Massage therapy involves the manipulation of the body’s soft tissues, including muscles, connective tissues, tendons, ligaments, and skin, to improve a person’s health and well-being. This practice has been used for thousands of years across various cultures and is widely recognized for its numerous benefits.

What is Deep Tissue Massage?
Deep tissue massage is a type of massage therapy that focuses on the deeper layers of muscle and connective tissue. It is especially beneficial for individuals who suffer from chronic pain, muscle tension, or are recovering from an injury. This technique involves the use of slow, deliberate strokes and deep pressure to target specific areas of tension and tightness.
What is Swedish Massage?
Swedish massage is a popular and widely practiced form of massage therapy known for its gentle and relaxing techniques. It focuses on promoting overall relaxation, improving blood flow, and relieving muscle tension. Swedish massage is an excellent choice for those new to massage therapy or looking for a general wellness treatment.
What is the difference between Deep Tissue Massage and Swedish Massage?
Swedish Massage:
- Relaxation: Promotes overall relaxation and reduces stress.
- Circulation: Enhances blood flow and oxygen delivery.
- Muscle Relief: Eases muscle tension and soreness.
- Flexibility: Improves range of motion and flexibility.
- General Wellness: Suitable for maintaining overall health and well-being.
Deep Tissue Massage:
- Pain Relief: Addresses chronic pain and conditions such as lower back pain and neck pain.
- Muscle Tension: Releases deeper layers of muscle tension and knots.
- Injury Recovery: Aids in rehabilitation from injuries by promoting healing and reducing scar tissue.
- Posture Improvement: Corrects muscle imbalances and postural issues.
- Specific Problem Areas: Focuses on targeted areas rather than the whole body.
What are some other types of Massage therapy?
1. Sports Massage
- Focus: Enhances athletic performance and recovery.
- Techniques: Combines Swedish massage, deep tissue, and stretching techniques.
- Benefits: Reduces muscle soreness, improves flexibility, and prevents injuries.
- Ideal For: Athletes and active individuals.
2. Trigger Point Therapy
- Focus: Relieves pain by targeting specific trigger points.
- Techniques: Applies direct pressure to trigger points (knots in the muscles).
- Benefits: Reduces localized pain and referred pain in other areas.
- Ideal For: People with chronic pain and tension.
3. Shiatsu
- Focus: Balances the body’s energy flow.
- Techniques: Uses finger pressure on specific points along the body’s meridians.
- Benefits: Promotes relaxation, reduces stress, and improves energy flow.
- Ideal For: Individuals seeking holistic health benefits and stress relief.
4. Reflexology
- Focus: Stimulates reflex points on the feet, hands, or ears.
- Techniques: Applies pressure to specific points believed to correspond to other body parts.
- Benefits: Enhances overall health and well-being, relieves stress, and improves circulation.
- Ideal For: People looking for non-invasive therapy and overall wellness.
5. Prenatal Massage
- Focus: Supports the health and well-being of pregnant women.
- Techniques: Gentle techniques to relieve pregnancy-related discomfort.
- Benefits: Reduces back pain, improves sleep, and decreases stress and anxiety.
- Ideal For: Pregnant women experiencing discomfort and seeking relaxation.
6. Hot Stone Massage
- Focus: Deep relaxation and muscle tension relief.
- Techniques: Uses heated stones placed on the body and integrated into massage strokes.
- Benefits: Enhances relaxation, improves circulation, and alleviates muscle stiffness.
- Ideal For: Individuals looking for a deeply relaxing experience.
7. Thai Massage
- Focus: Combines acupressure, stretching, and assisted yoga postures.
- Techniques: Performed on a mat, involves rhythmic pressure and stretching.
- Benefits: Increases flexibility, relieves muscle tension, and boosts energy levels.
- Ideal For: People seeking an active and invigorating massage experience.
8. Lymphatic Drainage Massage
- Focus: Stimulates the lymphatic system to remove toxins and waste.
- Techniques: Gentle, rhythmic strokes and light pressure.
- Benefits: Reduces swelling, improves immune function, and detoxifies the body.
- Ideal For: Individuals with lymphedema, post-surgery recovery, or those wanting detoxification.
9. Craniosacral Therapy
- Focus: Works on the craniosacral system to relieve tension.
- Techniques: Gentle touch to manipulate the skull and sacrum.
- Benefits: Reduces stress, alleviates pain, and improves nervous system function.
- Ideal For: People with chronic pain, headaches, or stress-related conditions.
10. Aromatherapy Massage
- Focus: Enhances the massage experience using essential oils.
- Techniques: Combines Swedish or other massage techniques with aromatherapy.
- Benefits: Promotes relaxation, reduces stress, and improves mood.
- Ideal For: Individuals seeking relaxation and mood enhancement.
Click here to book an appointment with a massage therapist at one of our eight locations.
- Massage therapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Massage Therapy Clinic – Triangle Physiotherapy Oakville
- Massage Therapy North York – Triangle Physiotherapy North York
- Mississauga Massage Therapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Massage Therapy Clinics – Triangle Physiotherapy King West
- Uptown Massage Therapy Clinics – Triangle Physiotherapy Lawrence Park
- Massage Therapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- RMT Mississauga – Triangle Physiotherapy Erin Mills
Whether you choose deep tissue or Swedish massage, both can offer significant benefits for relaxation and pain relief. If you’re looking for expert advice on which massage therapy is best for you, consider visiting a physiotherapy clinic in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Professional physiotherapists and massage therapists in these areas can provide the right treatment to help you achieve your wellness goals.
Working and studying from home can take a toll on your body and mind, making it crucial to incorporate some daily movement. Simple actions like walking around your workspace while on a call or standing up while having a snack can help reduce sedentary behavior. Additionally, daily stretching can prevent issues such as “tech neck” and back pain.
