Winter is here and the snow is around the corner. The season for skiing is upon us. Whether you are a novice skier or experienced in the sport, there is always a possibility of an injury. This article talks about common skiing injuries and how you can recover from them.

What are some common snow sports injuries?
Some common injuries sustained during skiing are:
Head
- Concussion
- Traumatic brain injury
Neck & Shoulders
- Whiplash
- Fracture
- Torn rotator cuff
- Shoulder dislocation
Back & Spine
- Herniated disks
- Lower back pain
Hand
- Skier’s thumb
- Wrist sprain
- Finger fracture
Knees & Legs
- ACL/PCL rupture
- Meniscus injury
- Fracture
How can I protect my knees while skiing?
Using properly adjusted bindings, maintaining proper ski technique, and conditioning exercises to strengthen the muscles around the knee can help protect against knee injuries.
What is “snowboarder’s fracture”?
Snowboarder’s fracture refers to a fracture of the lateral process of the talus bone in the ankle, usually caused by an inversion injury when landing from a jump.
Are head injuries common in skiing?
Head injuries can occur in skiing, especially in the absence of helmets. Wearing a properly fitted helmet significantly reduces the risk of head injuries.
How do I know if I have a concussion from skiing?
Symptoms of a concussion may include headache, dizziness, nausea, confusion, sensitivity to light, and memory problems. If you suspect a concussion, it’s crucial to seek medical attention.
What do I do after I get injured while skiing?
No matter how minor the injury, it is advisable to seek a doctor or physiotherapist’s advice to make sure it does not get worse. A physiotherapist can assess the extent of your injury. Follow their advice and recommendations for treatment.
When should I seek medical help for a ski injury?
Seek medical help if you experience severe pain, swelling, inability to bear weight, persistent joint instability, or any symptoms of a head injury or concussion. It’s essential not to ignore potentially serious injuries.
How do I book an appointment with a physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Recovering from a skiing injury requires targeted physiotherapy to regain strength and mobility. Triangle Physiotherapy offers specialized services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team is dedicated to guiding you through a safe and effective recovery process.”
Shockwave therapy, also known as extracorporeal shock wave therapy (ESWT), is a non-invasive medical treatment that uses acoustic waves to stimulate healing in various musculoskeletal conditions, including plantar fasciitis. Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes.

Here’s how shockwave therapy is typically used for plantar fasciitis:
- Mechanism of Action:
- Shockwave therapy works by delivering high-energy shockwaves to the affected area. These shockwaves create microtrauma in the tissue, which triggers the body’s natural healing response.
- The treatment is thought to stimulate blood flow, promote tissue regeneration, and reduce inflammation.
- Procedure:
- During the procedure, a gel is applied to the skin of the affected foot to help transmit the shockwaves.
- A handheld device is then used to deliver controlled shockwaves to the targeted area, typically the heel or the sole of the foot.
- Number of Sessions:
- The number of shockwave therapy sessions required can vary.
- Some individuals may experience relief after just one session, while others may require additional treatments.
- Post-Treatment:
- After the procedure, patients may experience temporary soreness or discomfort, but this usually subsides within a few days.
- It’s important to follow any post-treatment instructions provided by the healthcare provider, which may include rest, ice, and avoiding certain activities.
- Effectiveness: The use of shockwave therapy is often considered when conservative treatments, such as rest, stretching exercises, orthotics, and anti-inflammatory medications, have not provided sufficient relief.
It’s crucial to note that while shockwave therapy may be beneficial for some individuals, it may not be suitable for everyone. Patients should consult with their healthcare provider to determine the most appropriate treatment approach based on their specific condition and medical history.
Who can provide Shockwave Therapy at Triangle Physiotherapy?
Shockwave Therapy can be provided at our clinics by a physiotherapist, a chiropractor or a massage therapist.
Will Shockwave Therapy be covered by my insurance?
Yes, shockwave therapy will be covered depending on the healthcare practitioner providing the service. For example, if you are seeing a physiotherapist for shockwave therapy, it will be covered under your physiotherapy coverage.
How do I book an appointment with a physiotherapist or chiropractor near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Shockwave therapy is an effective treatment for plantar fasciitis, helping to reduce pain and promote healing. Triangle Physiotherapy provides expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists are here to help you find relief from plantar fasciitis and get back on your feet.”
Back pain is one of the most common ailments we see in our practice.

