Written by Roshni Ravi, Pelvic Health Physiotherapist
Have you ever experienced pain with sex? A burning sensation during or afterwards, a sharp pain or general discomfort? A lot of these symptoms point towards a common condition called dyspareunia. This is also known as pain with intercourse. It is a common condition postpartum, during menopause or even just due to general pelvic floor dysfunction.
But don’t worry, there are ways to alleviate the discomfort and enjoy a fulfilling sex life again! One of the most effective methods is through pelvic health physiotherapy.
Pelvic health physiotherapy involves working with a trained professional to strengthen and stretch the muscles in your pelvic floor, which can become weakened or tight due to a variety of factors. By doing so, you can improve your pelvic floor function and reduce pain during sex.
When it comes to sexual dysfunction, pelvic physiotherapy can be an effective treatment option for women. Pelvic physiotherapy can help address issues such as pain during intercourse, difficulty achieving orgasm, or vaginismus (involuntary contraction of the vaginal muscles).
What does a treatment session entail?
During a pelvic physiotherapy session, you’ll typically undergo an initial evaluation where your therapist will assess your pelvic floor muscles and create a personalized treatment plan. The exercises and techniques used will vary depending on your specific needs and goals, but they may include:

- Pelvic floor relaxation exercises
- Deep breathing
- Yoga based therapy
- Functional strengthening such as squats
- Biofeedback and/or muscle stimulation
It’s important to note that pelvic physiotherapy isn’t a quick fix and may take several sessions to see results. However, with dedication and commitment, it can significantly improve your quality of life and sexual function. So if you’re experiencing dyspareunia, don’t suffer in silence. Talk to your healthcare provider about pelvic physiotherapy and take the first step towards a happier, healthier you.
Book your consultation with a pelvic health physiotherapist today. We have pelvic health physiotherapists at all eight of our locations.
Where can I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin
“Revitalizing your relationship and reclaiming your sex life can be achieved with the help of pelvic floor physiotherapy. Triangle Physiotherapy offers specialized services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can help you address pelvic floor issues and enhance intimacy through personalized treatment plans.”
Written by Roshni Ravi, Pelvic Health Physiotherapist
Stress incontinence is a type of urinary incontinence that occurs with physical activity or exertion. This can be from coughing, sneezing, laughing or exercise e.g. jumping. All of these actions can put pressure on the bladder thereby causing leaks. The pelvic floor is important in preventing this leaks and supporting the bladder.
Pelvic floor exercises such as a kegel are commonly recommended for leaks. However, a lot of time the pelvic floor is actually tight rather than weak. Reverse Kegels involve relaxing the pelvic floor muscles, allowing them to lengthen and release tension. This helps to prevent over-tightening and over-activity of the pelvic floor muscles, which can contribute to stress incontinence.

Hypertonic pelvic floor
Hypertonic pelvic floor refers to a condition where the pelvic floor muscles are in a state of excessive and persistent contraction. This can lead to a number of symptoms, including pelvic pain, urinary and fecal incontinence, and sexual dysfunction.
Hypertonic pelvic floor can be caused by a number of factors, including pregnancy, childbirth, surgery, chronic constipation, and chronic pelvic pain. It can also be a result of excessive or improper use of pelvic floor muscle exercises, such as Kegels.
Treatment for Hypertonic pelvic floor
Treatment for hypertonic pelvic floor typically involves a combination of physical therapy and relaxation techniques. Physical therapy may include manual therapy to release muscle tension, as well as exercises to stretch and relax the pelvic floor muscles. Relaxation techniques, such as deep breathing, progressive muscle relaxation, and biofeedback, can also be helpful in reducing muscle tension.
If you’re experiencing leaks, reach out to a pelvic floor therapist for an assessment or discovery call!
FAQ’s about Stress Incontinence
Q: What is stress incontinence?
A: Stress incontinence is a type of urinary incontinence that occurs when pressure is placed on the bladder, such as during coughing, sneezing, laughing, or exercising, and causes involuntary urine leakage.
Q: What causes stress incontinence?