How often should you stretch working from home?
When working from home, it’s beneficial to stretch regularly to prevent stiffness and discomfort. Here are some general recommendations:
- Every 30-60 Minutes: Aim to take a short break to stand up, move around, and do some stretches. This helps prevent prolonged periods of inactivity and reduces the risk of musculoskeletal issues.
- Mini Breaks: Take a few minutes every hour to do some simple stretches or walk around. This can help improve circulation and reduce muscle tension.
- Daily Stretching Routine: Incorporate a more comprehensive stretching routine at least once a day, focusing on areas prone to tension such as the neck, shoulders, back, and hips.
By following these guidelines, you can maintain flexibility, reduce the risk of pain, and improve overall well-being while working from home.
What stretches can I do at my desk?
Tricep Stretch
Neck Stretch

Upper Body and Arm Stretch

Trunk Rotation Stretch

Shoulder Shrug Stretch

Stretch Courtesy: https://uwaterloo.ca/campus-wellness/blog/post/desk-stretches
If you are experiencing persistent neck pain, back pain or discomfort, it is advisable to consult a physiotherapist, for proper evaluation and guidance.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Incorporating simple stretches into your routine can help reduce back pain when working from home. For personalized guidance, you can seek physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, where experienced physiotherapists can create a tailored plan to support your back health and overall well-being.
Pubic bone pain after giving birth, also known as postpartum pubic symphysis diastasis or symphysis pubis dysfunction (SPD), is a condition that affects some women following childbirth. This pain is usually centered around the pubic symphysis, the joint at the front of the pelvis where the two halves of the pelvic bone meet.
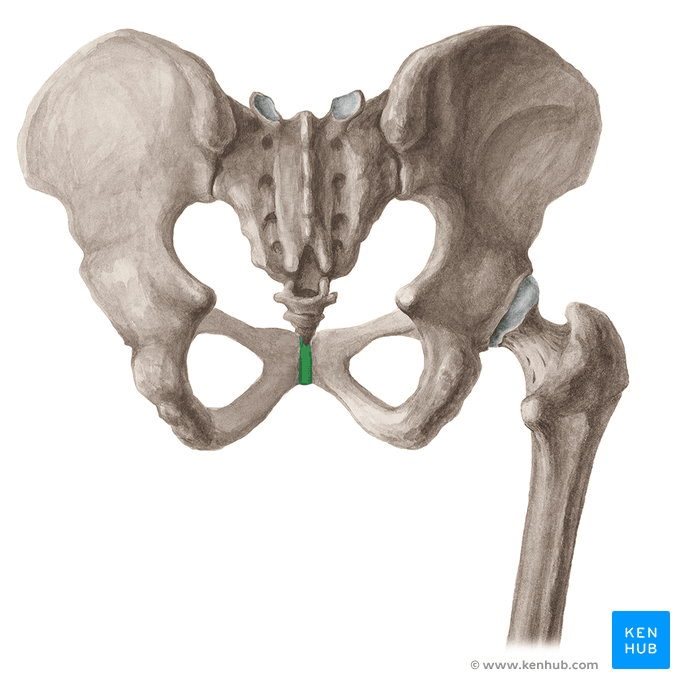
What are the causes of post-partum pubic bone pain?
- Hormonal Changes: During pregnancy, the body releases the hormone relaxin, which loosens the ligaments in the pelvis to prepare for childbirth. This can sometimes lead to instability or separation of the pubic symphysis.
- Physical Stress: The process of labor and delivery can put significant strain on the pelvic area, particularly if the baby is large, labor is prolonged, or delivery involves interventions such as forceps or vacuum extraction.
- Pre-existing Conditions: Women who had SPD or pelvic girdle pain during pregnancy are more likely to experience pubic bone pain postpartum.
What are the symptoms of symphysis pubis dysfunction (SPD)?
Pain:
- Burning, shooting, grinding or stabbing
- Mild or prolonged
- Usually relieved by rest
- Radiating to the back, abdomen, groin, perineum and legs
- Disappears commonly after giving birth (not in every case)
- Discomfort sense onto the front of the joint
- Clicking of the lower back, hip joints and sacroiliac joints when changing position
- Difficulty in movements like abduction and adduction
Locomotor difficulty:
- Walking
- Ascending or descending stairs
- Rising from a chair
- Weight-bearing activities
- Standing on one leg
- Turning in bed
- Depression, possibly due to the discomfort
How is pubic bone pain treated?
- Rest and Activity Modification: Reducing activities that exacerbate pain, such as standing for long periods, lifting heavy objects, or walking long distances.
- Pelvic Physiotherapy: A physiotherapist can provide exercises to strengthen the pelvic floor, abdominal, and hip muscles, and help stabilize the pelvic area. Manual therapy may also be used to realign the pelvis.
- Pain Relief: Over-the-counter pain medications such as acetaminophen or non-steroidal anti-inflammatory drugs (NSAIDs) may be recommended. Always consult with a healthcare provider before taking any medication, especially if breastfeeding.
- Supportive Devices: Wearing a pelvic support belt can help stabilize the pelvis and reduce pain.
- Heat and Cold Therapy: Applying heat or cold packs to the affected area can help reduce pain and inflammation.
How can a pelvic health physiotherapist help with pubic bone pain?
A pelvic health physiotherapist can be of immense help with symphysis pubis dysfunction (SPD). A pelvic health physiotherapist can provide:
- Guidance on movement techniques for daily activities such as climbing stairs, bending, lifting, and feeding the baby.
- Education on gradually advancing exercises aimed at neuromuscular re-education, core stability, and proper posture.
