Winter is on its way out and spring is almost upon us. With the warmer change in weather, we shake off our desire to hibernate and become more active, doing activities we haven’t done in months! However, we sometimes rush into things too quickly and can put too much pressure on our feet, leading to the development of various foot problems. Orthotics might be the answer for you as they can help change the way your foot makes contact with the ground and can take pressure off high-pressure areas in the foot.
What are Orthotics?
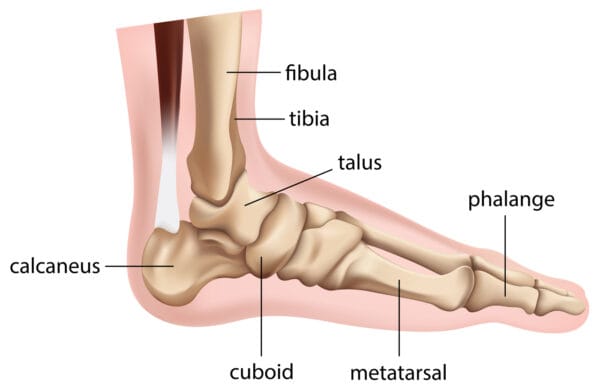
Orthotics are insoles that you use inside your shoes that help rectify biomechanical problems of the foot. They are usually made of a combination of rubber, metal, plastic, leather, or any other synthetic material. Our feet have so many muscles, bones, and joints that abnormal biomechanics of how they’re moving can result in numerous foot problems along with pain in your knee, lower back, hip or leg.
Also read, Physiotherapy Clinics in Mississuaga
How can Orthotics correct foot conditions?
- Orthotics help balance pressure placed on the feet by redistributing the weight appropriately
- They help stabilize the heel
- Support the arch of the feet
- Provides cushioning to delicate and inflamed areas of the feet that arise from too much walking, jogging, running, etc.
There are generally two options when it comes to selecting orthotics: over-the-counter orthotics and custom-made orthotics. Over-the-counter orthotics are available at your local pharmacy and big box store and they can be used with your regular shoes to correct trivial problems. However, because they are prefab, generalized products, there is a possibility that they might make your foot pain worse due to it not being the right kind of support that you need. Custom made orthotics work best because they are tailor-made to correct the problems specific to your feet. Check out our earlier blog on the most popular kinds of Orthotics for further detail.
Also read, Physiotherapy Clinic in Oakville
Here’s a tip
Orthotics can still benefit you even if you don’t suffer from any foot issues but are an active participant in sports. If your foot is dealing with stress and impact, or if you have recently gained weight, orthotics will help you walk better!
Put your best foot forward and in the right direction!
We at Triangle Physiotherapy will quite literally help you get back on your feet! Our Chiropodist can advise you on how to look after your feet and what type of shoes or orthotics to opt for. Book an appointment with our Chiropodist today at any of our 6 clinics located across the GTA: Etobicoke, Oakville, Mississauga, North York, Toronto (King Street West) and Yonge Street. If you have any questions regarding any kind of foot conditions, please call or email us and we will be happy to help you!
Orthotics can be highly effective in managing various foot-related conditions, providing support and alignment to improve comfort and mobility. If you are looking for physiotherapy services to complement your orthotic treatment, there are clinics available in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and customized treatment plans to address your foot health needs.
Who is a Podiatrist? A podiatrist deals with the assessment, diagnosis and treatment of the lower limbs and feet. What is a Chiropodist? A chiropodist deals with the assessment, diagnosis and treatment of the lower limbs and feet. Sound familiar? That is because these two professions are one and the same!
While there may be differences in terms of scope of practice in other areas of the world, in Canada, both podiatrists and chiropodists are qualified to treat patients with arthritis, diabetes, lower limb sports injuries, and various other ailments of the feet. They have received specialized training which allows them to work with patients of all ages and to help the elderly stay mobile and independent. The only practical difference between the two professions, in terms of their scope of practice in Canada, is simply their title.
