Spondylolisthesis is a condition that leads to back pain caused by the instability in the vertebrae. According to an article published in Spine, 6 to 11.5% of the adult population experiences this condition. People who are involved in football or gymnastics are at a higher risk. While we understand that it’s a painful condition to be in, we don’t want you to stop doing what you love and therefore, we suggest you to book an appointment with our expert Physiotherapists at any of our nine rehabilitation clinics across the GTA ( Physiotherapy Etobicoke, Physiotherapy North York, Physiotherapy Mississauga, Physiotherapy King West, Physiotherapy Lawrence Park, Physiotherapy Erin Mills, Physiotherapy Queen Quay, Physiotherapy Oakville, Liberty Village).
When it comes to spondylolisthesis, exercise plays a very important role in improving the condition. However, one must remember here that not all exercises are safe and can even further damage the spine. We are going to make you learn Spondylolisthesis exercises that must be avoided for an effective Spondylolisthesis treatment. Before we move to exercises to avoid in spondylolisthesis, we must first understand what is spondylolisthesis.
Spondylolisthesis – an overview

Is is usually caused by degeneration of the vertebrae or disc, due to trauma, injury or genetics. It makes a piece of the spinal bone, also known as vertebrae slips out of alignment and onto the bone below it. Spondylolisthesis usually occurs at the fifth lumbar vertebrae. As reported by the Cleveland Clinic, spondylolisthesis is one of the most common causes of back pain for teen athletes. Having said that, degenerative spondylolisthesis also results in low back pain in people older than 40 years.
Specific spondylolisthesis exercises are suggested to alleviate the pain and discomfort thereby improving the function and quality of life. Let’s now talk about the symptoms of spondylolisthesis.
Symptoms of Spondylolisthesis
Most of the spondylolisthesis symptoms include pain in the lower back that gets worse with standing and hyperextension. The pain may appear like a muscle strain. There are some other symptoms of spondylolisthesis that one must look out for –
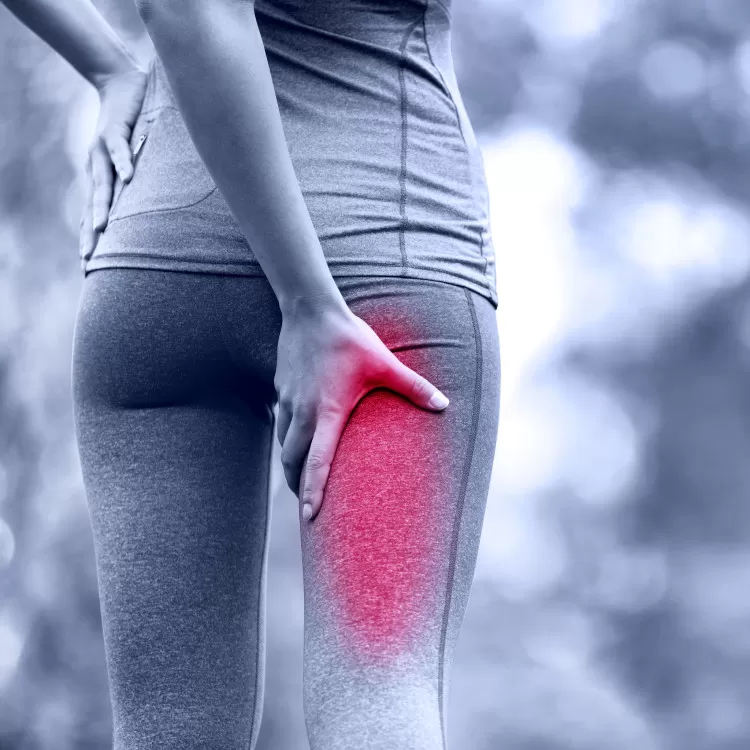
• Tightness in hamstring
• Pain in posterior buttock
• Neurological changes including tingling down the legs and numbness
If you are experiencing any of these symptoms or have recently occurred an injury, consult our experienced physiotherapists at our rehabilitation clinics in different locations in GTA.
After a through examination, the physiotherapist suggests a personalised program to help reducing the pain and discomfort caused due to spondylolisthesis. Usually, the physiotherapists classify spondylolisthesis as low grade or high grade, depending on how much the vertebrae have slipped forward. Patients with lesser symptoms and low-grade slips respond well to conservative line of treatment, like exercise. However, patients who experience high grade slips witnessing numbness or tingling in the legs may require surgery.
Considering the potential risks, it is very important to know what exercises must be avoided in spondylolisthesis to prevent further damage or injury.
Spondylolisthesis Exercises to Avoid
If you are looking to rehabilitate a non-operative spondylolisthesis after consulting with the physiotherapist, expect it to take three to six months to heal, according to Sanford Orthopaedics Sports Medicine. It is suggested that the patient must take a break of at least three months from sports and athletics. The patients are also suggested to wear a brace for continuous stretch of time.