Here are some self-care measures you can consider to manage or prevent recurrence:
- Rest: Give your back a break by avoiding activities that may exacerbate the pain. However, avoid prolonged bed rest, as it can lead to stiffness and muscle weakness. Gentle movement and stretching are usually better than complete immobility.
- Ice and Heat: Apply ice packs to the affected area for the first 48 hours to reduce inflammation, then switch to heat therapy (e.g., heating pads) to relax tight muscles. Use each for 15-20 minutes at a time.
- Over-the-Counter Pain Relief: Non-prescription pain relievers such as ibuprofen (Advil) or acetaminophen (Tylenol) can help alleviate pain and reduce inflammation. Follow the recommended dosage and consult a healthcare professional if you have concerns.
- Exercise: Gentle, low-impact exercises can help strengthen your back and improve flexibility. Activities like swimming, walking, or yoga can be beneficial. Consult a physical therapist for guidance on appropriate exercises.
- Posture: Maintain good posture when sitting and standing to reduce strain on your back. Use ergonomic chairs and accessories if needed, and avoid prolonged periods of sitting.
- Proper Lifting Technique: When lifting heavy objects, bend at your knees and hips instead of your waist, and use your legs to lift while keeping the object close to your body.
- Core Strengthening: Strengthening your core muscles (abdominals, obliques, and lower back) can provide better support for your spine. Pilates and specific core exercises can help with this.
- Sleep: Ensure you have a comfortable mattress and pillow that support your spine. Sleeping on your side with a pillow between your knees can help maintain proper alignment.
- Stress Reduction: Stress can contribute to muscle tension and pain. Techniques such as meditation, deep breathing exercises, and relaxation techniques may help manage stress.
- Weight Management: Maintaining a healthy weight can reduce the strain on your back and decrease the risk of back pain.
- Physiotherapy: A physical therapist can provide personalized exercises and techniques to address your specific back pain issues.
- Chiropractic Care or Massage Therapy: Some people find relief through chiropractic adjustments or therapeutic massages. Consult with professionals in these fields to see if it’s appropriate for your condition.
- Avoid Smoking: Smoking can impair blood flow to the spine and hinder the healing process.
If your back pain persists, worsens, or is accompanied by other concerning symptoms (such as numbness, tingling, weakness, or loss of bladder or bowel control), seek immediate medical attention. Always consult a healthcare provider before starting any new exercise or treatment regimen, especially if you have underlying health conditions or are taking medications. They can provide a more accurate diagnosis and recommend the best treatment options for your specific situation.
How do I book an appointment with a physiotherapist or chiropractor near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Relieving back pain requires a comprehensive approach that includes targeted physiotherapy. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you find effective solutions to alleviate your back pain and improve your quality of life.”
You should consider seeing a physiotherapist when you’re experiencing pain or discomfort, or have mobility issues that affect your daily activities and quality of life. Physiotherapists are healthcare professionals trained to diagnose and treat a wide range of musculoskeletal and movement-related conditions.

Here are some situations in which you might want to consult a physiotherapist:
- Pain and Discomfort: If you’re experiencing persistent pain, whether it’s in your joints, muscles, or any part of your body, a physiotherapist can help identify the root cause and provide treatment to alleviate the pain.
- Injury Recovery: If you’ve suffered an injury, such as a sprain, strain, fracture, or sports-related injury, a physiotherapist can guide you through a rehabilitation program to regain strength, flexibility, and function.
- Mobility Issues: If you’re having trouble moving, walking, or performing daily activities due to stiffness or limited range of motion in your joints, a physiotherapist can develop exercises and techniques to improve your mobility.
- Post-Surgery Rehabilitation: After surgeries, such as joint replacements or orthopedic procedures, a physiotherapist can help you recover faster and regain normal function through targeted exercises and therapies.
- Chronic Conditions: Physiotherapy can help manage chronic conditions like arthritis, fibromyalgia, or chronic back pain by improving muscle strength, joint flexibility, and overall functional capacity.
- Postural Problems: If you have poor posture that’s leading to discomfort or pain, a physiotherapist can assess your posture and provide guidance on how to improve it.
- Neurological Conditions: Physiotherapists also work with individuals who have neurological conditions such as stroke, multiple sclerosis, or Parkinson’s disease to improve movement, balance, and coordination.
- Preventive Care: Even if you’re not currently experiencing pain, a physiotherapist can provide guidance on exercises and habits that can help prevent future injuries and maintain overall musculoskeletal health.
- Sports Performance Enhancement: Athletes can benefit from physiotherapy to improve their performance, prevent injuries, and receive specialized training techniques.