Also read, Physiotherapy Treatment Etobicoke
Chiropodists can advise patients on how to look after their feet and what type of shoes or orthotics to wear. They can also treat, alleviate and benefit day-to-day foot conditions, such as:
- Thickened, fungal, or ingrown toenails
- Varicose veins
- Athlete’s foot
- Smelly feet
- Dry and cracked heels
- Flat feet
- Bunions
- Heel pain
- Ageing feet
- Blisters
- Gout
- Sports Injuries
Also read, Oakville Physiotherapy Rehab Clinic

Seek help from a Chiropodist for advice or treatment if you have:
- Painful heels or arches
- Thickened or discoloured toenails
- Cracks, cuts, or hardened skin on your feet
- Growths, such as warts
- Scaling or peeling on the soles
- Any other foot condition
Don’t bury your head in the sand and ignore small foot problems! These small “problems” can quickly transform into major issues that can affect the quality of your life. As they say, “Prevention is the best cure“. Patients who make regular check-up appointments can avoid many potential foot problems as Chiropodists are specialists at recognizing problems before they have occurred.
Don’t let your feet problems keep you from stepping into our clinic! Seek the help of our foot specialists at any of our locations in Etobicoke, Oakville, North York, Mississauga & Toronto, and say goodbye to your foot dilemmas!
Addressing foot problems effectively often requires a comprehensive approach that includes professional physiotherapy. If you need expert care for foot-related issues, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide specialized physiotherapy services and personalized treatment plans to help you get back on your feet and improve your overall mobility.
Are your worries all perched on a pillow? And we don’t mean figuratively, but literally, are your worries all about THE PILLOW? Well, you are not in as uncommon a dilemma as you may think. Physiotherapists frequently get queries about pillow-related problems.
Sleeping on the wrong pillow, or one that is too worn out, not only leads to headaches, backaches, and neck cramps but also prevents you from getting a good night’s sleep. Lack of proper sleep can lead to many serious health issues, like obesity, heart disease, diabetes, etc.
It is imperative that you choose the right pillow for yourself but the kind of pillow you should pick will depend on your own unique needs as well. A physiotherapist is the best person to tell you exactly what you need. However, here are a few things that you can keep in mind while making a choice –
- Your usual sleeping position
- The shape and size of your head, neck and back
- Desired softness/firmness of the pillow
- Any neck pain, or backache you may have
- And your budget

Also read, Physiotherapy Clinic in Mississauga
There are a plethora of pillows in the market – cotton, polyester, feather, down, memory foam etc. However, these don’t cater to specific support or pain needs. If you have been injured, or have a particular condition, you will need a pillow that caters best to not just your problem, but also the stage that you are in. There are three main stages –
- Accommodation
- Correction
- Maintenance
For each of these three stages, you will need a specific kind of pillow.
Accommodation Stage:
Specialty pillows that are designed for the ‘Accommodation’ stage, are pillows that bring in comfort and ease by providing support and stabilizing the existing ailment or disorder. Such pillows are often called Displacement pillows and are often recommended by physiotherapists for short-term pain relief after an injury.
Correction Stage:
The next stage of an issue or injury is ‘Correction’. At this stage, a doctor or physiotherapist attempts to find a remedy for the cause of the problem, and thereby correct it. Pillows recommended in this stage are often designed to provide support, and sometimes to even change the sleeping position of the injured or ailing person. There are various ‘Supportive’ pillows to meet different support levels, firmness and neck lobe size needs of different patients. There are also specialized ‘Corrective’ pillows, which can reduce headaches, neck pain, joint pain, and whiplash discomfort and can even improve nerve function. A physiotherapist can tell you what is the ideal Supportive or Corrective pillow you need, based on your health and body needs.
Also read, Physiotherapy Clinic Oakville
Maintenance Stage:
Pillows for the last stage, ‘Maintenance’, help to promote good health by returning and keeping the body in its natural alignment. At this stage maintaining the normal curvature of the neck and spine is of utmost importance. While the normal curvature of one person’s neck and spine may differ from another, there are some general guidelines that a physiotherapist can jot down to help you understand your needs better. Comfort and support are the most important of these.
There are also Aqua pillows, which perform all the 3 functions of a pillow:
- Accommodation: Since water is fluid, a person gets customized accommodation that happens in real time, as the individual changes their position on the pillow.
- Correction: The volume of water determines the firmness and density of the pillow, which means different amounts of water can be utilized to help correct the neck position of different people in different stages of healing.
- Maintenance: Since the volume of water remains constant until changed manually, it helps maintain the neck posture at all times while sleeping.