- Hands-on therapy, including pelvic evaluations and muscle energy techniques to correct pelvic alignment.
- Evaluations to identify tissue dysfunction or lack of coordination.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Recovering from pubic bone pain after giving birth can be supported through targeted physiotherapy. If you’re looking for specialized care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can help you manage pain and regain strength and mobility through personalized treatment plans.
Physiotherapy is often recommended before considering surgery for a variety of musculoskeletal conditions and injuries. The decision to try physiotherapy before surgery depends on several factors, including the nature and severity of the condition, the patient’s overall health, and the specific goals of treatment.
What are some of the scenarios where physiotherapy is considered before surgery?
Here are some common scenarios where physiotherapy is advised before opting for surgery:
- Chronic Pain Management:
- Conditions like chronic back pain, neck pain, or osteoarthritis can often be managed with physiotherapy. Techniques such as exercise, manual therapy, and education can help reduce pain and improve function.
- Rehabilitation after Injury:
- For injuries such as sprains, strains, and minor fractures, physiotherapy can aid in healing and restore mobility and strength without the need for surgical intervention.
- Degenerative Joint Diseases:
- For conditions like osteoarthritis, physiotherapy can help maintain joint function, improve strength, and reduce pain, potentially delaying or avoiding the need for joint replacement surgery.
- Sports Injuries:
- Many sports-related injuries, including tendonitis, ligament sprains, and muscle tears, can be effectively treated with physiotherapy. Rehabilitation programs can restore function and allow a safe return to activity.
- Postural and Muscular Imbalances:
- Conditions resulting from poor posture or muscular imbalances, such as certain types of shoulder impingement or knee pain, can often be corrected through targeted physiotherapy exercises and manual therapy.
- Non-Surgical Management of Disc Herniations:
- In cases of herniated discs causing back or neck pain, physiotherapy can help reduce symptoms through specific exercises and modalities, sometimes avoiding the need for surgical intervention.
- Rehabilitation of Neurological Conditions:
- For certain neurological conditions like stroke, multiple sclerosis, or Parkinson’s disease, physiotherapy plays a crucial role in managing symptoms and improving quality of life.
- Post-Surgical Rehabilitation:
- In cases where surgery is eventually necessary, pre-surgical physiotherapy (prehabilitation) can help strengthen the body, improve overall fitness, and enhance recovery post-surgery.
- Conservative Management First:
- For many conditions, especially those where surgery carries significant risks or has variable outcomes, conservative management with physiotherapy is often the first line of treatment to try less invasive options.
What are the benefits of trying physiotherapy before opting for surgery?
Trying Physiotherapy Oakville before opting for surgery offers numerous benefits, both physical and psychological. Here are some key advantages:
Physical Benefits of Physiotherapy
- Pain Reduction:
- Physiotherapy can effectively reduce pain through various techniques such as manual therapy, exercises, and modalities like heat or cold therapy, electrical stimulation, and ultrasound.
- Improved Mobility and Function:
- Targeted exercises and stretches can help improve range of motion, strength, and overall functional ability, allowing patients to perform daily activities with greater ease.
- Enhanced Healing and Recovery:
- Physiotherapy promotes natural healing by improving blood flow, reducing inflammation, and preventing further injury through proper movement patterns.
- Strengthening and Stabilization:
- Physiotherapists design personalized exercise programs to strengthen muscles and stabilize joints, which can prevent the need for surgery by addressing the underlying causes of pain and dysfunction.
- Injury Prevention:
- By improving posture, body mechanics, and muscle balance, physiotherapy can reduce the risk of future injuries.
- Management of Chronic Conditions:
- For chronic conditions like osteoarthritis, physiotherapy can help manage symptoms and slow the progression of the disease, potentially delaying or avoiding the need for surgery.
Psychological and Emotional Benefits
- Reduced Anxiety and Stress:
- The prospect of surgery can be daunting. Physiotherapy offers a non-invasive approach that can alleviate anxiety and stress related to surgical procedures and recovery.
- Increased Confidence and Empowerment:
- Patients often feel more in control of their health when actively participating in their treatment through physiotherapy, leading to improved mental well-being.
- Better Understanding of Condition:
- Physiotherapists educate patients about their condition and the mechanics of their body, providing them with knowledge and strategies to manage their symptoms effectively.
Economic and Practical Benefits
- Cost-Effective:
- Physiotherapy is generally less expensive than surgery and associated hospital stays, making it a cost-effective alternative for many patients.
- Reduced Recovery Time:
- While surgery often requires significant recovery time, physiotherapy allows patients to continue their daily activities with minimal interruption, enhancing their quality of life.
- Avoiding Surgical Risks:
- Surgery carries inherent risks such as infection, complications from anesthesia, and prolonged recovery periods. Physiotherapy avoids these risks by offering a non-invasive treatment option.
- Trial of Conservative Management:
- Trying physiotherapy first allows for the possibility that conservative management might be sufficient. If it proves ineffective, surgery can still be considered as a subsequent option.
Long-term Health Benefits
- Development of Healthy Habits:
- Physiotherapy encourages the adoption of healthy habits and exercises that can contribute to long-term well-being and prevent future issues.
- Maintenance of Physical Fitness:
- Ongoing physiotherapy helps maintain physical fitness, flexibility, and strength, contributing to overall health and resilience against other potential health issues.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Trying physiotherapy before opting for surgery can be a beneficial step in managing pain and improving function. If you’re considering this approach, you can find expert physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village to help you explore non-surgical options and make informed decisions about your health.
Breast cancer and pelvic health are two significant aspects of women’s health that can intersect in various ways. Breast cancer treatment can affect your bladder, sexual and/or pelvic function. Anywhere between 50 to 70 per cent of women will experience these kinds of issues after treatment.1
What are the known risk factors for Breast Cancer?