- Pregnancy and Postpartum Care: Physiotherapists can assist pregnant individuals with managing pain and discomfort associated with pregnancy and can provide exercises to help with postpartum recovery.
It’s important to note that physiotherapists work closely with other healthcare professionals, and they will often collaborate to provide you with comprehensive care. If you’re unsure whether seeing a physiotherapist is appropriate for your situation, consider consulting your primary care physician or a medical professional for guidance.
At Physiotherapy Oakville, our team works hand-in-hand with doctors, specialists, and other healthcare providers to ensure you receive the most comprehensive and effective treatment. Scientific studies have shown that a multidisciplinary approach to care can significantly improve patient outcomes. By joining Physiotherapy Oakville, you benefit from a coordinated and collaborative healthcare experience that addresses all aspects of your condition, providing you with a well-rounded and practical path to recovery.
How do I book an appointment with a physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Knowing when to see a physiotherapist can make a significant difference in your recovery and overall well-being. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team is here to help you address any physical concerns early on and guide you toward optimal health.”
Shoulder pain can vary in its cause and severity, and whether it goes away on its own depends on several factors. Here are some considerations:
- Cause of Shoulder Pain
- Acute vs. Chronic Pain
- Severity of Pain
- Age and Health Status
- Activity Level
- Professional Evaluation
- Treatment Options

What are some Common Shoulder Problems and how to treat them?
Shoulder problems can encompass a range of conditions and injuries. Here are some common shoulder problems and some general guidelines on how they are typically treated:
- Rotator Cuff Tears:
- Treatment can range from rest and physiotherapy for partial tears to surgical repair for complete tears.
- Tendinitis (Rotator Cuff Tendinitis):
- Rest, ice, anti-inflammatory medications, and physiotherapy are common initial treatments. Severe cases may require corticosteroid injections.
- Bursitis (Shoulder Bursitis):
- Similar to tendinitis, treatment includes rest, ice, anti-inflammatory drugs, and physiotherapy. In some cases, corticosteroid injections may be used.
- Frozen Shoulder (Adhesive Capsulitis):
- Physiotherapy and stretching exercises are often recommended. Severe cases may require manipulation under anesthesia or surgery.
- Shoulder Impingement:
- Rest, ice, physiotherapy, and modifications to activity are typical treatments. Injections or surgery may be necessary in severe cases.
- Labral Tears (SLAP Tears):
- Non-surgical options include rest and physiotherapy. Severe cases may require arthroscopic surgery to repair the labrum.
- Shoulder Instability (Shoulder Dislocation):
- Initial treatment includes immobilization and physiotherapy. Surgical options may be considered for recurrent dislocations.
- Arthritis (Osteoarthritis or Rheumatoid Arthritis):
- Management includes pain relief with medications, physiotherapy, and lifestyle modifications. In severe cases, joint replacement surgery may be recommended.
- Fractures (Clavicle, Humerus, or Scapula):
- Treatment depends on the type and severity of the fracture. Options include immobilization with a cast or sling, surgery, and physiotherapy.
- AC Joint Separation:
- Mild cases may require rest and physiotherapy, while severe cases may require surgery.
- Nerve Compression (Thoracic Outlet Syndrome):
- Treatment may involve physiotherapy, posture correction, and occasionally surgery to relieve compression on nerves and blood vessels.
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Shoulder pain can be persistent and may not resolve on its own without proper care. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists can help you address the root causes of your shoulder pain and guide you towards effective recovery.”
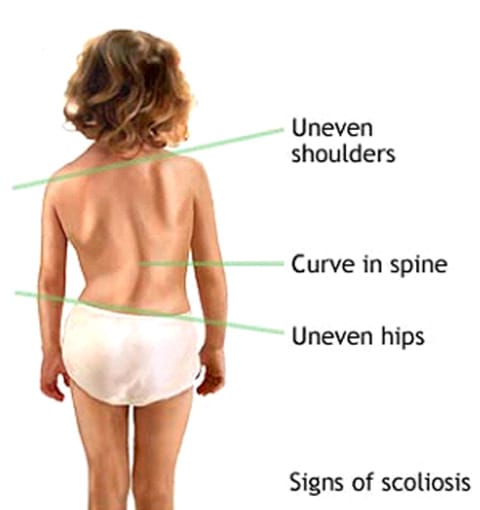
Physiotherapy can play a role in managing scoliosis, but it is important to understand that it is not a cure for the condition. Scoliosis is a complex spinal deformity characterized by an abnormal curvature of the spine. The treatment of scoliosis depends on various factors, including the severity of the curvature, the age of the individual, and other medical considerations.