A lot of people buy a pillow, try it for a few nights, and then feel it isn’t right for them. Sometimes the pillows can be returned, but more often, people end up having a collection of pillows that they have hardly ever used. An Aqua pillow is a huge savior in this aspect, as it can be customized for each individual! The water levels can be modified to best suit the clinical condition, neck shape, and size, and preferred sleeping position of the buyer.
There are also specially designed Orthopaedic pillows for specific conditions like arthritis, fractures, and slip discs. A physiotherapist can enlighten you more about these.
Seek the help of our professionals at any of our locations in Etobicoke, Oakville, North York, Mississauga & Downtown Toronto, and say goodbye to your pillow problems!
Proper posture and support are essential for preventing discomfort and maintaining spinal health. For those seeking professional physiotherapy services to address posture-related issues, consider visiting clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and tailored treatment plans to help you improve your posture and overall well-being.
Summer is here, and with the sun on one’s face and a cool breeze, everyone feels like going out and enjoying some fresh air. Be it an early morning run or a quick swim, a game of tennis with your buddies or you just dribbling the ball all by yourself at the basketball court; this is the season when even the lazy ones find some energy to be active. Kids in particular love to go out and play in the summers. But with an active lifestyle, or an energetic kid, there is always the chance of sports-related injuries or foot fatigue.
Maybe you twisted your ankle while playing tennis? Or did your kid get hurt while playing football? Maybe too much running is affecting your feet? Or your friend is having pain in his or her legs post-cycling?
Also read, Physiotherapy Clinic in Etobicoke
Orthotics might just be the answer to your woes!

The type of Orthotics recommended to you will depend on not just your ailment or injury, but the shape of your feet as well. A physiotherapist can tell you what kind of orthotics you need, by evaluating your injury and the shape of your feet.
The most popular kind of Orthotics include:
- Casual Orthotics – These are inserts or pads that can be worn with regular shoes.
- Custom Orthotics – these are inserts that are specially designed, keeping the shape of your feet and your particular needs in mind.
- Sports Orthotics – these are inserts or pads that help to absorb shock while doing high-impact activities. Be it running, jogging, cycling, or playing a sport. There are even specialized Orthotics that slip easily into athletic shoes for professional athletes.
- Dress Orthotics – These are inserts that can be put into heels and other fashionable shoes, and are particularly made for women.
- Accommodative Footwear – this refers to special footwear, which can accommodate the Orthotics.
Also read, Physiotherapy Oakville
If you don’t have a sports injury but are just very active, orthotics can still come to your aid. But do seek your doctor’s advice before using any kind of orthotics.
At Triangle Physiotherapy our health professionals cater to your needs and specifications. With the help of our professionals, you can figure out what is the best solution for you, based on your activities and the needs of your feet. So visit any of our locations in Etobicoke, Oakville, North York, Mississauga & Downtown Toronto, to stay active with Orthotics!
Orthotics can be crucial for active individuals looking to prevent injuries and enhance performance. If you need professional physiotherapy services to complement your orthotic treatment, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and personalized treatment plans to support your active lifestyle and overall foot health.
Wearing heels may be a fashion statement for some, but for others, it is a work necessity.
Studies have shown that:
- 72% of women wear high heels at some point or the other
- 50% of them wear them at parties
- 39% of them wear them every day
- And 31% of them wear them to work
But wearing heels for a prolonged period of time can lead to multiple issues. So what are the “heel issues” that affect most women? And how can you deal with them?

Also read, Physiotherapy Mississauga
Do your toes hurt and your feet feel numb?
You might have Morton’s Neuroma, commonly known as forefoot pain. People with this ailment most often complain of pain between the 3rd and the 4th toe. Pain between the 2nd and the 3rd toe is less common but also known to happen. This ailment occurs when the nerves between the toes get irritated and inflamed.
Another common issue with wearing high heels is back pain. Constantly wearing very high heels puts stress on the thighs and hip flexors, which in turn puts more pressure on the spine and causes it to curve. The curving of the spine then leads to back pain.
Pain in the knee joints is also an issue that occurs if you wear high heels too often. High heels put too much pressure on knee joints and can create an imbalance in your leg alignment, leading to pain and other issues of the knee joint.