Risk Factors:
- Genetics: Family history, BRCA1 and BRCA2 gene mutations.
- Hormonal factors: Early menstruation, late menopause, hormone replacement therapy.
- Lifestyle factors: Alcohol consumption, obesity, lack of physical activity.
- Age: Risk increases with age.
What are the most common symptoms of Breast Cancer?
Symptoms:
- Lumps in the breast or underarm
- Changes in breast shape or size
- Skin dimpling or irritation
- Nipple discharge
How is Pelvic Health connected to Breast Cancer?

Many types of breast cancer are estrogen-positive, which means higher estrogen levels in the blood can increase cancer risk. Treatment for these cancers often involves medication that blocks estrogen reception to slow or delay cancer growth. Although this approach is effective against estrogen-positive breast cancer, it can impact pelvic floor health. One common side effect is vaginal dryness, which can adversely
affect the health of the vulvar and vaginal tissues. Incontinence, pelvic pain, sexual dysfunction can occur as a side effect of cancer treatments and these are conditions a pelvic health physiotherapist can help with.
How does estrogen affect the pelvic floor?
Breast cancer treatments that lead to lower levels of estrogen in the body which can induce symptoms similar to menopause. Estrogen is important for vaginal health because it keeps the tissues plump, pliable and lubricated. Hormone treatment, chemotherapy and/or ovary suppression or removal can all decrease estrogen levels in the body. Lower estrogen levels can lead to the thinning of vaginal tissues, vaginal dryness, burning, itching, an increased urge to urinate, the leakage of urine, recurring urinary tract infections, pelvic pressure, discomfort and pain with sexual activity.
How can I relieve pelvic pain during breast cancer treatment?
If you experience pelvic pain or pressure during treatment, consider these strategies to alleviate the discomfort:
- Engage in an exercise routine, provided your healthcare provider approves. Physical activity, such as walking, jogging, or yoga, can be beneficial.
- Use cold or hot compresses to help ease the pain.
- Take over-the-counter medications, but only if they are approved by your doctor.
- Perform pelvic floor exercises as recommended by your pelvic floor physiotherapist.
Where can I find a pelvic health physiotherapist in Mississauga?
We have 8 locations with pelvic health physiotherapists to help you.
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
Understanding the connection between breast cancer and pelvic health is crucial for comprehensive care. If you’re looking for expert support, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can help address pelvic health concerns and support you through every step of your recovery journey.
Physiotherapy is a vital field in healthcare. Physiotherapists are healthcare professionals that can help people of all ages live a healthy lifestyle.

Here are seven common myths about physiotherapy debunked:
1. Myth: Physiotherapy is only for injuries.
Reality: While physiotherapy is indeed crucial for injury recovery, it is also beneficial for managing chronic conditions, post-surgical rehabilitation, preventive care, and enhancing athletic performance. Physiotherapists work with patients across various stages of life and health conditions to improve mobility and quality of life.
2. Myth: Physiotherapy is just about exercise.
Reality: Physiotherapy encompasses a wide range of treatments beyond exercises, including manual therapy, electrical stimulation, ultrasound therapy, dry needling, and patient education. These modalities are tailored to address specific conditions and patient needs.
3. Myth: Physiotherapy is painful.
Reality: While some discomfort might be involved, especially when working through injuries or stiffness, physiotherapists aim to minimize pain and improve function. They use techniques that manage pain effectively and strive to make the rehabilitation process as comfortable as possible.
4. Myth: You need a referral to see a physiotherapist.
Reality: In Ontario, you can directly access physiotherapy services without a doctor’s referral. This direct access allows for quicker intervention and treatment, which can be crucial for recovery and pain management. However, you must check with your insurance provider if they need a doctor’s referral to reimburse any treatment fees.
5. Myth: Physiotherapy is only for older people.
Reality: Physiotherapy benefits people of all ages. Children with developmental issues, athletes needing performance enhancement, adults recovering from surgeries, and elderly individuals managing arthritis all benefit from physiotherapy.
6. Myth: Once you start physiotherapy, you’ll need it forever.
Reality: Physiotherapy aims to empower patients with the knowledge and exercises to manage their conditions independently. Many patients achieve their goals and maintain their progress through self-management techniques learned during therapy.
7. Myth: All physiotherapists are the same.
Reality: Physiotherapists specialize in different areas such as sports physiotherapy, pediatric physiotherapy, pelvic health physiotherapy, geriatric physiotherapy, cardiopulmonary physiotherapy, and more. Their training and expertise can vary widely, and it’s essential to find a therapist whose specialization aligns with your specific needs.
Understanding these myths helps in recognizing the comprehensive and essential role of physiotherapy in healthcare, encouraging individuals to join Physiotherapy Oakville for appropriate care and optimal health outcomes.
How do I book an appointment at a Triangle Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Debunking myths about physiotherapy helps more people understand its benefits for pain management and overall health. If you’re looking for reliable physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village, there are qualified physiotherapists available to provide expert care and help you achieve your wellness goals.
Orthotics are inserts or devices worn inside footwear to provide support, correct foot abnormalities, and alleviate discomfort or pain associated with various foot conditions. They can be made from various materials like foam, rubber, plastic, or even metal, depending on the specific needs of the individual. Orthotics are often prescribed by chiropodists or other healthcare professionals to address issues such as flat feet, high arches, plantar fasciitis, bunions, arthritis, and other biomechanical imbalances in the feet and lower limbs. They can help improve alignment, distribute pressure more evenly, and enhance overall foot function, leading to reduced pain and improved mobility.
What are Custom-Made Orthotics?

What are over-the-counter Orthotics?