How do I know if I have scoliosis?
While it’s possible to have scoliosis without experiencing noticeable symptoms, there are some signs and symptoms that may indicate the presence of scoliosis.
- Uneven Shoulders: Stand in front of a mirror with your arms hanging naturally at your sides. If one shoulder appears higher than the other, it could be a sign of scoliosis.
- Uneven Hips: When standing, if one hip appears to be higher or more prominent than the other, it may be a sign of scoliosis.
- Asymmetrical Waist: An uneven waistline, where one side of the waist is higher or more pronounced than the other, can be a sign of scoliosis.
- Leaning to One Side: Some people with scoliosis may unconsciously lean to one side when standing or walking.
- Visible Spinal Curvature: In more severe cases, you or someone else may notice a visible curve or twist in the spine when looking at your back. This is often more noticeable when bending forward at the waist.
- Back Pain or Discomfort: Scoliosis can sometimes cause back pain, particularly if the curvature is significant or if it progresses rapidly.
- Clothing Fit: You may notice that your clothing doesn’t hang evenly or that one side of your shirt or dress appears longer than the other.
- Uneven Leg Length: Scoliosis can sometimes give the appearance of uneven leg lengths due to pelvic rotation caused by the spinal curvature.
How is Scoliosis diagnosed?
Scoliosis is typically diagnosed through a combination of methods, including a physical examination, medical history assessment, and imaging studies. Here is a step-by-step explanation of the diagnosis process:
- Medical History and Symptom Assessment: The first step in diagnosing scoliosis involves discussing your medical history and any symptoms you may be experiencing with a healthcare provider. They will ask about any family history of scoliosis, previous medical conditions, and any pain or discomfort you may have noticed.
- Physical Examination: A physiotherapist, will conduct a physical examination. During this examination, they will:
- Ask you to bend forward at the waist with your feet together and arms hanging down. This helps the healthcare provider assess the curvature of your spine. They will look for any asymmetry or abnormal curvature.
- Examine your back while you are standing to check for any signs of scoliosis, such as uneven shoulders, hips, or a noticeable curve in the spine.
- Measure the degree of spinal curvature using a scoliometer, a specialized instrument that quantifies the angle of spinal rotation.
- Imaging Studies: If the physical examination suggests the presence of scoliosis or if there are other concerning factors, imaging studies may be ordered to confirm the diagnosis and assess the severity of the curvature. Common imaging techniques used include:
- X-rays: X-rays provide detailed images of the spine and are used to measure the angle of the spinal curvature (Cobb angle). X-rays are essential for determining the severity of scoliosis and planning treatment.
- MRI (Magnetic Resonance Imaging): In some cases, an MRI may be recommended, especially if there are concerns about spinal cord compression or underlying spinal abnormalities. MRI provides detailed soft tissue images.
- Additional Evaluation: Depending on the findings from the physical examination and imaging studies, additional tests or evaluations may be necessary. This can include assessing lung function if the scoliosis is severe, as it can affect respiratory function in some cases.
How can physiotherapy help Scoliosis?
Physiotherapy can play a beneficial role in the management of scoliosis, particularly in helping to improve posture, reduce pain, and enhance overall function. While physiotherapy cannot cure scoliosis, it can be a valuable component of a comprehensive treatment plan. Here are ways in which physiotherapy can help individuals with scoliosis:
- Pain Management: Many individuals with scoliosis experience back pain and discomfort. Physiotherapists can employ various techniques to alleviate pain, including manual therapy, soft tissue mobilization, and modalities like heat or ice therapy.
- Postural Improvement: Physiotherapists can work with individuals to improve their posture. Proper posture can help prevent the progression of scoliosis and reduce the strain on the spine and surrounding muscles.
- Muscle Strengthening: Specific exercises are prescribed to strengthen the muscles around the spine. Strengthening these muscles can provide better support for the spine and potentially help improve spinal alignment.
- Range of Motion: Physiotherapy can help maintain or improve the range of motion in the spine and other affected joints. This is important for overall mobility and function.
- Breathing Exercises: In cases where scoliosis affects respiratory function, physiotherapists can teach breathing exercises to improve lung capacity and respiratory function.
- Core Stability: Core strengthening exercises can enhance the stability of the spine and help individuals maintain better posture.
- Patient Education: Physiotherapists can educate individuals with scoliosis on their condition, treatment options, and self-management techniques. This education empowers individuals to take an active role in their care.