Also read, Physiotherapy Treatment in Etobicoke
Ditching the heels completely will obviously be the best solution. But if you can’t do that, here are some things that you can do –
- Wear heels that are 2 inches or less in height, this will help take off the pressure from your spine and cause less curving.
- If you absolutely must wear very high heels (4 to 6 inches high) one day, wear low to moderate heels the next day. This way your knee joints, spine and thigh muscles will get a break from undue stress.
- If you have forefoot pain, try wearing shoes that are wider around the toes – a shoe with a round or square shape in front is a better choice than a pointy-toed shoe.
- Opt for shoes that have leather insoles so your feet have better grip. Slippery heels cause even more damage to your posture.
- Wear heels for shorter periods of time. The longer you wear high heels, the more damage you cause to your knees and spine.
- Ditch those heels if you are in too much pain. It is better to sit at your desk without your heels on, rather than cringe with pain for the entire day.
- And finally, visit a physiotherapist and do some simple exercises that he or she may suggest to relieve you of your feet, back or knee pain caused by high heels.
At Triangle Physiotherapy our professionals can help you figure out what will be the ideal solution for your ailment. So visit any of our 8 locations of Triangle Physiotherapy clinics – Etobicoke, Oakville, Mississauga, North York, Toronto to heal the issues caused by them heels!
Healing heel pain requires a combination of effective treatments, including physiotherapy to address underlying issues and promote recovery. For professional physiotherapy services to help with heel pain, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and customized treatment plans to support your journey to pain-free mobility.
Yoga has been gaining immense popularity lately, due to the short-term as well as long-term benefits that it provides. Practicing yoga provides a strong spiritual element that offers fitness and flexibility. People suffering from various health disorders can find solutions through yoga, and they may reap the extra benefits yoga provides through living a more stress-free lifestyle as well as with increased fitness.
Yoga for a healthy life
Yoga is an ancient system of health that promotes ‘union’ and connects the body, mind, breath and spirit as one unit, therefore enhancing and promoting an overall balanced lifestyle of health and well-being.
Also read, Best Physiotherpist in Oakville

If practiced regularly the benefits of yoga are numerous. Physically and mentally, yoga may result in:
- Improvement in muscular strength
- Endurance
- Flexibility
- Body awareness
- Circulation
- Digestion
- Hormonal balance
- Normalizing blood pressure
- Weight loss
- Pain relief
- Alertness
- Concentration
- Improvement in sleep
- And much, much more!
It is believed that we only have a limited number of breaths in each life. Hence,yoga is believed to stretch our lives out a bit longer by taking slow and deep breaths.
Also read, Physiotherapy Treatment in Mississauga
Research has also suggested that yoga improves social and occupational functioning in schizophrenic patients.
Styles:
Some styles of yoga emphasize breathing and meditation, with limited activity; some styles emphasize form and alignment through postures, some are about a serious workout and flow, & some are all about relaxation.
Not a competition:
Don’t try a posture that you are uncomfortable with; don’t let someone else push you into something that you don’t want to do; and don’t think that you have to compete with yourself or others to achieve a posture.
Yoga is not about competition or feeling the burn. However, a little discomfort is to be expected. There is a huge difference between pain and discomfort, and most people mistake one for the other, especially when they are new to yoga practice.
Consult A Physiotherapist
At Triangle Physiotherapy, we work with the help of your medical history and assess how yoga may help guide your health in the right direction. All you need to do is overlook your anxieties related to your health, and feel free to contact any of our five locations for an in-depth consultation.
Incorporating yoga into your routine can enhance flexibility, strength, and overall well-being, and combining it with physiotherapy can optimize these benefits. For those seeking professional physiotherapy services to complement their yoga practice, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and tailored treatment plans to support your physical health journey.
Massage therapy has a positive effect on a plethora of medical conditions. It rejuvenates both your mind and muscles. Everyone experiences pain, the only difference is some continue to suffer and some proactively seek pain relief through massage therapy. Our skin is the largest organ in our body. The skin interfaces with the environment and is the first line of defense from external factors. Taking good care of your skin through massage therapy will help keep your skin healthy and muscles rejuvenated. Massage therapy is regarded as one of the oldest healthcare professions. Massage therapy is not just for the skin and muscles, it can also help to reduce high blood pressure, lower chances of depression and relieve headaches.