Other than rest and bracing, there are many other things to avoid in spondylolisthesis. We are now listing spondylolisthesis exercises to avoid to ensure proper and speedy recovery. These include lumbar extension movements that can take your spine past the neutral position. The lumbar extension movements may increase the pain and slow down the healing of the affected vertebrae.
Some other exercises to avoid in spondylolisthesis include –
- Prone press-ups (Push-up while lying on the stomach)
- Standing extensions
- Prone leg raises (Lifting legs while lying on the stomach)
- Back extension machine at the gym
It is also suggested that yoga asanas must also be avoided in spondylolisthesis. Yoga includes various back extension postures, like cobra and swan pose, which may not be safe to practice in spondylolisthesis.
There are some other exercises that must be avoided in spondylolisthesis. These includes weightlifting, exercises that need you to twist or bend, high impact activities that put a lot of stress on the healing back, like jumping rope or box jumps.
Now that we have learnt what exercises should be avoided for spondylolisthesis, we must also understand are the best to treat spondylolisthesis. Just like all the other injuries, physiotherapy is beneficial in the treatment of spondylolisthesis. Mostly, the rehabilitation focuses on increasing the core muscles without going past neutral along with hamstring stretches. One should expect up three to six months of rehabilitation before returning back to normalcy.
Spondylolisthesis Exercises to Do
We suggest the following spondylolisthesis exercises for a speedy and efficient recovery. We also suggest you to consult with your physiotherapist and not undertake any of these exercises without his approval.
- Pelvic tilt exercises – These exercises help in reducing the discomfort by stabilising the lower spine in a flexed position. Depending upon the pain and your preference, pelvic tilt exercises can be done in various positions.
- Crunches – Patients suffering from spondylolisthesis often face instability and pain caused by weak abdominal muscles. This can be strengthened with powerful crunch exercises. You must try to focus on proper form and moving slowly to engage the core muscles. Spondylolisthesis is a painful condition to be in and therefore we suggest not to force the body to move through full range of motion. This may increase the pain and slow down the recovery time.
- Hamstring stretch – Spinal instability often causes tension in the hamstrings to those suffering from spondylolisthesis. Hamstrings are the large muscles that run down the back of the thigh. Stretching hamstrings sitting on the ground can help to relieve tension and tightness caused due to spondylolisthesis. It also reduces the lower back pain.
- Multifidus activation – Multifidus muscles are the small but very important muscles lying next to the spine. These muscles help in bending and twisting movements thereby increasing the stability of the spinal joints. If suffering from spondylolisthesis, activating multifidi will ease the pain and provide the much-needed comfort.
- Double knee to chest – This spondylolisthesis exercise is suggested to decrease the instability and improve the strength. It works on the core muscles of the torso and is thus beneficial in spondylolisthesis.
Check with your physiotherapist before starting any exercise program for spondylolisthesis while recovering from this injury. You can aim for a gradual return to physical and sports activities, depending on the severity of the injury and how string your core is. Post healing core strengthening is also suggested to prevent future injuries.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
For those managing spondylolisthesis, seeking guidance from professional physiotherapists is essential. Whether you are looking for physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are specialized clinics available to help you avoid harmful exercises and support your recovery with personalized treatment plans.
Why Physiotherapy?

Physiotherapy is a highly beneficial niche treatment of injury, disorder and disease. Using specific physical methods, it aids in restoring the mobility, function and movement in the affected area. Physiotherapy uses experimented and researched information on how the body works and uses medically certified procedures for treatment.
Physiotherapy also comes extremely advantageous in preventing further injury or damage on the previously strained body part. It is widely popular as people of any age can receive its benefits by managing and maintaining great shape and health, thereby preventing injury or disease.
Physiotherapy is a degree-based occupation where well-trained, skilled and experienced professionals provide the best care and treatment. At Triangle Physiotherapy, our team of exceptionally qualified Physiotherapists do their best to provide you finest and world-class service.
Physiotherapists at Physiotherapy Oakville are well-researched and use their extensive skills and experience to improve complicated conditions like respiratory, neurological, cardiovascular, and neuromusculoskeletal issues. If you have an injury or are facing a problem, consult our expert physiotherapists at Physiotherapy Oakville at its various locations.
Our team stays updated with the latest scientific advancements, ensuring that you receive the most effective treatments available. By joining Physiotherapy Oakville, you benefit from personalized care plans tailored to your unique needs, helping you achieve optimal recovery and improved quality of life. Don’t wait connect with our experts today and take the first step towards better health and well-being.
Benefits of Physiotherapy
We are listing below some conditions where physiotherapy has helped in providing the best possible results.
- Eliminating or reducing pain
Patients suffering from arthritis, muscle strain/sprain or tendonitis benefit from using therapeutic techniques and exercises such as Soft Tissue Mobilization or usage of modalities like TENS, IFC and Ultrasound. These therapies help in alleviating the pain thereby ensuring normalcy. You can check with our specialized and trained physiotherapists at Etobicoke centre for more information on this.