A: Stress incontinence is typically caused by weakened pelvic floor muscles and/or a weakened urethral sphincter, which can occur due to aging, pregnancy and childbirth, menopause, obesity, chronic coughing, or certain medical conditions.
Q: Who is at risk for developing stress incontinence?
A: Women are more likely to develop stress incontinence than men, especially those who have gone through pregnancy and childbirth, menopause, or pelvic surgery. Other risk factors include obesity, chronic coughing, and certain medical conditions that affect the bladder or nervous system.
Q: How is stress incontinence diagnosed?
A: Stress incontinence can be diagnosed through a physical exam, a urine test, and other tests such as a bladder diary or urodynamic testing.
Q: What are the treatment options for stress incontinence?
A: Treatment options for stress incontinence may include:
- pelvic floor exercises,
- behavioral therapies,
- medications,
- medical devices such as pessaries, and in some cases,
- surgery.
Q: Can stress incontinence be prevented?
A: While stress incontinence may not be completely preventable, there are steps you can take to reduce your risk. Maintaining a healthy weight, doing regular pelvic floor exercises, and avoiding smoking and excessive caffeine consumption are some of these.
Q: Is stress incontinence a normal part of aging?
A: While stress incontinence is more common in older adults, it is not a normal part of aging and should not be ignored or accepted as an inevitable consequence of getting older. Treatment options are available, and seeking help from a healthcare provider is important.
Managing stress incontinence effectively involves a combination of pelvic floor exercises, lifestyle changes, and sometimes physiotherapy. For those seeking professional physiotherapy services to help manage incontinence and improve pelvic health, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans to help you achieve a leak-free life and enhanced quality of life.
Written by Roshni Ravi, Pelvic Health Physiotherapist
Constipation is a common gastrointestinal (GI) condition that causes difficulty with passing stool or reduces the frequency of having a bowel movement. It can be caused by
– dehydration
– diet e.g. not enough fibre
– sedentary lifestyle
– Ignoring the urge for a bowel movement due to pain.
– Pelvic organ prolapse (POP)
– Medications such as anti-inflammatories, iron supplements or anti depressants.

Medically, constipation is defined as having fewer than 3 bowel movements a week with hard stools.
Pelvic muscle dyssynergia (incoordination) can lead to constipation. During a typical bowel movement, the pelvic floor needs to relax in order to evacuate stool. When there is tightness in the pelvic floor muscles, it can be painful or uncomfortable to pass stool.
Treatment for constipation can include a number of lifestyle modifications such as increased fibre and water intake, and regular exercise. However, consulting with a pelvic physiotherapist can improve outcomes, by creating an exercise program specific to your pelvic floor dysfunction. The need for lengthening versus strengthening of the pelvic floor is determined through internal vaginal or rectal examination. Another option is seeing a naturopath for ways to adjust your diet accordingly. Quite often, both treatments go hand in hand.
Experiencing constipation or constipation like symptoms? Book a consultation with one of our pelvic physiotherapists today!
“Pelvic physiotherapy can be an effective solution for relieving constipation and improving overall pelvic health. Triangle Physiotherapy offers specialized services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can help you develop a personalized treatment plan to address constipation and enhance your quality of life.”
The labour and delivery process can greatly benefit from Pelvic Physiotherapy. Pelvic Physiotherapists can help to improve strength and mobility of the muscles and joints in the pelvic area and help make it easier for the baby to descend through the birth canal during delivery.
FAQs about the Labour and Delivery Process
What are the different stages of Labour and Delivery?
The three stages of labour and delivery are:
- Early Labour: This is from the onset of labor to when the cervix is fully dilated to 3-4 centimeters.
- Active Labour: This is when the cervix is fully dilated to 3-4 centimeters to when it is fully dilated to 10 centimeters.
- Transition: This is when the cervix is fully dilated to 10 centimeters to the delivery of the baby.
How long does labour usually last?
The duration of labour varies from person to person and can range from a few hours to over 24 hours for first-time mothers.
What are the common signs of labour?
The common signs of labour include:
- Regular contractions
- Water breaking
- Back pain
- Pelvic pressure
- Blood-tinged mucus discharge
What is an epidural and how does it work?