In contrast to custom foot orthotics, standard over-the-counter options are manufactured in bulk and available for purchase at pharmacies, grocery stores, and various retail outlets.
What are the pros and cons of Custom-Made Orthotics and Over-The-Counter Orthotics?
Custom Made Orthotics
PROS
- Tailored Fit: Custom-made orthotics are crafted specifically for the individual’s foot shape and biomechanics, ensuring optimal support and comfort.
- Targeted Correction: They can address specific foot conditions, such as
over-pronation or high arches, with precise corrections tailored to the
patient’s needs. - Enhanced Effectiveness: Custom orthotics are often more effective at relieving pain and improving foot function compared to over-the-counter options.
- Longevity: They are typically made from durable materials and can last for a longer period with proper care and maintenance.
CONS
- Cost: Custom-made orthotics can be expensive, especially in comparison to their OTC counterparts
- Time-Consuming Process: The process of obtaining custom orthotics
involves multiple appointments and measurements, which can take time. - Adjustment Period: Patients may require some time to get used to wearing
custom orthotics, and adjustments may be needed to achieve the desired
comfort and effectiveness.
Over-the-Counter Orthotics
PROS
- Accessibility: Over-the-counter orthotics are readily available at
pharmacies, retail stores, and online, making them convenient to
purchase without the need for a prescription or specialized fitting. - Affordability: They are generally more affordable than custom-made
orthotics, making them a cost-effective option for individuals on a
budget. - Immediate Use: Over-the-counter orthotics can be used right away without the need for a waiting period or multiple appointments.
CONS
- Limited Customization: Over-the-counter orthotics are not tailored to
the individual’s specific foot shape and biomechanics, which may result
in less precise support and correction. - Less Effective: They may not provide the same level of pain relief or
improvement in foot function as custom-made orthotics, especially for
more severe foot conditions. - Durability: Over-the-counter orthotics may not be as durable as custom-made ones and may need to be replaced more frequently.
- Potential Discomfort: Some over-the-counter orthotics may cause
discomfort or exacerbate existing foot issues if they do not fit
properly or provide adequate support.
Click here to book an appointment with a chiropodist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Choosing the right orthotics, whether custom-made or over-the-counter, is crucial for foot health and comfort. For those looking to enhance their treatment with professional physiotherapy services, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and customized treatment plans to help you achieve optimal foot health and overall well-being.
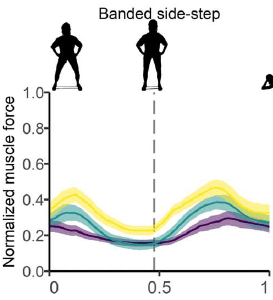
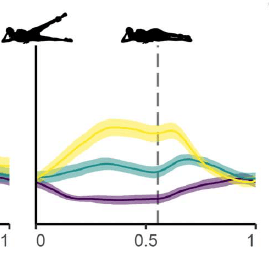
Glute exercises are fantastic for improving overall lower body strength, stability, and athletic performance. The gluteal muscles exert significant effort in maintaining alignment, contributing to both posture and movement, enhancing strength, and providing support to adjacent muscle groups as well.
Why are strong Glutes important?
Strong glutes are essential for various reasons:
- Improved Posture: Strong glutes help maintain proper alignment of the pelvis, which is crucial for good posture. Weak glutes can contribute to postural imbalances and increase the risk of lower back pain and injury.
- Enhanced Athletic Performance: The glutes are powerhouse muscles involved in many movements, including running, jumping, and lifting. Strengthening them can improve performance in sports and other physical activities.
- Prevention of Injuries: Strong glutes can help stabilize the pelvis and knees, reducing the risk of injuries such as ACL tears, IT band syndrome, and lower back pain. They also provide support during movements that involve rotation or lateral movements.
- Increased Strength: The glutes are one of the largest muscle groups in the body. Strengthening them can improve overall lower body strength, making daily tasks easier and enhancing functional fitness.
- Better Aesthetic Appearance: Developed glute muscles contribute to a toned and sculpted lower body appearance. Many people aim to strengthen their glutes for aesthetic reasons as well as functional benefits.
What muscles make up the Glutes?
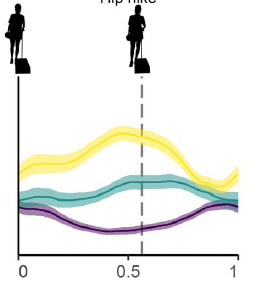
Gluteal Muscles. The Maximus (yellow), medius (blue) and minimus (red).
The glutes, or gluteal muscles, are comprised of three main muscles:
- Gluteus Maximus: This is the largest muscle in the gluteal group and one of the strongest muscles in the human body. It forms much of the shape and appearance of the buttocks. The gluteus maximus is primarily responsible for hip extension, such as when you stand up from a seated position or climb stairs.
- Gluteus Medius: Located on the outer surface of the pelvis, the gluteus medius is responsible for hip abduction (moving the leg away from the body’s midline) and internal rotation of the hip joint. It plays a crucial role in stabilizing the pelvis during activities like walking, running, and standing on one leg.
- Gluteus Minimus: This smaller muscle lies beneath the gluteus medius and has similar functions, assisting in hip abduction and internal rotation. It also helps stabilize the pelvis and maintain balance during movement.
Together, these muscles work synergistically to provide stability, power, and mobility to the hips and lower body. Strengthening all three muscles is essential for overall lower body strength, function, and injury prevention.