- Helps in avoiding surgery
Let’s face this. We are all living in tough pandemic times and nobody wants to visit a hospital or undergo a surgery. However, there are some unavoidable situations where surgery is the last resort. Physiotherapy can help in avoiding this by managing and healing in the initial stages itself. It is also helpful in pre and post rehabilitation programs to mitigate the complications that can occur in the surgery. If you are residing in or around Toronto, we suggest you to consult our Physiotherapy experts in Toronto before planning a surgery. You can also discuss your case if you are recuperating from a surgery or treatment.
- Improving overall strength and coordination
While physiotherapy is highly beneficial to reduce the pain during or after a surgery, it also aids in improving the overall strength and robustness of the body. Do you know that physiotherapy involves specific exercises and stretches that help in cumulative coordination of the body? So, if you are facing symptoms of vertigo or dizziness, we suggest you to get in touch with our Physiotherapists. Our expert physiotherapists in Oakville are highly qualified and provide specific program for your requirement.
- Reducing the dependency on medicines
Every medicine that a patient consumes has a side effect at some point in life. Certain situations demand a patient to take medicines to control or treat his/her condition. However, there are cases like surgery, where a patient is dependent on the medicine for pain relief. We suggest physiotherapy as an alternative choice to address this concern and reduce the dependency and side effects caused by medicines.
- Boosting cardiovascular functioning and lung capacity
Post- stroke surgery requires extreme care and recovery program. Physiotherapy offers post heart stroke patients in regaining their degree and sense of direction, movement and balance. Our experience physiotherapists at Triangle Physiotherapy helps the patients in readjusting to their daily healthy lifestyle. You can consult our seasoned and best physiotherapists at Lawrence Park for special programs on breathing exercises that helps in restoring the optimal lung capacity and blood flow in the body.
- Managing and preventing sports related injuries
We understand that sports is all about agility and various sports can elevate the risk to specific types of conditions like ACL Tear, Golfers Elbow, Hamstring strain to name a few. Physiotherapy is extremely important and useful in such situations as it provides very specific treatment to improve the endurance and fix the symptomatic problem. Other than the injuries, sportsperson and athletes are benefitted with regular physiotherapy sessions. Our team of skilled physiotherapists at North York helps in improving the circulation and strengthening body muscles. This increases the flexibility which will improve whichever game you play.
- Staying fit at all ages and phases
Old age is not always pleasant. It brings with it certain complications that hamper the daily lifestyle. These includes Rheumatoid Arthritis (RA), Osteoporosis, Sciatica, Dementia, Neck pain, Back pain, Knee replacement etc. All these ailments can be controlled and managed by physiotherapy. If you or any of your loved ones is facing old age problems like these, we suggest you to check our rehabilitation clinic across GTA. You can have a look at Triangle Physiotherapy Mississauga or any other clinic close to your location.
- Managing heart and diabetic conditions
It has been often observed that the diabetes patient suffer from discomforts like knee, shoulder and back pain. This is often resulted because of the unbalanced sugar levels in the body. There are dedicated physiotherapy plans that help in pain management caused due to diabetes. These plans also aid in controlling the sugar levels. Our expert physiotherapists at Triangle Physiotherapy help in guiding the patients about Diabetic Neuropathy, Diabetic Foot etc.
- Easing pregnancy and postpartum care
Pregnancy is a beautiful journey. However, many women face trouble in this journey as their bodies undergo fundamental changes impacting overall well being and health. Many women face issues like fluctuating hormones, difficulty in carrying out routine activities due to increased body weight, changing habits etc. We suggest checking with our brilliant physiotherapist in Queens Quay clinic to enjoy this wonderful experience
- Improving mental health
Of all the amazing benefits of physiotherapy, mental health is the most important one. We are not saying this just in terms of ‘feeling happy and healthy’. We understand that Mental Health is a lot more than that. At Triangle Physiotherapy, we acknowledge and advocate the fact that feeling good in your body is important not just to do your daily chores, but also to elevate your confidence in whatever do and wherever you go. That’s why we are – to help you realize your true and full potential.
With the help of a skilled and qualified physiotherapist from Triangle Physiotherapy, we can customize a program for you that will suit your specific need. Get in touch with us and we would be happy to answer all your queries.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
Physiotherapy offers numerous benefits, from pain relief and improved mobility to faster recovery from injuries. If you’re looking for quality physiotherapy services, there are excellent options in various locations, including physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide personalized care to help you achieve better health and well-being through effective physiotherapy treatments.
Physiotherapy is the study of science of movements. It is a healthcare profession that includes different treatment modalities like massages, electrotherapy, heat therapy, exercises, patient awareness and advice for treating an ailment, deformity or injury.
When should I go to a Physiotherapist?
This is a very common yet important question. If you have suffered an injury or chronic pain that affects your daily chores, then you must consult a good physiotherapist. You can also avail the benefits of physiotherapy after surgery, like knee replacement or stroke.
At Physiotherapy Oakville, we have a team of dedicated and skilled physiotherapists who provide expert care tailored to your specific needs. Scientific research supports the role of physiotherapy in improving recovery outcomes and enhancing overall physical function post-surgery. By joining Physiotherapy Oakville, you gain access to personalized treatment plans and evidence-based practices that help you recover efficiently and resume your daily activities with confidence.