Also read, Physiotherapy Etobicoke
Healing from a car accident injury through massage therapy
Car accidents can cause a variety of physical problems, and many people seek physiotherapy and/or massage therapy for relief from whiplash and other aches and pains. Massage therapy has the potential for facilitating health, wellness, and injury recovery from car accidents.
-
Massage therapy can relieve Whiplash
Whiplash injuries are common in car and sports accidents. People who get whiplash may experience pain, stiffness, and poor range of motion, among other symptoms. Some people may feel mental or emotional symptoms such as loss of memory or focus, insomnia, and depression. If you have whiplash, ask your physician about adding massage to your physical therapy regimen, as the combination could help speed up your recovery.
- Massage Therapy for Knee Injuries
People in car accidents often injure their knees (though not as often as heads, necks, and spines). Statistics show car crash victims often injure their Anterior Cruciate Ligaments (ACLs), as do many athletes. Massage therapy has been shown to provide pain relief and healing for people with a wide variety of knee problems.
Also read, Physiotherapy Clinic in Oakville
- Massage therapy helps to recover from Immediate emotional trauma
If you’re in a car crash, you may suffer emotionally even if you do not sustain any physical injuries. Massage therapy, especially within several hours of an auto accident, can help people recover their emotional balance.
We all suffer from adverse health effects both psychological and physical, and stress is one of the important factors to look after. A massage can help reduce everyday stress by helping muscles to relieve and relax through the pressure points manually worked on by one of our experienced massage therapists.
Our registered massage therapists at Triangle Physiotherapy are happy to assist you with any questions pertaining to your health goals and guide you on the road to recovery. Adding massage therapy to your healthcare/recovery plan will provide natural relief without the aid of painkillers. Living pain-free naturally is our goal, and at Triangle Physiotherapy, we will guide you every step of the way.
Massage therapy is a great way to relax, reduce muscle tension, and promote overall well-being. For those looking to combine massage therapy with physiotherapy services, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and personalized treatment plans to help you achieve optimal health and relaxation.
What are orthotics?
Orthotics are custom-made inserts that are worn inside your shoe to control abnormal foot function.
Orthotics solve a number of biomechanically related problems, for example, ankle and knee pain, pelvis, hip, and spinal pain. This is achieved by preventing misalignment of the foot, which significantly alters the way in which the bones move within their joints.
Also read, Physiotherapy Rehab Clinic in Mississauga
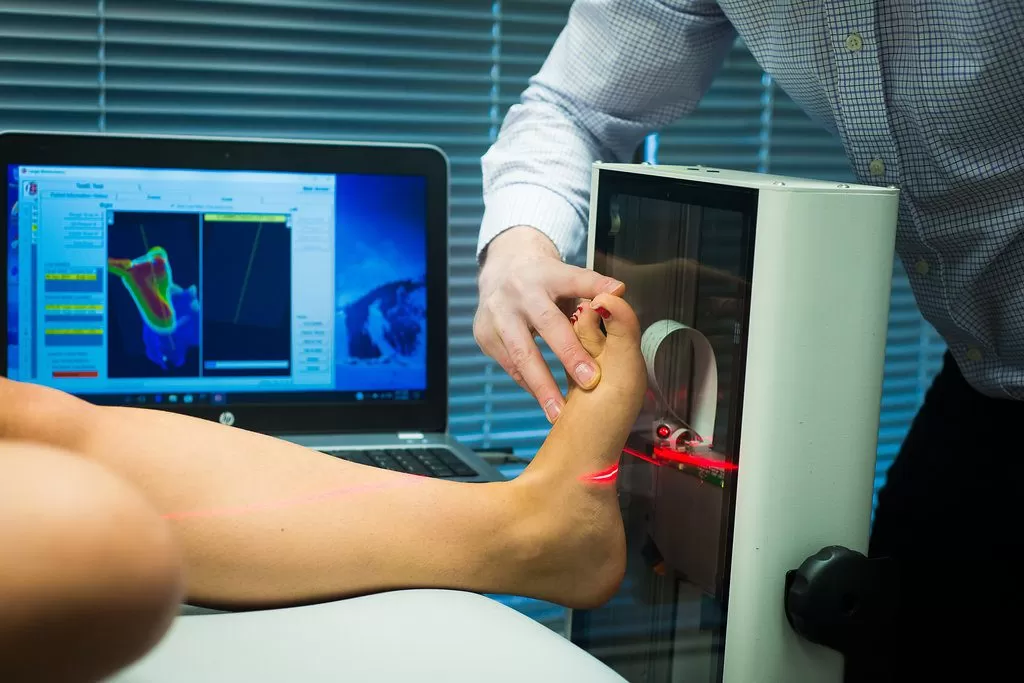
How are custom orthotics made?