8 Glute Exercises you can do at home
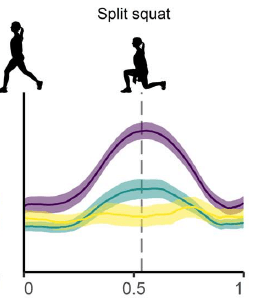
Single Leg Squat
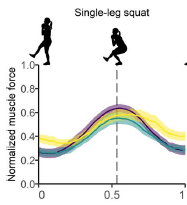
Split Squat

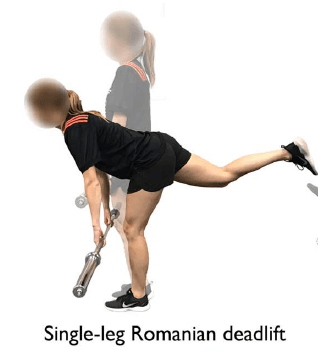
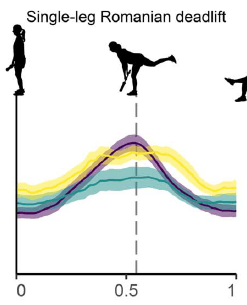
Single-Leg Romanian Dead Lift
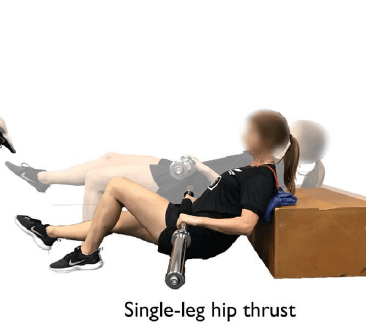
Single-Leg Hip Thrust
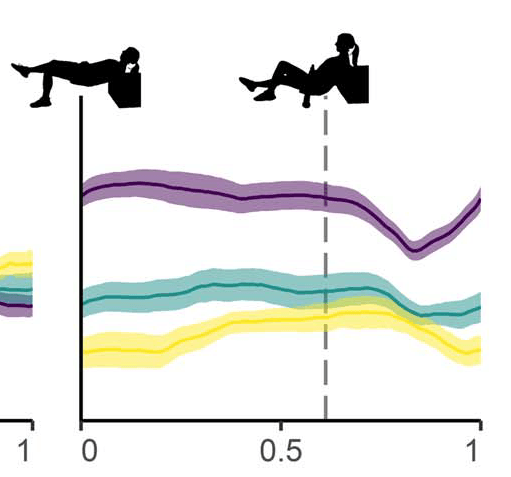
Banded Side-Step

Side-Lying Leg Raise


Side-Plank
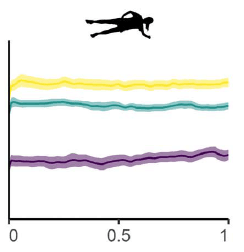
Ref: Gluteal Muscle Forces during Hip-Focused Injury Prevention and Rehabilitation Exercises
TYLER J. COLLINGS, MATTHEW N. BOURNE, ROD S. BARRETT, EVY MEINDERS, BASÍLIO A. M. GONÇALVES, ANTHONY J. SHIELD, and LAURA E. DIAMOND School of Health Sciences and SocialWork, Griffith University, Gold Coast Campus, Queensland, AUSTRALIA
It is important that you avoid injury while doing any type of exercise. Make sure you consult your physiotherapist at Physiotherapy Oakville throughout your workout journey to ensure you are doing the exercises correctly and avoiding injury.
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Strengthening your glutes with at-home exercises is a great way to improve your overall fitness. For personalized guidance, Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our physiotherapists can help you create a tailored exercise plan to meet your specific needs.”
Arthritis is a term used to describe inflammation of one or more joints, leading to pain, stiffness, and decreased mobility. There are many types of arthritis, but the two most common are osteoarthritis and rheumatoid arthritis.
What are the two most common types of Arthritis?
- Osteoarthritis (OA): This is the most common form of arthritis, often associated with aging or wear and tear on the joints. In OA, the protective cartilage that cushions the ends of bones wears down over time, leading to pain, swelling, and stiffness in the affected joint. Osteoarthritis can affect any joint but commonly occurs in the hands, knees, hips, and spine.
- Rheumatoid Arthritis (RA): Unlike osteoarthritis, rheumatoid arthritis is an autoimmune disorder in which the body’s immune system mistakenly attacks the synovium, the lining of the membranes that surround the joints. This leads to inflammation, joint damage, and eventually erosion of the bone and cartilage. RA commonly affects the joints in the hands, wrists, and feet and can cause systemic symptoms such as fatigue, fever, and weight loss.
What are the causes of Arthritis?
While the causes of some forms of arthritis are unknown, arthritis can be caused by disease, injury, overuse and genetic predisposition.
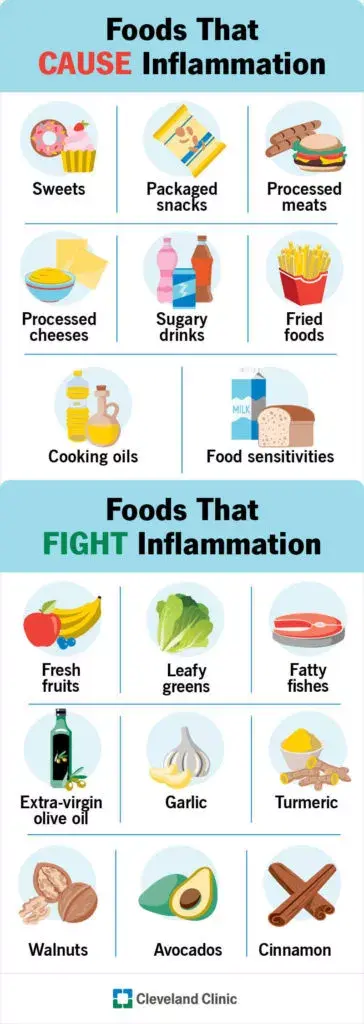
What are 8 foods to avoid when you have arthritis?