What will a Physiotherapist do?
Our experienced Physiotherapists provide case-based solution to your need. These are focused on preventive as well as rehabilitation. Some scenarios where a good Physiotherapist can help –
- Back and neck pain caused due to sprain in the skeleton or muscles
- Conditions like arthritis or after effects of amputation that results in discomfort in joints, muscles, knees and ligaments
- Lung disorders like asthma or bronchitis
- Disability resulting from heart problems
- Troubles occurred during childbirth like pelvic issue, bladder and bowel problems
- Parkinson’s disease and multiple sclerosis or loss of mobility due to trauma to the brain or spine
- Pain, swelling, fatigue, loss of muscle strength and stiffness during palliative care or cancer treatment
What should I expect from my Physiotherapist?
Our trained Physiotherapists at Triangle Physiotherapy provide specific and concerned answers to your core problems. This is what you can expect from your Physiotherapist-
- Your physiotherapist will understand your medical history
- Based on the medical history and symptoms, the physiotherapist will assess and diagnose your condition
- A treatment module will be set for you for your concern
- Specific exercises and assistive devices would be suggested to you based on your module
To understand what all things are done in Physiotherapy, let’s try to learn the various types of treatment modalities used in Physiotherapy.
- Manual Therapy – This technique is a very common one where the physiotherapists massage the affected joints to mobilise and manipulate using his hands. Our team of expert physiotherapists in Toronto are highly equipped and experienced in this therapy.

- Transcutaneous Electric Nerves Stimulation (TENS) Therapy – In this therapy, the physiotherapist uses a small device driven by a battery and place it on the skin surface of the patient. Low grade currents are sent through these electrodes to relive pain of the affected area.
- Magnetic Therapy – This therapy uses electromagnets of different sizes and types. These are used to limit the pain of the affected body part.
- Dry needling and acupuncture – In this therapy, the physiotherapist uses fine needles and insert them into specific body parts to alleviate the pain for a short time. You can consult with our physiotherapists at Etobicoke clinic for this specialized line of treatment.

- Taping – This physiotherapy technique is highly popular as it promotes body’s inherent natural healing mechanism. Here, the physiotherapist uses a tape which lifts the skin away from the connecting tissue, thereby increasing the space and allowing the lymphatic fluid to move more functionally to ease the pain.

- Joint Mobilisation – This is a manual therapy technique where a physiotherapist mobilises the joint at different depths, speeds and amplitudes. It helps in restoring normal joint movement in the body. Our physiotherapists at Lawrence Park clinic are highly equipped and skilled in this technique.

- Stretches and exercises – This is a fairly common module where the physiotherapist teaches different exercises and techniques for body stretching which helps in restoring the joint movements.
- Rehabilitation – This includes a broad range of corrective, preventive and stretching exercises to reduce the sprain or pain in the affected area.
- Strengthening Program – This is one of the most important modalities in physiotherapy where the physiotherapist conducts specific program to make the patient understand about his personal responsibility towards his health and physical conditioning. This program is very useful as it helps the patient in improving overall heath, strength, balance, coordination and flexibility.

- Diathermy – In this technique, electrically induced heat or high-frequency electromagnetic currents are used to relive the pain and cure the condition. Our physiotherapists at North York clinic are efficient and skilled in this technique. If you are facing pain or recovering from a surgery, you can consult us.
- Ultrasound and phonophoresis – A frequency range of 0.5 – 3 MHz is used in this therapeutic ultrasound. This technique induces a deep heat to the target area to treat muscle spasm, promote healing at cellular level and lower the inflammation. It also increases the metabolism and improve the flow of blood towards the damaged tissue. Phonophoresis uses ultrasonic waves for better absorption of drugs that are applied topically during the treatment. This is a very useful technique as it helps in reducing the pain by allowing maximum absorption of drugs like anti-inflammatory and analgesics.
- Range of Motion exercises (RoM) exercises – A good physiotherapist would diagnose the patient and recommend Range of Motion exercises to improve the mobility of joints and reduce the stiffness in the muscles. There are various types of RoM exercises, like Passive Range of Motion (PROM) exercises, Active Assistive Range of Motion (AAROM) exercises and Active Range of Motion (AROM) exercises.
- Soft tissue mobilization – This highly effective technique in physiotherapy helps in alleviating pain, reducing swelling and relaxing the tight muscles in the body.
To summarize, Physiotherapy is a special treatment to maintain, restore and make the most of a person’s function, mobility, strength and well-being. It helps through various techniques and aid in recovery as well as strengthen the body for w holistic living.
Now that we have established what all is done and expected in Physiotherapy, we would like to hear from you. Please write to us if you have any questions regarding Physiotherapy. You can also check our services and locations for any line of treatment.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy encompasses a wide range of techniques, including manual therapy, exercise prescription, and patient education, to promote healing and recovery. For those seeking physiotherapy services, there are numerous clinics available in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and customized treatment plans to help patients achieve optimal health and mobility.