An epidural is a type of anesthesia that is used to relieve pain during labor and delivery. It is administered through a small catheter placed in the lower back and works by blocking the sensation of pain in the lower body while allowing the woman to remain conscious.
What is the process of a vaginal delivery like?
A vaginal delivery is the delivery of a baby through the birth canal without the use of surgical intervention. During a vaginal delivery, the baby moves through the birth canal and the mother pushes with contractions to help deliver the baby.
What is a cesarean delivery (C-section)?
Doctors perform a cesarean delivery (C-section) by making an incision in the mother’s abdomen and uterus to deliver the baby. They typically opt for a C-section when a vaginal delivery is not possible or when there is a medical concern for the mother or the baby.
What are some of the risks associated with labour and delivery?
Some of the risks associated with labor and delivery include:
- Preterm labour and delivery
- Hemorrhage
- Infection
- Fetal distress
- Shoulder dystocia (difficulty delivering the baby’s shoulders)
What can I do to prepare for labour and delivery?
You can prepare for labour and delivery by:
- Take childbirth education classes
- See a pelvic health physiotherapist
- Create a birth plan
- Find a supportive birth team like doulas or midwives
- Pack a hospital bag
- Discuss pain management options with your healthcare provider.

The role of Pelvic Health Physiotherapists in preparing you for Labour and Delivery

Pelvic physiotherapy can help to alleviate common pregnancy-related symptoms such as back pain, incontinence, and pelvic pain. A combination of manual therapy techniques with soft tissue and joint mobilization along with mobility work can be used to alleviate pain in the pelvic area, additionally, the physiotherapist can also work on alignment and posture to help prevent injury and reduce discomfort.
Leading up to labour, a pelvic physiotherapist can provide you with a variety of tools to help with pain relief and positioning to improve your experience during labour. One of the common techniques taught to birthing parents at 32 weeks, is the perineal massage to reduce the chance of tearing during delivery. In addition, you would also be taught positions to help reduce discomfort during contractions as well as pushing techniques.
After delivery, a physiotherapist can help restore strength and mobility along with providing education on suitable abdominal and pelvic floor exercises based on weaknesses and tone, moreover, any side effects from delivery such as perineal tearing can also be treated post-partum.
Have questions? Discuss your options with a pelvic health physiotherapist for pregnancy and post-partum care!
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
The journey through labor and delivery can be significantly supported with proper physiotherapy, which helps prepare the body for childbirth and aids in postpartum recovery. If you are looking for professional physiotherapy services to support your pregnancy and postpartum needs, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans to help you through every stage of pregnancy and beyond.
By Roshni Ravi, Pelvic Health Physiotherapist
Endometriosis is a condition in which the tissue that lines the uterus grows outside of it, on other organs or structures in the pelvic cavity. This tissue, called endometrium, acts just like the lining of the uterus and thickens, breaks down, and bleeds with each menstrual cycle. However, because this tissue is located outside of the uterus, it has no way to exit the body, which can lead to pain, heavy bleeding, and the formation of scar tissue and adhesions. Endometriosis can also affect fertility.

What is Endometriosis?
The cause of endometriosis is not well understood. It is usually treated with hormones, pain medication, and surgery. The average delay from symptom onset to diagnosis is 5.4 years in Canada, because of the uncertain etiology. Patients wait for an average of 3.1 years from the onset of symptoms to seeking consultation with their physician.
Some causes for endometriosis may possibly include:
- Retrograde menstruation: some of the endometrial tissue flows backwards through the Fallopian tubes and into the pelvic cavity, and attaches to other organs and structures.
- Embryonic cell growth: develops from cells in the embryonic stage that grow into endometrial tissue instead of into other tissue types
- Immune system dysfunction: some women may have a dysfunction in their immune system that allows endometrial tissue to grow outside the uterus
- Hormonal factors: hormonal imbalances contribute to the development of endometriosis
- Genetic factors
So what can I do about it?
Medical treatment includes surgery, hormonal therapy and medicated pain management. Other alternatives are acupuncture, herbal supplements and pelvic floor physiotherapy.