- Bracing Support: For individuals prescribed with a brace to manage scoliosis, physiotherapists can provide guidance on wearing and adjusting the brace properly to achieve the best results.
- Emotional Support: Coping with scoliosis, especially during adolescence, can be emotionally challenging. Physiotherapists can provide emotional support and help individuals develop a positive body image and self-esteem.
- Collaboration with Other Healthcare Providers: Physiotherapists often work as part of a multidisciplinary team that includes orthopedic surgeons, chiropractors, and other healthcare professionals. They collaborate to ensure comprehensive care for individuals with scoliosis.
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Scoliosis can be managed effectively with the right physiotherapy approach. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you develop a personalized treatment plan to manage scoliosis and improve your quality of life.”
Getting the most out of your physiotherapy appointment involves effective communication, preparation, and active participation.

Here are some tips to help you make the most of your physiotherapy session:
- Be Prepared:
- Write down your symptoms, concerns, and questions beforehand.
- Note any changes in your condition since your last appointment.
- Bring relevant medical reports, imaging results, or a list of medications you’re taking.
- Arrive Early:
- Arriving a few minutes early will give you time to complete any necessary paperwork and relax before your session.
- Effective Communication:
- Clearly describe your symptoms, their onset, severity, and any factors that worsen or alleviate them.
- Be honest about your lifestyle, activities, and habits that could impact your condition.
- Ask questions if you don’t understand something. Your physiotherapist is there to help you.
- Set Clear Goals:
- Discuss your goals with your physiotherapist. What do you want to achieve through physiotherapy? This could be pain relief, improved mobility, or functional goals.
- Follow Instructions:
- Listen carefully to the advice and instructions provided by your physiotherapist.
- Follow the recommended exercises, stretches, or home-care routines diligently.
- Ask Questions:
- Don’t hesitate to ask questions about your condition, treatment plan, exercises, or any concerns you might have.
- Understand Your Treatment Plan:
- Make sure you understand your treatment plan, including the goals, expected outcomes, and duration of treatment.
- Take Notes:
- Jot down key points, exercises, or recommendations during the session so you can refer back to them later.
- Feedback:
- Provide feedback to your physiotherapist about your progress and any changes you’ve noticed.
- Be Patient:
- Understand that progress may take time. Don’t get discouraged if you don’t see immediate results.
- Follow Up:
- Schedule follow-up appointments as recommended by your physiotherapist to monitor your progress and make adjustments to your treatment plan.
- Hygiene and Attire:
- Wear comfortable clothing that allows easy access to the area being treated.
- Maintain good hygiene, especially if your session involves physical contact.
- Engage Actively:
- Participate actively during the session. Follow your physiotherapist’s instructions and give your best effort during exercises.
Remember, your physiotherapist is there to help you achieve your goals and improve your health and well-being. By being proactive, engaged, and open in your communication, you can maximize the benefits of your physiotherapy appointments.
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Maximizing the benefits of your physiotherapy appointment is essential for a successful recovery. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists are committed to helping you achieve your health goals with personalized care and guidance.”
Physiotherapy can be beneficial for individuals with arthritis. Arthritis is a condition that involves inflammation and stiffness of the joints, leading to pain and reduced mobility. Physiotherapy aims to improve joint function, alleviate pain, and enhance overall quality of life through various techniques and exercises. Here are some frequently asked questions (FAQs) about physiotherapy and its role in managing arthritis:
What is arthritis or osteoarthritis?

- Arthritis, also known as Osteoarthritis (OA), is one of the most common causes of a decrease in mobility and an increase in disability among older adults. It is a common condition affecting the joints, most often the knees, hips, lower back, neck, and fingers.
- In a typical joint, there is a smooth layer of cartilage over the surfaces of the bones. This cartilage has several purposes, including distributing weight evenly during movement to minimize friction and absorb any shock.
- In OA, this cartilage breaks down and causes bones to rub against each other, producing pain and, therefore, disuse of that joint. Muscle weakness due to decreased use is a commonly associated issue in osteoarthritis, which affects function and mobility in many ways.
Can physiotherapy help with the pain?
Yes, physiotherapy can help manage arthritis pain by utilizing techniques such as manual therapy, joint mobilization, and soft tissue manipulation. These techniques can help reduce pain and improve joint function.
Can physiotherapy prevent joint deformities in arthritis patients?
Early intervention through physiotherapy can help prevent or minimize joint deformities by maintaining joint function, improving muscle balance around the affected joints, and promoting proper biomechanics.