The process starts with the chiropodist, chiropractor, or physiotherapist conducting a Biomechanical Gait analysis on a tablet that records your gait pattern & explaining the results to you. The chiropodist, chiropractor, or physiotherapist may also take a 3D cast of your feet in a foam box.
The orthotics are then custom-manufactured in the lab based on your foot impressions & scan.
Once the orthotics are made & delivered to the clinic, the chiropodist, chiropractor or physiotherapist will have you come in for a fitting & explain to you the wear & care of the orthotics.
Also read, Physiotherapy Clinic in Etobicoke
Why choose Triangle Physiotherapy for your custom orthotics?
- State-of-the-art technology
- Experienced chiropodists, chiropractors or physiotherapists trained in Biomechanical Assessments & Orthotic Prescription
- Lifetime warranty on the orthotics*
- Assistance with sending your claims to your insurance.
Click HERE to book an appointment with a chiropodist at one of our eight locations.
- Orthotics Etobicoke – Triangle Physiotherapy Etobicoke
- Orthotics Oakville – Triangle Physiotherapy Oakville
- Orthotics North York – Triangle Physiotherapy North York
- Orthotics Mississauga – Triangle Physiotherapy Mississauga
- Orthotics Downtown Toronto – Triangle Physiotherapy King West
- Orthotics Yonge and Eglinton – Triangle Physiotherapy Lawrence Park
- Orthotics Toronto – Triangle Physiotherapy Queens Quay
- Orthotics Mississauga – Triangle Physiotherapy Erin Mills
Orthotics are essential for providing support, alignment, and pain relief for various foot and lower limb conditions. If you are looking for professional physiotherapy services to complement your orthotic treatment, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and personalized treatment plans to help you achieve optimal foot health and mobility.
Pacifying the Pain – All about Patella Tendon Tears
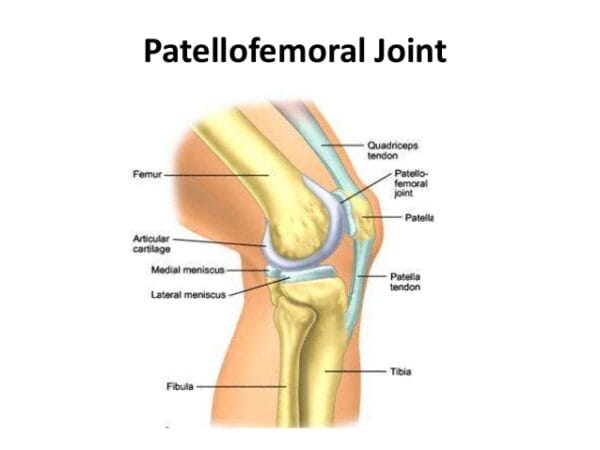
Despite it being named a “Tendon”, the patella tendon is both a ligament and a tendon. It connects to two different bones, the patella and the tibia. The patella tendon works in unison with the quadricep muscles and quadriceps tendons allowing them to straighten the knee. The tear within the patella tendon is either partial or complete and can be a disabling injury:
- Partial tear- More frayed and not complete, (think of a rope that is not completely torn)
- Complete Tear- The tissue is torn into two complete pieces
There are numerous causes that can contribute to the tear of a patella tendon:
- Falls
- Jumping
- Patellar tendonitis- inflammation of the patellar tendon thus weakening the tendon, causing small tears.
- Chronic disease – Chronic renal failure, rheumatoid arthritis, Diabetes mellitus & metabolic disease, etc.
