rotations: Rotate your ankles in circles to prepare them for the uneven terrain.
- Hip Circles: Rotate your hips to loosen the hip joints, which are crucial for hiking.
- Calf Raises: Perform calf raises to warm up your calves, which are heavily used during hiking.
Taking a few minutes to warm up before you start your hike can make a significant difference in your overall hiking experience and help prevent injuries.
What are the most common hiking injuries?
Some of the most common hiking injuries are:
- Knee Pain
- Ankle Sprain
- Foot Pain
Knee Pain when Hiking
Knee pain is a common issue among hikers, especially on longer or more challenging trails. Here’s a comprehensive approach to understanding, preventing, and managing knee pain when hiking:
Causes of Knee Pain While Hiking
- Overuse and Strain: Continuous stress on the knee joint from uphill climbs, downhill descents, or long sessions of hiking.
- Improper Biomechanics: Poor hiking technique, such as improper foot placement or stride, can strain the knee joint.
- Previous Injuries: Past knee injuries or conditions like arthritis can flare up during hiking.
- Improper Gear: Worn-out or inappropriate footwear lacking proper cushioning and support.
Ankle Sprain when Hiking
An ankle sprain can be a painful and frustrating injury, especially when hiking in rugged terrain. Here’s how to understand, prevent, and manage ankle sprains while hiking:
Causes of Ankle Sprains While Hiking
- Uneven Terrain: Stepping on uneven surfaces, rocks, or roots can twist or roll the ankle.
- Fatigue: Muscles that support the ankle can become tired, leading to less stability and increased risk of injury.
- Inadequate Footwear: Wearing shoes or boots without proper ankle support or that are worn out.
Foot Pain when Hiking
Foot pain while hiking can be uncomfortable and distracting. Here’s how to understand, prevent, and manage foot pain effectively:
Causes of Foot Pain While Hiking
- Improper Footwear: Shoes or boots that are too tight, loose, worn out, or lacking proper cushioning and support.
- Overuse or Strain: Prolonged walking or hiking, especially on challenging terrain, can strain the muscles and joints of the feet.
- Blisters: Friction from improperly fitting shoes or moisture buildup can lead to painful blisters.
If you get injured while hiking, consult one of our physiotherapists who can help you with treating the injuries as well as advise and educate you on prevention so you can enjoy your outdoor activities without pain and discomfort.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
What is Plantar Fasciitis?
Plantar fasciitis is an overuse injury. Accumulation of micro-damage leads to the degradation of the collagen fibers that make up the origin point of the plantar aponeurosis. This prevalent condition is the most common cause of heel pain. It is a common condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot. Managing plantar fasciitis involves a combination of lifestyle changes, exercises, and medical interventions.
What are the risk factors for plantar fasciitis?
- Overpronation
- High-Arched Feet
- Leg-length Discrepancy
- Footwear
Here are five ways to manage plantar fasciitis:
- Stretching Exercises:
- Perform gentle stretching exercises for the Achilles tendon, calf muscles, and plantar fascia. Regular stretching can help alleviate tension and improve flexibility.
- Towel stretches, calf stretches, and wall stretches are beneficial for targeting the affected areas.
2. Night Splints:
- Wear night splints to keep the foot in a dorsiflexed position while sleeping. This helps stretch the plantar fascia and Achilles tendon, promoting healing and reducing morning pain.
3. Custom Orthotics
- For orthotics to successfully treat plantar fasciitis, they need to control overpronation and the motion of the first metatarsal head.
4. Supportive Footwear
- Choose shoes with proper arch support and cushioning to reduce strain on the plantar fascia. Avoid high heels and worn-out shoes.
- Consider orthotic inserts or custom-made insoles to provide additional support and stability.
5. Physiotherapy
- Consult with a physiotherapist who can guide you through exercises and techniques to strengthen the muscles around the foot and improve overall foot mechanics.
- Shockwave therapy has been known to show great results in the management of plantar fasciitis.
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Managing plantar fasciitis effectively requires a combination of the right treatments and exercises. For professional support in addressing foot pain, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can provide personalized care plans to help you recover and stay active.
A running assessment is a process in which an individual’s running form, biomechanics, and overall performance are evaluated by a physiotherapist. The goal of a running assessment is to identify any issues or inefficiencies in the individual’s running technique that may contribute to discomfort, pain, or decreased performance.
What are the components of a Running Assessment?

Key components of a running assessment may include:
- Gait Analysis: Observing the way an individual walks or runs to assess their biomechanics, stride length, foot strike pattern, and overall form.