Can physiotherapy reduce the need for medication?
In some cases, successful physiotherapy can lead to reduced reliance on pain medications or other arthritis-related drugs. However, this should always be discussed with a healthcare professional.
How long does it take to see results from physiotherapy for arthritis?
The timeline for seeing results can vary based on the severity of arthritis, the individual’s response to treatment, and consistency in following the physiotherapy program. Some individuals may experience improvements within a few weeks, while others might require more time.
Is physiotherapy suitable for all types of arthritis?
Physiotherapy can be beneficial for various types of arthritis, including osteoarthritis, rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis. However, the approach may vary depending on the specific type and individual needs.
At Physiotherapy Oakville, our experienced physiotherapists create customized treatment plans tailored to the type of arthritis you have and your unique requirements. Scientific research supports the effectiveness of physiotherapy in managing arthritis symptoms, reducing pain, and improving joint function. By joining Physiotherapy Oakville, you can take advantage of evidence-based treatments and individualized care strategies that help you manage arthritis more effectively, enhance your quality of life, and maintain your mobility and independence.
How can strength training help arthritis?
- The strength in the muscles surrounding a joint is directly related to the progression of osteoarthritis. Studies show that muscle weakness after decreased use of the joint due to pain can actually make OA progress faster, further exacerbating the disability. In normal aging, there can already be some underlying muscle wasting or weakness, making function even more difficult.
- The goals of strength training are to decrease pain, protect against worsening of the condition, and improve self-efficacy and general health/well-being. Below are some ways strength training can help OA:
- Improve joint mechanics by offloading the join with stronger muscles
- Reduce joint pain by normalizing neural firing patterns
- Decrease cartilage degeneration by decreasing inflammatory chemicals in the body that breakdown cartilage
- Decrease depression and anxiety by increasing self-efficacy, independence, and mobility
- Older adults without existing osteoarthritis can lower their chances of getting it with increased strength!
What does the evidence show?
- Pain decreased by almost 50% in as little as 2 months of strength training
- Improve walking distance by 30-45%
- Significantly decrease progression of OA in the long-term, up to 30 months after beginning strengthening exercise
What are some of the changes I can expect to see after seeing a physiotherapist?
Changes you will see!
- Easier to go up and down the stairs
- Less pain during squatting and kneeling tasks
- Ability to walk longer and faster, allowing you to enjoy outdoor activities
- Better mood and decreased emotional stress
What are some exercises to do for arthritis?
Examples of exercises
- Swimming
- great for taking the weight of your joints but challenging your muscles against the weight of the water!
- Squatting up and down from a chair
- You do this every day and it will translate directly into easier activities of daily living!
- Biking
- Another very functional, strengthening exercise that also incorporates aerobic training to increase overall health
- Single leg balance
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Physiotherapy can play a significant role in managing arthritis by improving joint function and reducing pain. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you develop a personalized treatment plan to manage arthritis and enhance your quality of life.”
✔️ Physiotherapy absolutely works!
Physiotherapy is a legitimate and effective healthcare practice that aims to improve and restore physical function and mobility, reduce pain, and enhance overall well-being. It is commonly used to treat a wide range of conditions, injuries, and illnesses. Physiotherapists, also known as physical therapists, are trained healthcare professionals who use various techniques, exercises, and modalities to help patients recover from injuries, manage chronic conditions, and improve their physical capabilities.
What is Physiotherapy?
- Physiotherapy is used to help people affected by injury, illness, or disability through movement, exercise, manual therapy, education, and advice.
- At Triangle Physiotherapy, we work in partnership with our patients to help them recover and stay well.
- We use advanced techniques along with evidence-based care. The utilization of these skills allows our physiotherapists to assess, diagnose, treat, and prevent a wide range of health conditions and movement disorders.
What are the benefits of physiotherapy treatment?

- Injury Rehabilitation: Physiotherapists play a crucial role in rehabilitating injuries, such as sprains, strains, fractures, and surgeries. Physiotherapists develop personalized treatment plans to help patients regain strength, flexibility, and mobility.
- Pain Management: Physiotherapy techniques, including manual therapy, massage, and therapeutic exercises, can help reduce pain and discomfort associated with musculoskeletal issues, neurological conditions, and chronic pain.
- Neurological Conditions: Physiotherapy is used to improve motor function, balance, and coordination in individuals with neurological conditions such as stroke, Parkinson’s disease, multiple sclerosis, and spinal cord injuries.