- Infection
- Surgery
Also read, Best Physiotherapy Clinic Mississauga
Most patients have stated that they had felt a popping or tearing sensation when the patella tendon has torn. Additional symptoms recorded were:
- Indentation at the spot where the patella tendon is located
- Bruising
- Tenderness
- Cramping
- Shift of the kneecap to thigh, due to un-attachment
- Difficulty walking due to weakness in the knee
Also read, Physiotherapy Oakville
Once the initial pain and swelling has subsided, physiotherapy treatments can be started. Physiotherapy can restore strength and range of motion. Depending on the intensity of the injury, a brace may need to be worn. While the brace is worn, straight leg exercises are often prescribed to strengthen the quadriceps muscles. As the patellar tendon heals, eventually the brace may be removed, allowing the patient to move freely with a greater range of motion, with more exercises being put into use as healing progresses.
Recovery from patellar tendon tears is possible, and most individuals are able to return to work and regular activities. Even though patients may feel stiffness in the region after recovery, most regain nearly equal motion compared to the uninjured leg. At Triangle Physiotherapy, we are able to dispense custom-fit braces to aid in the recovery of patellar tendon tears. For more information visit our custom braces page at: http://www.trianglephysiotherapy.com/services/custom-bracing
Recovering from a patella tendon tear requires a comprehensive approach, including effective physiotherapy to restore strength and mobility. If you’re seeking professional physiotherapy services for tendon injuries, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and customized treatment plans to help you recover fully and get back to your active lifestyle.
What exactly are shin splints? Are they treatable?
Shin splints are a condition characterized by damage and inflammation of the connective tissue joining muscles to the inner shin bone (tibia). Shin splints are known by many different names such as: Medial Tibial Tenoperiostitus, MTSS, Medial Tibial Stress Syndrome, Tenoperiostitus of the Shin, Inflammatory Shin Pain, Traction Periostitis, and Posterior Shin Splint Syndrome.
Several muscles lie at the back of the lower leg, and are collectively known as the calf muscles. The tibialis posterior, flexor digitorum longus, flexor hallicus, and soleus are muscles that lie deep within the calf and attach to the inner border of the tibia. Connective tissues are responsible for attaching these muscles to the tibia known as the tenoperiosteum. Every time the calf contracts, it pulls on the tenoperiosteum. When the tension becomes forced too much or is repeated frequently, the damage is caused to the tenoperiosteum. The results are inflammation and pain. Shin splints can also occur in combination with other pathologies that cause shin pain such as compartment syndrome and tibial stress fractures.
Patients who suffer from shin splints experience pain along the inner border of the shin. In other cases, the patient may experience an ache or stiffness along the inner aspect of the shin that increases with rest (typically and night or first thing in the morning). Areas of muscle tightness, thickening, or lumps may also be felt in the same area of pain.

There are several factors that predispose patients to shin splints:
• Excessive training or exercise
• Poor foot posture (especially in patients with flat feet)
• Inappropriate footwear
• Inadequate warm-up• Training on hard or inappropriate surfaces
• Muscle weakness (especially in calve muscles)
• Tightness in specific joints (such as ankle)
• Tightness in specific muscles (calves especially)
• Poor lower limb biomechanics
• Poor training techniques or methods
• Leg length differences
• Poor balance
• Being overweight
• Deconditioning
• Poor core stability
Also read, Physiotherapy Clinic in Oakville
Physiotherapy treatment for patients with shin splints is vital to speed up the healing process. Physiotherapy will ensure the most optimal outcome and reduce the likelihood of recurrence. Treatment may comprise of the following:
- Deep tissue massage
- Joint mobilization
- Dry needling
- Electrotherapy
- PNF stretches
- Arch support taping
- The use of orthotics or shock-absorbing insoles
- Crutches
- Biomechanical correction
- Ice or heat treatment
- Exercises to improve flexibility, balance, strength, and core stability
- Activity modification advice
- Anti-inflammatory advice
- Footwear advice
- Weight loss advice where appropriate
Also read, Physiotherapy Clinic in Mississauga
If you happen to suffer from shin splints and you are looking for a way to relieve pain, stress, and improve overall health, try adding physical therapy to a routine wellness plan. Our physiotherapists at Triangle Physiotherapy can be a powerful ally when combating daily stress, muscle pain, and general health issues when it comes to shin splints. Not only does physical therapy relieve pain, increase energy levels, and improve overall physical and mental performance, it prevents further injuries.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy can play a crucial role in treating and preventing shin splints by addressing muscle imbalances and improving biomechanics. If you’re looking for professional physiotherapy services to help manage shin splints, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and tailored treatment plans to support your recovery and enhance your running or athletic performance.