- Footwear Analysis: Evaluating the type and condition of the running shoes worn by the individual to ensure they provide proper support and are suitable for their running style.
- Muscle and Joint Assessment: Checking for any muscle imbalances, weaknesses, or joint restrictions that may affect running mechanics.
- Injury History: Review the individual’s history of injuries, if any, to identify patterns or recurring issues that may be related to running technique.
- Functional Movement Assessment: Assessing the individual’s flexibility, strength, and stability, especially in areas relevant to running, such as the hips, knees, and ankles.
- Running on a Treadmill or Track: The individual may be observed while running on a treadmill or a track to get a real-time assessment of their running mechanics.
- Discussion of Training Goals: Understanding the individual’s running goals, whether they are training for a specific event, improving performance, or addressing pain or discomfort.
I am a novice runner, can I still do a running assessment?
Absolutely. As a novice runner, it is very important to learn the proper technique so that you don’t injure yourself. The physiotherapist will assess you and help you with technique, shoe selection, and a training plan if you want to run a marathon.
Where can I find a physiotherapist who does Running Assessments in Toronto?
We have 8 locations with physiotherapists to help you run better.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
A running assessment can help identify and correct biomechanical issues to improve performance and prevent injuries. For a comprehensive running assessment and personalized care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Expert physiotherapists in these locations can help you optimize your running form and stay injury-free.
Shockwave therapy, also known as extracorporeal shock wave therapy (ESWT), is a non-invasive medical treatment that uses acoustic waves to stimulate healing in various musculoskeletal conditions, including plantar fasciitis. Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes.

Here’s how shockwave therapy is typically used for plantar fasciitis:
- Mechanism of Action:
- Shockwave therapy works by delivering high-energy shockwaves to the affected area. These shockwaves create microtrauma in the tissue, which triggers the body’s natural healing response.
- The treatment is thought to stimulate blood flow, promote tissue regeneration, and reduce inflammation.
- Procedure:
- During the procedure, a gel is applied to the skin of the affected foot to help transmit the shockwaves.
- A handheld device is then used to deliver controlled shockwaves to the targeted area, typically the heel or the sole of the foot.
- Number of Sessions:
- The number of shockwave therapy sessions required can vary.
- Some individuals may experience relief after just one session, while others may require additional treatments.
- Post-Treatment:
- After the procedure, patients may experience temporary soreness or discomfort, but this usually subsides within a few days.
- It’s important to follow any post-treatment instructions provided by the healthcare provider, which may include rest, ice, and avoiding certain activities.
- Effectiveness: The use of shockwave therapy is often considered when conservative treatments, such as rest, stretching exercises, orthotics, and anti-inflammatory medications, have not provided sufficient relief.
It’s crucial to note that while shockwave therapy may be beneficial for some individuals, it may not be suitable for everyone. Patients should consult with their healthcare provider to determine the most appropriate treatment approach based on their specific condition and medical history.
Who can provide Shockwave Therapy at Triangle Physiotherapy?
Shockwave Therapy can be provided at our clinics by a physiotherapist, a chiropractor or a massage therapist.
Will Shockwave Therapy be covered by my insurance?
Yes, shockwave therapy will be covered depending on the healthcare practitioner providing the service. For example, if you are seeing a physiotherapist for shockwave therapy, it will be covered under your physiotherapy coverage.
How do I book an appointment with a physiotherapist or chiropractor near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Shockwave therapy is an effective treatment for plantar fasciitis, helping to reduce pain and promote healing. Triangle Physiotherapy provides expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists are here to help you find relief from plantar fasciitis and get back on your feet.”
Yes, a physiotherapist can definitely help with plantar fasciitis. They can provide specialized exercises, stretching techniques, and other treatments to alleviate pain, improve mobility, and promote healing of the plantar fascia.

What is plantar fasciitis and what causes it?
Plantar Fasciitis is a painful condition resulting from inflammation of a band of connective tissue located on the bottom side of the foot known as the Plantar Fascia. This band of connective tissue runs from the heel of the foot, all the way to the base of each toe, and it functions to support the arch of the foot, especially during weight-bearing.
What are the symptoms of plantar fasciitis?
The pain associated with Plantar Fasciitis is located on the bottom of the foot, with it often manifesting around the heel and along the inside of the foot. It is common for this pain to be at its worst first thing in the morning, and it is usually accompanied by other symptoms, such as stiffness, weakness, swelling, and decreased proprioception.