Imagine you have the power to control your pain, and stiffness.You will not have to spend months in therapy. You will not need to buy or use expensive equipment. You will not have to rely on needles, injections or surgery.You will use your own skills and resources when you gain knowledge and guidance from a Certified McKenzie Provider.
What is the McKenzie method?

The Mckenzie method utilizes repeated movements for assessment , diagnosis and treatment. It is a comprehensive and clinically reasoned evaluation of patients where the emphasis is on patient independence , avoidance of therapist dependency, and use of minimal intervention.
Also read, Best Physiotherapy Clinic in Etobicoke
What lower back problems can we treat with Mckenzie?
Developed by world-renowned expert physiotherapist Robin McKenzie in the 1950s, this well-researched MDT is a reliable assessment process intended for all musculoskeletal problems, including pain in the back, as well as issues associated with sciatica, sacroiliac joint pain, arthritis, degenerative disc disease, muscle spasms and intermittent numbness in feet. If you are suffering from any such issues, then a MDT assessment may be right for you!
How does it work?
Most musculoskeletal pain is “mechanical” in origin, which means it is not due to a serious pathology like cancer or infection but a result of abnormal forces or mechanics occurring in the tissue. Further, it means that a position, movement or activity caused the pain to start. If a mechanical force caused the problem then it is logical that a mechanical force may be part of the solution. The MDT system is designed to identify the mechanical problem and develop a plan to improve it. In the simplest and most common instance, this may mean that moving in one direction may provoke and worsen the pain, and moving in the opposite direction may eliminate the pain and restore function.
Also Read, Best Clinic for Physiotherapy in Oakville
Assessment, treatment and prevention.
The McKenzie assessment process begins with the trained clinician taking a detailed history about your symptoms and how they behave. This enables the clinician to identify specific pain patterns, which then helps the clinician develop a treatment plan specific to your pattern of presentation. The clinician will prescribe specific exercises and advice regarding appropriate postures and ergonomics.If your problem has a more difficult mechanical presentation, a certified McKenzie clinician can provide advanced hands-on techniques to help manage the problem until you can self-manage.The aim is to be as effective as possible in the least number of treatment sessions. By learning how to self-treat your current problem, you gain hands-on knowledge to minimize the risk of recurrence and rapidly deal with symptoms if they recur putting you in control safely and effectively. The chances of problems persisting can more likely be prevented through self-maintenance.
Take control of your pain, empower yourself and get back to the life you love with the McKenzie Method of Mechanical Diagnosis and Therapy.
Book an appointment with our McKenzie Certified Physiotherapist, Ankit Doshi, BPT, MClSc (Adv Healthcare Practice), FCAMPT, CGIMS, Cert. MDT
Related Tags : Physiotherapy Toronto, physiotherapy Oakville, physiotherapist Toronto, physiotherapist North york, physiotherapists Toronto, physiotherapists Oakville, physiotherapy exercise Toronto, physiotherapy exercise Oakville
The McKenzie Method is a proven approach for managing low back pain through specific exercises and posture correction. If you are seeking professional physiotherapy to help with back pain, there are excellent clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide personalized care and expert guidance to help you manage pain and improve your quality of life.
Piriformis Syndrome is a neuromuscular disorder that is caused when the piriformis muscle compresses the sciatic nerve. The piriformis muscle is a flat, band-like muscle located in the buttocks near the top of the hip joint. This muscle is important in lower body movement because it stabilizes the hip joint and lifts and rotates the thigh away from the body. This enables us to walk, shift our weight from one foot to another, and maintain balance. It is also used in sports that involve lifting and rotating the thighs, in short, in almost every motion of the hips and legs.

Causes of Piriformis Syndrome
The exact causes of piriformis syndrome are unknown. Suspected causes include:
- Muscle spasm in the piriformis muscle, either because of irritation in the piriformis muscle itself, or irritation of a nearby structure such as the sacroiliac joint or hip
- Tightening of the muscle, in response to injury or spasm
- Swelling of the piriformis muscle, due to injury or spasm
- Bleeding in the area of the piriformis muscle.
Also read, Best Mississauga Physiotherapy Clinic
Symptoms of Piriformis Syndrome
Most commonly, patients describe acute tenderness in the buttock and sciatica-like pain down the back of the thigh, calf and foot. Typical piriformis syndrome symptoms may include:
- A dull ache in the buttock
- Pain down the back of the thigh, calf and foot (sciatica)
- Pain when walking up stairs or inclines
- Increased pain after prolonged sitting
- Reduced range of motion of the hip joint
- Symptoms of piriformis syndrome often become worse after prolonged sitting, walking or running, and may feel better after lying down on the back.
Also Read, Triangle Physiotherapy Clinic at Oakville
Physiotherapy Treatment for Piriformis Syndrome
Ice Packs and Ice Massage
At the onset of pain, lie in a comfortable position on the stomach and place an ice pack on the painful area for approximately 20 minutes. Repeat as needed every 2 to 4 hours.