- Cardiopulmonary Rehabilitation: Physiotherapy is involved in rehabilitating individuals with heart and lung conditions, helping them regain cardiovascular fitness and respiratory function.
- Posture and Ergonomics: Physiotherapists can provide guidance on maintaining proper posture and ergonomics to prevent musculoskeletal problems and discomfort.
- Sports Injuries: Physiotherapy is commonly used in sports medicine to treat and prevent sports-related injuries, enhance athletic performance, and aid in sports-specific training.
- Geriatric Care: Physiotherapy can help older adults maintain their independence, improve mobility, and manage age-related conditions like arthritis and osteoporosis.
- Pediatric Conditions: Physiotherapists work with children to address developmental delays, congenital conditions, and other pediatric issues that affect mobility and physical function.
- Preventive Care: Physiotherapists can provide education and exercises to prevent injuries and improve overall physical health and fitness.
- Pelvic Health: Pelvic Floor Physiotherapy refers to a specific and advanced field within physiotherapy that deals with Pelvic Floor Dysfunction. Pelvic Floor Dysfunction can impact people of any age or gender and the term describes several conditions that may affect the urinary, reproductive, digestive, sexual, and/or stability systems in the pelvis. Pelvic Health Physiotherapists have post-graduate training in pelvic health and can resolve many pelvic floor issues in people of all genders and ages.
- Cancer Rehabilitation: Cancer rehabilitation can help you to lessen and overcome these side effects and help you to participate in all your meaningful daily activities. The goal of cancer rehabilitation is to thus improve your daily function and physical and mental well-being both during and after your cancer treatments. Triangle Physiotherapy has trained physiotherapists that provide cancer rehabilitation services to help manage the common side effects of cancer and cancer treatment.
How do I get the most out of my Physiotherapy Appointment?
Getting the most out of your physiotherapy appointment involves effective communication, preparation, and active participation. Here are some tips to help you make the most of your physiotherapy session:
- Be Prepared:
- Write down your symptoms, concerns, and questions beforehand.
- Note any changes in your condition since your last appointment.
- Bring relevant medical reports, imaging results, or a list of medications you’re taking.
- Arrive Early:
- Arriving a few minutes early will give you time to complete any necessary paperwork and relax before your session.
- Effective Communication:
- Clearly describe your symptoms, their onset, severity, and any factors that worsen or alleviate them.
- Be honest about your lifestyle, activities, and habits that could impact your condition.
- Ask questions if you don’t understand something. Your physiotherapist is there to help you.
- Set Clear Goals:
- Discuss your goals with your physiotherapist. What do you want to achieve through physiotherapy? This could be pain relief, improved mobility, or functional goals.
- Follow Instructions:
- Listen carefully to the advice and instructions provided by your physiotherapist.
- Follow the recommended exercises, stretches, or home-care routines diligently.
- Ask Questions:
- Don’t hesitate to ask questions about your condition, treatment plan, exercises, or any concerns you might have.
- Understand Your Treatment Plan:
- Make sure you understand your treatment plan, including the goals, expected outcomes, and duration of treatment.
- Attend your Appointments Consistently: Your treatment plan may prescribe multiple sessions over weeks or months to achieve your health and recovery goals. Attend the sessions recommended by your physiotherapist in your treatment plan to ensure you can achieve the results you are looking for. Sometimes you may feel you are 100% better once your pain is gone but the underlying issue may not be completely resolved and you may risk a recurrence.
- Take Notes:
- Jot down key points, exercises, or recommendations during the session so you can refer back to them later.
- Feedback:
- Provide feedback to your physiotherapist about your progress and any changes you’ve noticed.
- Be Patient:
- Understand that progress may take time. Don’t get discouraged if you don’t see immediate results.
- Hygiene and Attire:
- Wear comfortable clothing that allows easy access to the area being treated.
- Maintain good hygiene, especially if your session involves physical contact.
- Engage Actively:
- Participate actively during the session. Follow your physiotherapist’s instructions and give your best effort during exercises.
Remember, your physiotherapist is there to help you achieve your goals and improve your health and well-being. By being proactive, engaged, and open in your communication, you can maximize the benefits of your physiotherapy appointments.
Which is the closest Physiotherapy clinic near me in Etobicoke?
Our physiotherapy center in Etobicoke is located at 1 The East Mall Crescent near Cloverdale Mall. The closest intersection is Dundas St. W & The East Mall Crescent.
What makes you different from all the other clinics that also provide physiotherapy services near me?