How is it diagnosed by a physiotherapist?
A Physiotherapist will run a thorough examination of the problem to ensure a proper diagnosis is obtained. This will include getting a detailed history, observing the area and how you function, and running through a series of specific tests. From there, an individualized treatment plan will be made for you to help you achieve your goals and assist you on your road to recovery.
Who is the most at risk to develop this condition?
Plantar Fasciitis is more common in people who can relate to the following:
- Have flat feet or high arches
- Have tight calf muscles
- Wear improper footwear
- Engage in repetitive physical activity (overtraining)
- Suddenly changed activity levels (increased frequency, duration, or intensity)
- Suddenly changed activity or training environment
- Work in an environment that requires prolonged standing
What is the best treatment for plantar fasciitis?
Physiotherapy is considered to be very effective in treating plantar fasciitis. The treatment starts with managing the initial pain and symptoms after which the soft tissue is gradually loaded to promote strengthening so that the condition does not reoccur.
What does plantar fasciitis treatment look like?
Plantar Fasciitis treatment can include one or more of the following:
- Rest: Avoid activities that worsen the pain and give your feet time to heal.
- Ice: Applying ice to the affected area can help reduce inflammation and pain.
- Stretching: Regularly perform calf and foot stretches to help improve flexibility and reduce tension on the plantar fascia.
- Footwear: Choose supportive and cushioned shoes that provide proper arch support.
- Orthotics: Custom or over-the-counter shoe inserts can help distribute pressure evenly on the foot.
- Night splints: These devices keep the foot in a stretched position overnight to alleviate morning pain.
- Physiotherapy: A physiotherapist can guide you through exercises and treatments to aid recovery.
- Extracorporeal Shock Wave Therapy (ESWT): In some cases, this treatment may be used to stimulate healing.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Plantar fasciitis can be effectively managed with the help of a skilled physiotherapist. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can develop a personalized treatment plan to alleviate your symptoms and help you get back on your feet.”
What is Plantar Fasciitis?

Plantar Fasciitis is a type of foot pain resulting from inflammation of a band of connective tissue located on the bottom side of the foot known as the Plantar Fascia. This band of connective tissue runs from the heel of the foot, all the way to the base of each toe, and it functions to support the arch of the foot, especially during weight-bearing.
The pain associated with Plantar Fasciitis is located on the bottom of the foot, with it often manifesting around the heel and along the inside of the foot. It is common for this pain to be at its worst first thing in the morning, and it is usually accompanied by other symptoms, such as stiffness, weakness, swelling and decreased proprioception.
What is the Plantar Fascia?
The plantar fascia is a flat band of tissue that connects your heel bone (Calcaneus) to the base of the toes (Metatarsophalangeal joints). This ligament assists in supporting the arch of your foot.
What causes Plantar Foot Pain?
People experience this when they have strained the connective tissue from repetitive overloading to the area. Repetitive overloading causes little tears to occur, and over time this produces inflammation and other associated symptoms, as described above.
Plantar Fasciitis is more common in people who can relate to the following:
- Have flat feet or high arches
- Have tight calf muscles
- Wear improper footwear
- Engage in repetitive physical activity (overtraining)
- Suddenly changed activity levels (increased frequency, duration or intensity)
- Suddenly changed activity or training environment
- Work in an environment that requires prolonged standing
Plantar Fasciitis is one of the most common reasons people experience foot pain and seek Physiotherapy treatment to solve it.
How can a physiotherapist at Triangle Physiotherapy help with plantar foot pain?
A Physiotherapist at Triangle Physiotherapy will do a thorough assessment of the fot to ensure a proper diagnosis is obtained. This will include getting a detailed history, observing the area and how you function, and running through a series of specific tests. From there, an individualized treatment plan will be made for you to help you achieve your goals and assist you on your road to recovery.
If you think you might have Plantar Foot Pain, contact us to book an appointment with one of our Physiotherapists today!
“Managing plantar foot pain effectively requires targeted physiotherapy. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists provide personalized care to help alleviate pain and improve foot function, ensuring you can get back on your feet with confidence.”