It may be more helpful to combine a gentle massage with the ice. Lie on the stomach and have someone gently massage the painful area with a large ice cube. If ice is applied directly to the skin (instead of a cold pack), limit it to 8 to 10 minutes to avoid an ice burn.
Heat Therapy
Some people find it helpful to alternate cold with heat. If using a heating pad, lie on the stomach and place the heating pad on the painful area for up to 20 minutes. Be sure to avoid falling asleep on a heating pad, as this may lead to skin burns.
Electrotherapy
The application of electrical stimulation to the buttock with a transcutaneous electrical nerve stimulation (TENS) unit or interferential current stimulator (IFC) can help to block pain and reduce muscle spasm related to piriformis syndrome.
Also Read, Best Physiotherapists in Etobicoke
Piriformis stretches
There are a number of ways to stretch one’s piriformis muscle. Two simple ways include:
- Lie on the floor with the legs flat. Raise the affected leg and place that foot on the floor outside the opposite knee. Pull the knee of the bent leg directly across the midline of the body using the opposite hand or a towel, if needed, until stretch is felt. Do not force knee beyond stretch or to the floor. Hold stretch for 30 seconds, then slowly return to starting position. Aim to complete a set of three stretches.
2. Lie on the floor with the affected leg crossed over the other leg at the knees and both legs bent. Gently pull the lower knee up towards the shoulder on the same side of the body until stretch is felt. Hold stretch for 30 seconds, then slowly return to starting position. Aim to complete a set of three stretches.
Ref: https://en.wikipedia.org/wiki/Piriformis_muscle
http://www.spine-health.com/conditions/sciatica/symptoms-and-diagnosis-piriformis-syndrome.
Piriformis syndrome can cause significant discomfort and requires targeted physiotherapy to alleviate pain, improve mobility, and prevent further issues. If you are looking for professional physiotherapy services to manage piriformis syndrome, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer specialized care and personalized treatment plans to help you recover and regain full mobility.
Shoulder Prehabilitation (prehab) involves the process of implementing a physical, psychological, nutritional intervention before an individual goes into surgery. The goal behind prehab programs is to maximize an individual’s physical and psychological fitness/health before surgery in order to reduce pain, increase physical function and allow you to return to your normal activities sooner following surgery.
Although there is limited evidence regarding shoulder prehab programs, there is promising and growing evidence that suggests prehab programs for hip, knee, and spinal surgery may improve pain, function and reduce the total cost of healthcare spending in the post-operative period.
Also Read, Physiotherapy Clinics in Etobicoke

Types of Surgeries for Shoulder
- Reverse arthroplasty
- Total shoulder arthroplasty/replacement
- Rotator cuff repair
- SLAP repair
- Bicep tendon repair
- Tenotomy
What Prehab Programs look like:
Most prehab programs can be anywhere from 2-8 weeks leading up to surgery and could potentially involve:
1) Exercise training (2-3x/week)
- Strengthening and stabilization exercises for the rotator cuff and muscles supporting your shoulder blade
- Home exercise program tailored to your needs
- Exercise training 1 on 1 with a physical therapist
2) Education: information delivered regarding
- Shoulder anatomy and mechanics
- Pain science education
- The process of your operative procedure
- Patient-therapist expectations
- Post-operative protocol
- Detailed exercise program and technique
Also read, Best Physiotherapist near Mississauga
3) Nutritional support
- Consultation with a registered dietician
- Detailed nutrition programs to optimize physical and mental health
- Nutritional supplements as indicated
4) Psychological support
- Consultation with psychologist/ psychotherapist
- Anxiety and stress reduction
- Cognitive-behavioral therapy
- Relaxation techniques
- Coping strategies for surgery
Shoulder Prehab is a set of exercises and movements designed to strengthen and condition the shoulder joint and surrounding muscles, helping to prevent injury or improve recovery from a previous injury. Prehabilitation may include:
- Shoulder rotator cuff strengthening exercises such as internal and external rotation with light weights.
- Scapular stability exercises to improve posture and reduce stress on the shoulder joint.
- Stretching to improve flexibility and range of motion.
- Plyometric exercises to improve power and explosiveness.
- Core stability exercises to improve overall body control and stability.
Prehabilitation should be performed regularly, especially if you have a history of shoulder injuries or plan to participate in overhead activities such as weightlifting or throwing. By taking care of your shoulder before it becomes a problem, you can help prevent injury and improve your performance.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Shoulder prehabilitation is essential for preventing injuries and optimizing recovery, especially for those undergoing surgery or managing shoulder pain. If you’re looking for professional physiotherapy services for shoulder prehabilitation, there are several clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care to help you strengthen your shoulders and maintain overall joint health.
One of the most common runners’ complaints is Shin splints (also known as Medial Tibial Stress Syndrome (MTSS)). The word shin splints describes pain/discomfort that gets worse during running or exercise around the front of the lower shin. Shin splints are usually developed by overuse, and a registered physiotherapist will do a detailed assessment to diagnose shin splints and develop a treatment plan to resolve them.