We have been trusted by the residents of the Greater Toronto Area with their physiotherapy needs for over 15 years and we have now become one of the best Physiotherapy clinics in the GTA with numerous reviews to prove it.
Our physiotherapists at our Etobicoke location are all registered physiotherapists and are dedicated in providing the best Physiotherapy service possible.
Why do I need to be treated by a registered physiotherapist?
It is of utmost importance to ensure that you are being seen by a registered Physiotherapist because behind every registered Physiotherapist yes years of academic and clinical training as well as extensive knowledge of all the systems of the human body. At our physiotherapy center, we guarantee that every single physiotherapist we have is registered and will take excellent care of you.
Is there a highly qualified physiotherapist at your physio clinic in Mississauga who you would recommend I see?
Our physiotherapy center in Mississauga has highly qualified professional physiotherapists with many years of experience. We have physiotherapists with FCAMPT designation, which is the highest certification in manual therapy.
We also have a team of highly skilled professionals including physiotherapists, massage therapists, acupuncturists, chiropractic doctors as well as naturopathic doctors. You are welcome to read their profiles on our website or call us for more information.
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Physiotherapy is an effective treatment for a wide range of conditions, helping individuals recover and improve their quality of life. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists are committed to helping you achieve your health goals through personalized and evidence-based treatments.”
Warm-up exercises are essential to prepare your body for more intense physical activity by increasing blood flow to your muscles, raising your heart rate, and improving flexibility.
Here are ten effective warm-up exercises you can perform before a workout:
- Jumping Jacks: Stand with your feet together and hands by your sides. Jump and spread your feet apart while raising your arms overhead. Jump again to return to the starting position.
- High Knees: Stand with feet hip-width apart. Lift one knee at a time towards your chest while jogging on the spot, pumping your arms as you go.
- Arm Circles: Extend your arms out to the sides and make small circles with your hands, gradually increasing the size of the circles. After a few repetitions, reverse the direction.
- Leg Swings: Hold onto a stable surface (e.g., a wall or pole) for balance. Swing one leg forward and backward, and then sideways, in a controlled manner. Repeat with the other leg.
- Hip Circles: Stand with your feet hip-width apart and place your hands on your hips. Make circles with your hips, rotating in both clockwise and counterclockwise directions.
- Bodyweight Squats: Stand with feet shoulder-width apart. Lower your body into a squat position by bending your knees and pushing your hips back. Return to the starting position and repeat.
- Arm Crosses: Extend your arms straight out to the sides at shoulder height. Cross your arms in front of your chest, then open them wide again. Continue crossing back and forth.
- Butt Kicks: Stand with feet hip-width apart. Kick your heels up towards your glutes, one leg at a time, while jogging on the spot.
- Shoulder Circles: Stand with feet shoulder-width apart. Raise your shoulders up towards your ears, then roll them backward in a circular motion. Reverse the direction after a few repetitions.
- Walking Lunges: Take a step forward with one leg and lower your body into a lunge position. Push off the front foot and bring it back to the starting position. Repeat with the other leg.
FAQs
1. How long should I spend on warm-up exercises?
Aim to spend at least 5 to 10 minutes on your warm-up routine. The duration may vary depending on the intensity of your workout and personal preferences.
2. Should I stretch during the warm-up?
Dynamic stretching, which involves moving your muscles through their range of motion, is more appropriate during the warm-up. Save static stretching (holding stretches for extended periods) for after your workout.
3. Can I skip the warm-up if I’m short on time?
It’s not advisable to skip the warm-up entirely, as it increases the risk of injury and reduces your performance during the workout. If you’re short on time, shorten the warm-up but ensure you still get your heart rate up and do some dynamic movements.
4. Can I warm up without any equipment?
Absolutely! The warm-up exercises listed above require no equipment. They use your body weight and basic movements to prepare your muscles and cardiovascular system for exercise.
5. How intense should the warm-up be?
The warm-up should be less intense than the main workout. Gradually increase the intensity of the warm-up exercises to elevate your heart rate and prepare your body for the upcoming challenges.
Remember that warm-up exercises should be tailored to your specific workout routine and individual needs. A qualified physiotherapist can assess you and determine if you have any pre-existing conditions and recommend the best pre-workout routine for you.
How do I book an appointment at a Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Performing proper warm-up exercises before a workout is essential for preventing injuries and maximizing performance. Triangle Physiotherapy offers expert guidance and care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you develop a personalized warm-up routine to ensure a safe and effective workout.”