When managing arthritis, it’s often recommended to avoid certain foods that may exacerbate inflammation or contribute to joint pain. Here are eight foods commonly suggested to avoid:
- Processed Foods: Foods high in processed sugars, refined carbohydrates, and unhealthy fats can contribute to inflammation. These include fast foods, sugary snacks, and processed meats.
- Saturated and Trans Fats: Foods high in saturated and trans fats, such as fried foods, processed snacks, and fatty cuts of meat, can promote inflammation and worsen arthritis symptoms.
- High Sodium Foods: Excessive sodium intake can lead to water retention and inflammation, potentially aggravating arthritis symptoms. Processed foods, canned soups, and salty snacks are common sources of high sodium.
- Nightshade Vegetables: Some individuals with arthritis find that nightshade vegetables like tomatoes, eggplants, peppers, and potatoes can worsen their symptoms. While more research is needed, some believe that certain compounds in these vegetables may contribute to inflammation in susceptible individuals.
- Gluten: For some people with arthritis, particularly those with rheumatoid arthritis, gluten may exacerbate inflammation and joint pain. Gluten is found in wheat, barley, rye, and products made from these grains.
- Dairy Products: Some people with arthritis may find that dairy products worsen their symptoms. While the evidence is mixed, some studies suggest that certain proteins in dairy may contribute to inflammation in susceptible individuals.
- Alcohol: Excessive alcohol consumption can lead to inflammation and may worsen arthritis symptoms. Additionally, alcohol can interact with some medications used to treat arthritis.
- Sugar-Sweetened Beverages: Sugary drinks like sodas and fruit juices can contribute to inflammation and weight gain, which may exacerbate arthritis symptoms. Opting for water, herbal teas, or unsweetened beverages is a better choice.
It’s important to note that individual responses to these foods can vary, and it may be helpful to keep a food diary to identify any specific triggers. Additionally, maintaining a balanced diet rich in fruits, vegetables, lean proteins, and healthy fats is generally beneficial for managing arthritis symptoms. Consulting with a healthcare professional or a registered dietitian for personalized dietary advice is also recommended.
What foods can I eat when I have arthritis?
Here are some foods that are often recommended for people with arthritis:
- Fatty Fish: Fatty fish like salmon, mackerel, sardines, and trout are rich in omega-3 fatty acids, which have anti-inflammatory properties. Consuming fatty fish regularly may help reduce inflammation and alleviate arthritis symptoms.
- Fruits and Vegetables: Colorful fruits and vegetables are high in antioxidants and other nutrients that can help reduce inflammation and promote overall health. Aim for a variety of fruits and vegetables, including berries, cherries, oranges, leafy greens, broccoli, and bell peppers.
- Whole Grains: Whole grains like brown rice, quinoa, oats, and whole wheat are rich in fiber and nutrients that can help support joint health. Choose whole grains over refined grains to maximize nutritional benefits.
- Nuts and Seeds: Nuts and seeds, such as almonds, walnuts, flaxseeds, and chia seeds, are good sources of healthy fats, protein, and antioxidants. They can help reduce inflammation and provide essential nutrients for joint health.
- Legumes: Legumes like beans, lentils, and chickpeas are rich in protein, fiber, and various vitamins and minerals. They can be a nutritious and filling addition to meals, providing plant-based protein and promoting overall health.
- Legumes: Legumes like beans, lentils, and chickpeas are rich in protein, fiber, and various vitamins and minerals. They can be a nutritious and filling addition to meals, providing plant-based protein and promoting overall health.
- Herbs and Spices: Certain herbs and spices have anti-inflammatory properties and can add flavor to meals without extra salt or unhealthy fats. Examples include turmeric, ginger, garlic, cinnamon, and rosemary.
- Dairy Alternatives: For individuals sensitive to dairy, alternatives like fortified plant-based milk (e.g., almond milk, soy milk) and dairy-free yogurt or cheese can provide calcium and other nutrients without exacerbating arthritis symptoms.
What is the best treatment for arthritis?
It’s important for individuals with arthritis to work closely with their healthcare providers to develop a comprehensive treatment plan tailored to their specific needs and preferences. This may involve a combination of medication, physiotherapy, lifestyle modifications, and other interventions to effectively manage symptoms and improve quality of life.
How do I book an appointment at a Triangle Physiotherapy Clinic near me?
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Managing arthritis involves not only proper diet but also effective physical therapy. For comprehensive care, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can help manage arthritis symptoms and improve your quality of life through tailored treatment plans.