Pelvic floor physiotherapy can be beneficial for endometriosis. It can help alleviate pain, improve mobility and flexibility as well as reduce the formation of adhesions and scar tissue. Treatment targets the muscles and soft tissue in the pelvic area through techniques such as manual therapy, trigger point release and myofascial release to relax the muscles and thereby alleviate pain. There are a variety of pelvic floor exercises that can also contribute towards alleviating pain and improving symptoms.
Unsure of what to do next but experiencing these symptoms? Consult a pelvic health physiotherapist to see if pelvic floor physiotherapy is right for you. Our Mississauga Pelvic Health Physiotherapists are experienced and qualified to help you through this diagnosis. Book an appointment here.
Disclaimer: This article is for informational purposes only and should not be used for self-diagnosis.
“Recognizing the early signs of endometriosis is crucial for effective management and care. Triangle Physiotherapy offers expert pelvic health services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists provide personalized treatment plans to help you manage endometriosis symptoms and improve your quality of life.”
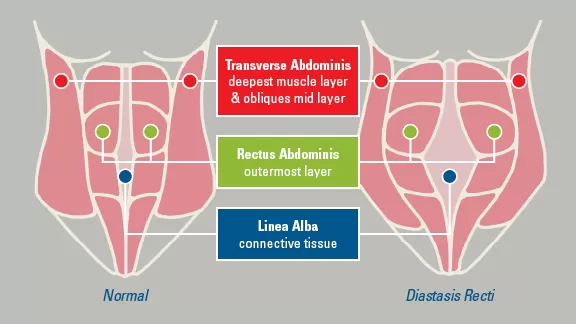
A Diastasis Recti Abdominus is a separation in the 6-pack muscle, the rectus abdominis.
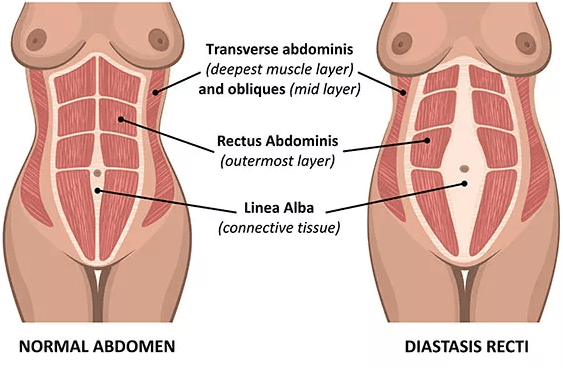
How does it occur?
It most often occurs during pregnancy. Sometimes it will spontaneously correct following birth, but it does not always.
It can also occur with overstretch of abdominal musculature.
Why is it a problem?
There is no pain with this condition.
However, the abdominal wall and the core will become weak. Your abdominals work with your pelvic floor, so a separation of your rectus abdominis muscles can make your pelvic floor less efficient and may result in prolapse and incontinence.Your abdominals also work with your lower back musculature, therefore it can lead to lower back pain.
How do I know if I have a Rectus Diastasis?
If you lift your head while lying on your back and the center of your belly protrudes out, you may have a rectus diastasis. It is measured by the number of fingers you can fit between the muscle when lying on your back and lifting your head. Normal is 1/2 a finger above and below the belly button, and one finger at the belly button.
How do I treat it?
If the abdominal separation is greater than 4 fingers, an abdominal binder is recommended. If you use an abdominal binder, it should be from your hip bones to your rib cage, you need to keep the binder on 24/7. You can only take the binder off when you do your correction exercise below, or when you take a shower. You should keep it on at bedtime.
To get your pelvic health assessed, schedule a consultation with a pelvic floor physiotherapist at Triangle Physiotherapy!
Written by: Kamand Zendeganidoost, Registered Physiotherapist
Managing rectus diastasis effectively often involves specialized physiotherapy to strengthen the core and improve abdominal function. If you are seeking professional physiotherapy services for abdominal separation, consider visiting clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide expert care and personalized treatment plans to help you restore core stability and strength.