Shin splints are painful and uncomfortable but here are a few tips to effectively manage them.

Woman suffering from an ankle injury while exercising. Running sport injury concept.
Rest
Shin splints are considered an overuse injury. In the short term, rest will help the pain, and it is advised to rest for a period of time before beginning to run again. Start with shorter, slower distances instead of jumping right back into long distances when you start running again. Start running once a week and work up to twice a week if you usually run 3 days a week.
Also read, Best physsiotherapy clinic in Oakville
Ice
Place ice packs on your shins for a few minutes at a time. Icing will not treat your shin splints but will help effectively manage your pain after running.
Change up your workout routine
Adding resistance training to your workout routine can help reduce your pain by helping your muscles & tendons increase their capacity. Incorporating other types of aerobic exercise into your routine, like cycling, rowing, or the elliptical in place of running, can also help. Shin splints commonly come from the impact from running on hard or uneven surfaces. Replacing running with a different type of exercise once a week can help.
Stretching, warm-ups and cool-downs
Stretch your calves and shins before running to increase the flexibility in your legs. Warm-up before your workout to prepare your muscles and cool down at the end of it to help your muscles recover.
Also read, Best Physiotherapy Clinic in Missisuaga
Footwear & Orthotics
Think about how long you have had your running shoes. Good shoes are important as they act as shock absorbers every time your foot hits the ground. If the sole of the shoe is worn, shoes lose their shock absorption. Try a new pair of shoes with more cushioning and see how you get on.
Also, consider seeing a chiropodist for a pair of orthotics. Custom orthotics can help align and stabilize your foot and ankle, taking stress off of your lower leg. They can also be beneficial if you have flat feet.
Our physiotherapists at Triangle Physiotherapy can help resolve your shin splints and get you back to running or any other sport that you may love! Call us to book your assessment or book online here.
If you’re suffering from shin splints, professional physiotherapy can help with pain management and recovery through targeted exercises and treatments. For those in need of physiotherapy services, there are reputable clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care to help you recover from shin splints and get back to your daily activities pain-free.
Osteoarthritis (OA) is caused by the wear and tear of the cartilage and can affect all joints in the body. The most commonly affected areas are the knees, hips, low back, neck, and the digits of the hands and feet. Osteoarthritis affects 3.3%-3.6% of the population globally. The risk factors for osteoarthritis include age, gender, weight, anatomy, and history of trauma. The severity of osteoarthritis can be evaluated through medical imaging.
The following are characteristics and clinical presentation of OA:
- Use-related pain
- Stiffness
- Crepitus
- Decrease range of motion and flexibility
- Instability, Weakness
- Deformity
- Swelling
- Local

Also read, Best Physiotherapy Clinic in Mississuaga
OA can be managed conservatively through physiotherapy or chiropractic interventions. Pharmacological or surgical intervention may also be of benefit depending on the severity of the joint. Assistive devices can aid in offloading the damaged joint. Physiotherapy and chiropractic treatment for osteoarthritis focuses on reducing pain and increasing physical function through education and exercises. An individualized exercise program consisting of stretching and strengthening the muscles surrounding the affected joint will improve the well-being of the individual.
Tell me more about the GLA:D™ for knee and hip osteoarthritis.
- Good Life with osteoArthritis in Denmark (GLA:D™), developed in Denmark, is an education and tailored neuromuscular exercise program designed for individuals with hip or knee osteoarthritis
- The program is unique because it provides education and targeted exercise that can be applied to movement in everyday activities
- The program is suitable for individuals with early to late stages of OA
The following are the benefits of an individualized exercise program:
- Decrease pain and stiffness
- Increase mobility and function
- Improve muscles length and elasticity
- Improve cartilage
- Reduce risk of injury
- Delay surgical intervention
A physiotherapist and chiropractor can help identify the main issues affecting an osteoarthritic joint and create a treatment program based on your needs and goals.
Contact us today if you would like to see one of our physiotherapists or chiropractors to help you manage your osteoarthritis & relieve your pain.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Managing osteoarthritis effectively requires a comprehensive treatment approach, including physiotherapy to alleviate pain and improve mobility. If you’re looking for professional physiotherapy services to support your osteoarthritis management, clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village offer expert care and personalized treatment plans to help you achieve better joint health and quality of life.
Knee ligament injuries are quite common, and they can occur at any age. These injuries can be caused by a variety of factors, such as sports injuries, accidents, or falls. Knee ligaments connect the bones in the knee, and when they are injured, they can cause severe pain, swelling, and instability in the joint.