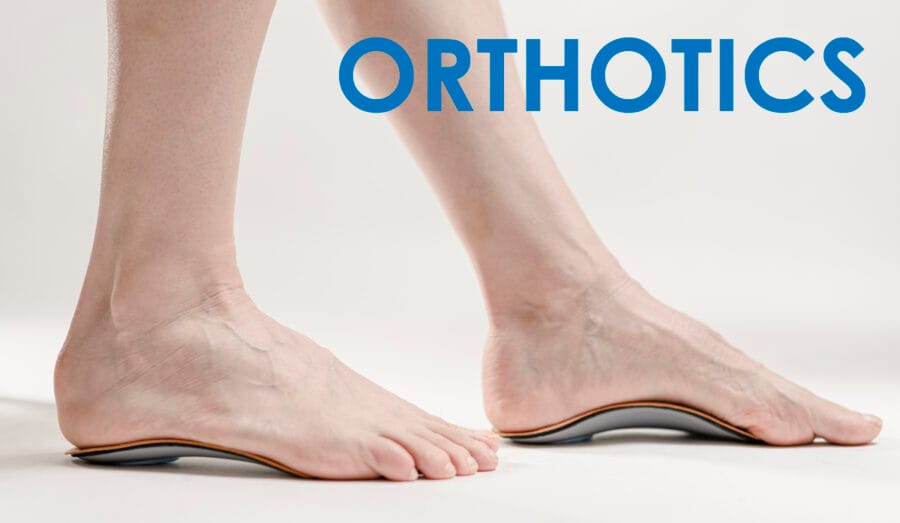
What are orthotics?
Orthotics are custom made inserts that are worn inside your shoe to control abnormal foot function.
Orthotics solve a number of biomechanically related problems, for example, ankle and knee pain, pelvis, hip, spinal pain. This is achieved by preventing misalignment of the foot, which significantly alters the way in which the bones move within their joints.
Orthotics work for the feet the same way prescription glasses work for the eyes.

Who can benefit from orthotics?
Custom orthotics can be used for all ages and for a variety of activities and can be made to fit any type of shoe.
Where can I get the best custom orthotics?
The best custom orthotics can be purchased from a clinic where a chiropodist or qualified health professional conducts an assessment and a 3D scan of your feet to determine the best orthotics for you. The 3D Scan is then sent to a lab where the scan is used to manufacture your orthotics.
Triangle Physiotherapy has qualified health practitioners that can assess you and recommend the best custom orthotics for you.
How can Orthotics correct foot conditions?
The best custom orthotics can:
- Help balance pressure placed on the feet by redistributing the weight appropriately
- Help stabilize the heel
- Support the arch of the feet
- Provide cushioning to delicate and inflamed areas of the feet that arise from too much walking, jogging, running, etc.
What is a knee brace and how can it help me?
A knee brace can help support and stabilize an unstable knee due to injury or osteoarthritis. The best knee brace will offer the support you need in order to balance and evenly distribute your weight in order to have a more comfortable walk or run.
What conditions can a knee brace help with?
Whether it’s a knee sprain, arthritis, torn ACL, runner’s knee, knee instabilities or knee discomfort, the best knee braces help support and manage pain.
When should I start wearing a knee brace?
Once you start experiencing knee pain or discomfort or find that the knee is unstable while walking or running or after you have had knee surgery , book an appointment with one of our health practitioners who can assess you and recommend the best knee brace for you.
“Custom orthotics and knee braces can significantly improve mobility and reduce pain. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can help you find the best solutions to support your foot and knee health, ensuring a personalized approach to your treatment.”
Re: Kevin Durant’s mid-game calf strain
Kevin Durant, Durantula, easymoneysniper, whatever you want to call him is a superstar basketball player and is regarded by many as the second-best basketball player in the world. Unless you have been living under a rock in Toronto, you should know his name and the impact of his eventual return to the NBA Finals. Moreover, if you’re a therapist like me, you may feel disgusted about the mismanagement of his return to the court on Monday.
Here are the facts:
- Kevin Durant was diagnosed with a right calf strain on May 8th, 2019, which many suspected was an Achilles strain to begin with. Grade 1 Calf Strain can take anywhere from 7-10 days to resolve. Durant was out for a whole month!
- Kevin Durant was cleared for practice on June 9th and he did so with his teammates (unsure of the extent of this practice as it was closed off to the media)
- After his practice, Kevin Durant is noted leaving practice with a slight limp and ice on his right Achilles (to help with possible pain/inflammation?)
- A few hours before tip off he is upgraded to questionable to play in game 5 of the NBA finals, and 90 minutes before tip off it is known that he is cleared to play and will start in game 5, with no minutes restriction. WHAT?
- Kevin Durant does indeed start game 5, and starts off hot connecting on his first 3 attempts beyond the arc and scoring 11 points in the first quarter.