Anatomy of the Knee
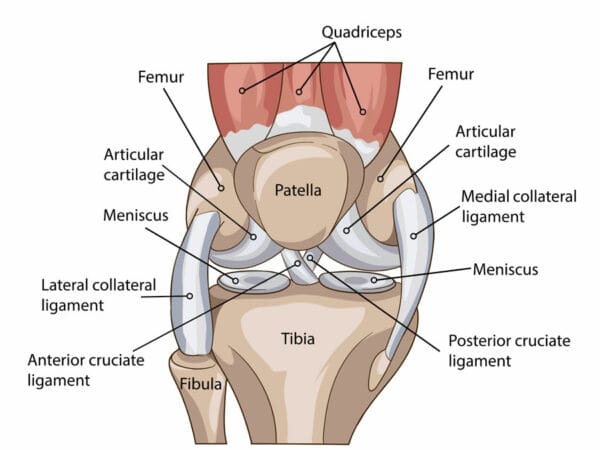
There are four primary ligaments in the knee, and they are the anterior cruciate ligament (ACL), the posterior cruciate ligament (PCL), the medial collateral ligament (MCL), and the lateral collateral ligament (LCL). Each of these ligaments serves a vital function in the knee joint, and an injury to any one of them can cause significant problems.ACL injuries are common in sports that require sudden stops and starts, such as football, basketball, and soccer. A sudden change in direction or a twisting motion can cause the ACL to tear or sprain. Symptoms of an ACL injury include a popping sound in the knee, severe pain, swelling, and difficulty walking or standing.
PCL injuries are less common than ACL injuries but can occur in the same types of sports. The PCL is located at the back of the knee and is responsible for stabilizing the knee joint. Symptoms of a PCL injury include pain, swelling, and instability in the knee joint.
MCL injuries are often caused by a direct impact to the outer side of the knee, such as during a tackle in football. Symptoms of an MCL injury include pain, swelling, and difficulty straightening the knee.LCL injuries are less common than MCL injuries but can occur in the same types of sports. The LCL is located on the outer side of the knee and is responsible for stabilizing the joint. Symptoms of an LCL injury include pain, swelling, and instability in the knee.
What is the best treatment for Knee ligament injuries?
Treatment for knee ligament injuries varies depending on the severity of the injury. In mild cases, rest, ice, compression, and elevation (RICE) may be all that is necessary to relieve pain and swelling. In more severe cases, surgery may be required to repair the damaged ligament.
Physical therapy is an essential component of treatment for knee ligament injuries. A physical therapist can help the patient regain strength, mobility, and flexibility in the knee joint. Exercises that focus on strengthening the muscles around the knee can help reduce the risk of future injuries.
How do I prevent knee injuries from recurring?
Preventing knee ligament injuries is also essential, especially for athletes who participate in high-impact sports. Wearing appropriate protective gear, such as knee pads, can help reduce the risk of injury. Stretching before and after exercise can also help prevent injuries.
In conclusion, knee ligament injuries can be a significant source of pain and disability. It is essential to seek prompt medical attention if you suspect you have a knee ligament injury. With the right treatment and rehabilitation, most people can recover from these injuries and return to their normal activities. Preventing knee ligament injuries is also crucial, and taking appropriate precautions can help reduce the risk of injury.
Book an appointment to see one of our physiotherapists to get that knee injury treated.
Recovering from knee ligament injuries requires proper physiotherapy to restore strength, stability, and function. For those seeking professional care, there are numerous physiotherapy clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide expert physiotherapy services and personalized rehabilitation programs to help you recover effectively and return to your active lifestyle.
What is Osteoarthritis?
Osteoarthritis (OA) is the most common form of arthritis. It is a degenerative joint disease which occurs most frequently in the hands, hips, and knees. It results from the breakdown of cartilage which could cause the ends of bones to rub together, causing pain, stiffness and decreased mobility. In some cases it also causes disability and reduced function.There is no known cure for osteoarthritis but much can be done to reduce its impacts. The cornerstones of treatment for Osteoarthritis are physiotherapy and exercise but knee braces for osteoarthritis and inserts could also help.

What are the different types of knee braces for osteoarthritis?
- Prophylactic knee brace for osteoarthritis helps in prevention of injury especially during sports.
- Offloader or Unloader knee brace for osteoarthritis provide stability, pain relief, and support relief by reducing pressure on key areas.
- Rehabilitative knee brace for osteoarthritis limit movement of a joint to allow time for healing.
- Functional or supportive knee brace for osteoarthritis offers support to the knee joint to help reduce pain and discomfort.
What are the benefits of knee braces for osteoarthritis?
- A knee brace for osteoarthritis aides in the reduction of pressure and relief of discomfort by providing support on the surrounding areas on the knee cap.
- A knee brace for osteoarthritis provides compression which is very beneficial in the reduction of swelling which occurs with arthritis.
- A knee brace for osteoarthritis helps increase joint space in knee joints.
- A knee brace for osteoarthritis provides compression to reduce swelling which is one of the common symptoms in Osteoarthritis.
- A knee brace for osteoarthritis helps by shifting your weight off the most affected portion of the knee joint thus providing reduction of pain and discomfort.
- A knee brace for osteoarthritis allows more mobility while providing comfort and support.
When should I start wearing a knee brace for osteoarthritis?
Once you get diagnosed with knee osteoarthritis, book an appointment with one of our health practitioners who can assess you and recommend the best knee brace for osteoarthritis.