- At 9:46 of the second quarter, Durant came up the court and tried to accelerate past Ibaka with his right foot planted, and that was enough. Durant fell to the ground holding his right Achilles.
- Teammates and opposing players help him back to the locker room, and post game Durant is seen leaving the Scotiabank Arena in a walking boot and crutches
- Durant is expected to fly to New York to have an MRI done, which many believe will confirm a right ruptured Achilles.
Also read, Physiotherapy Rehab Clinic in Mississuaga
What is an Achilles Tear/Rupture and what does it mean for Durant?
The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump.
Achilles tendon ruptures can occur spontaneously in individuals and one symptom many people display is the pop or gunshot sound of their Achilles tendon rupturing. If you look in the video above, you can notice the pop of the Achilles and the subsequent vibration of the calf muscles accordingly.
Detailed in an article by Physio Works it states:
Achilles Ruptures occur mostly in middle-aged men, most of whom play recreational sports Injury often occurs during recreational sports that require bursts of jumping, pivoting and running.
They can happen in these situations:
- You make a forceful push-off with your foot while your knee is straightened by the powerful thigh muscles. One example might be starting a foot race or jumping.
- You suddenly trip or stumble, and your foot is thrust in front to break a fall, forcefully overstretching the tendon.
- You fall from a significant height.
Also read, Physiotherapy Rehab Clinic in Etobicoke
The biggest risk factor for Achilles tendon rupture is tendon cell death which occurs as a result of poorly managed tendinopathy.
As noted in the bold statements, these are the exact scenarios which led to the possible tendon rupture for Kevin Durant, with strong emphasis on the second statement!
While we don’t know the extent of Kevin Durant’s Achilles tear, we can only speculate that it is a complete rupture and thus provide this comparative timeline on his return to that of another NBA player, Rudy Gay, who tore his Achilles in 2017 at the same age, and has the body frame similar to that of Durant.
If the MRI on Tuesday confirms a complete tear and Durant follows a similar timeline to that of Gay
- Durant will undergo surgery to repair the tendon
- He will be on crutches and in a boot for the next six weeks.
- He will start physical therapy in two weeks and formal rehabilitation at eight weeks post-surgery.
- >12 weeks post he can begin sport specific training
- Return to sport is anticipated in 6 months
Now if Kevin Durant is able to follow the same path as Rudy Gay, what are the implications to his career? He was a free agent this year hoping to be signed to a max contract with the team of his choosing as every team salivated at the idea of signing him (Brooklyn, Knicks to name a few). Will teams take that gamble anymore? It’s Kevin Durant, so I am sure they will. Yet, he may be forced to stay in Golden State another year as he returns to the court to prove that he isn’t damaged goods. Keep in mind, numerous athletes in the past were never the same after facing a similar injury. Kobe is one that comes to mind, and this ultimately led to his retirement. Currently we see the same with Durant’s teammate Demarcus Cousins who went from being an all-star to a bench caliber player. Moreover, Rudy gay was quoted as saying that it took him almost a full year and a half to feel 100% again. Which scenario will apply to Durant? How long, if ever, will it take for him to be truly 100% again, as he sits in the prime of his career? All valid questions probably going through Kevin Durant’s head as he awaits his MRI results on Tuesday.
Also read, Physiotherapy Rehab Clinic in Oakville
Moreover, as we await the results of the MRI, I also question the doctors, therapists, and ownership of the Golden State Warriors on making the decision for Kevin Durant to return to Game 5. I get that the athlete has the final say as to whether they want to play or not (Kawhi Leonard comes to mind here ironically), but considering the immense amount of pressure put on Durant to help the Warriors avoid upset, and amplify his legacy, one can only point the finger at the medical and management team for allowing him to go out there. He was clearly still nursing a calf strain (and/or possible grade 1 Achilles strain). He was clearly not pain-free, nor was he recovered from a metabolic and vascular standpoint in that calf to Achilles region. So, was the chance at a three-peat really worth risking the health and career of one of the best players in the league?
I guess now that we know the outcome of that decision, all members involved will have to carry that guilt. Just remember therapists, don’t lose your credibility as a health care practitioner with unrealistic outcomes for some championship trophy, financial gain, or anything to inflate your ego. Always do what you clinically know is right for your client, and PLEASE educate patients that no pain no gain is not a real motto.
Recovering from a calf strain or any sports injury requires proper physiotherapy to ensure safe and effective healing. If you’re looking for expert physiotherapy care, clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village offer specialized treatment plans to help athletes and individuals recover fully and prevent future injuries.