Ankle rehabilitation through physiotherapy involves a systematic approach to regaining strength, flexibility, stability, and functionality after an ankle injury. Here’s a step-by-step guide:
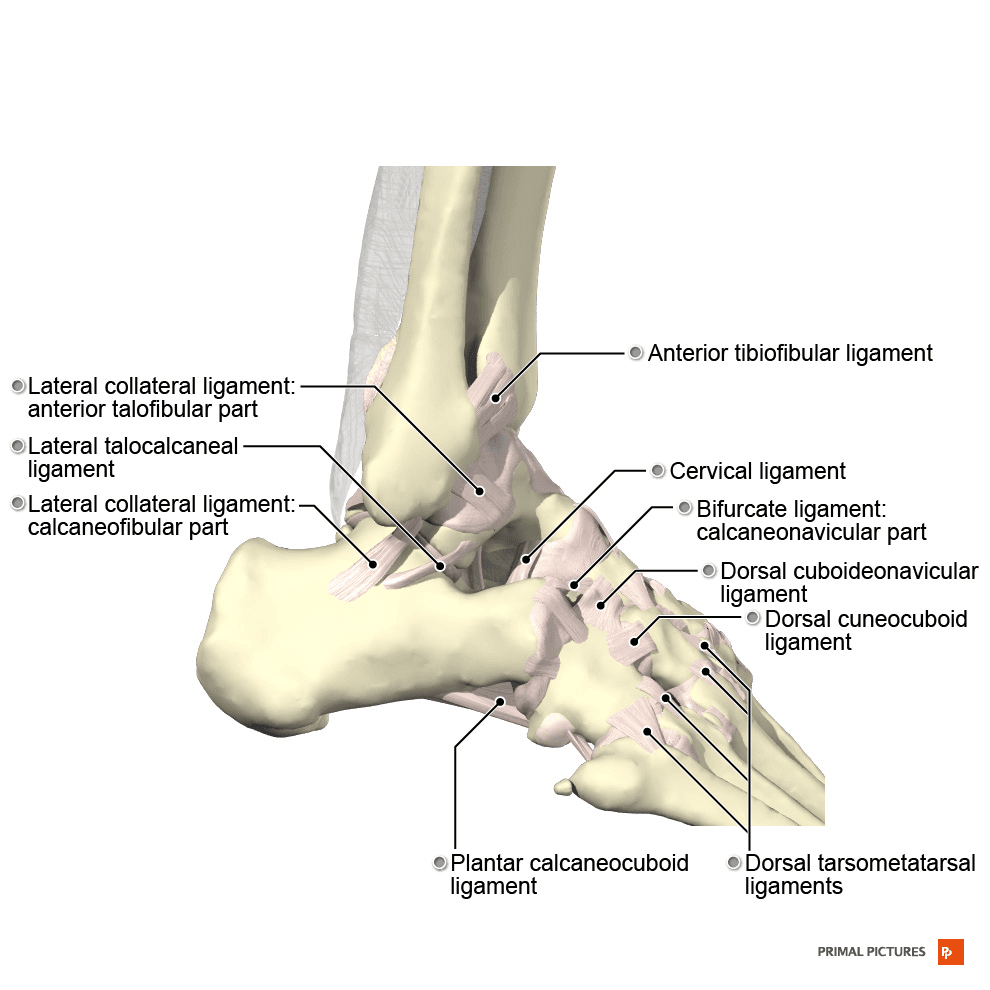
Ankle Anatomy and Injury Overview
Ankles are complex joints that connect the lower leg bones (the tibia and fibula) to the foot bones (the talus and calcaneus). The anatomy of the ankle includes bones, ligaments, tendons, and muscles, all of which work together to provide stability, support, and mobility.
Common Ankle Injuries
- Sprains: Ankle sprains occur when the ligaments are stretched or torn, usually due to an inversion or eversion injury. Lateral ankle sprains, involving the ligaments on the outside of the ankle, are more common than medial ankle sprains.
- Fractures: Fractures can occur in any of the ankle bones, typically as a result of trauma or excessive force. The lateral malleolus (part of the fibula) and the medial malleolus (part of the tibia) are commonly fractured in ankle injuries.
- Achilles Tendon Rupture: This injury involves a tear or rupture of the Achilles tendon, often occurring during activities that involve sudden forceful plantarflexion of the foot.
- Tendinitis: Inflammation of the tendons around the ankle, such as the Achilles tendon or the peroneal tendons, can result from overuse, improper footwear, or biomechanical issues.
Why Physiotherapy for Ankle Rehabilitation?
Physiotherapy is a crucial component of ankle rehabilitation for several reasons:
- Expert Assessment: Physiotherapists are trained to assess musculoskeletal conditions and movement dysfunctions. They can accurately diagnose the extent and nature of the ankle injury, identifying specific impairments and deficits that need to be addressed.
- Individualized Treatment Plans: Physiotherapists develop personalized treatment plans tailored to each patient’s needs, considering factors such as the severity of the injury, functional limitations, and personal goals. This ensures that rehabilitation is targeted and effective.
- Pain Management: Ankle injuries often result in pain and inflammation. Physiotherapists employ various modalities and techniques to manage pain, such as manual therapy, modalities like ultrasound or electrical stimulation, and therapeutic exercises designed to alleviate discomfort.
- Restoration of Function: Physiotherapy aims to restore optimal function to the ankle joint. Therapists use a combination of exercises, manual therapy, and functional activities to improve range of motion, strength, flexibility, and proprioception.
- Prevention of Complications: Without proper rehabilitation, ankle injuries can lead to complications such as chronic pain, stiffness, weakness, instability, and increased risk of re-injury. Physiotherapy helps prevent these complications by promoting optimal healing and restoring normal function.
- Optimizing Recovery Time: Physiotherapy can expedite the recovery process by facilitating tissue healing, reducing swelling, and promoting efficient movement patterns. This can help patients return to their normal activities, work, and sports sooner than if they were to rely solely on rest and self-management.
- Education and Empowerment: Physiotherapists educate patients about their injury, rehabilitation process, and strategies for injury prevention. By understanding their condition and how to manage it, patients feel empowered to take an active role in their recovery and make informed decisions about their health.
- Customized Rehabilitation Programs: Physiotherapists design comprehensive rehabilitation programs that evolve as the patient progresses. These programs include a combination of therapeutic exercises, manual therapy, modalities, and functional training tailored to address the specific needs and goals of the individual.
- Coordination of Care: Physiotherapists often work closely with other healthcare professionals, such as orthopedic surgeons, sports medicine physicians, and athletic trainers, to ensure comprehensive and coordinated care for the patient. This multidisciplinary approach optimizes outcomes and promotes continuity of care.
Step-by-Step Ankle Rehabilitation Through Physiotherapy

Step 1: Initial Assessment
Our physiotherapist will conduct a thorough assessment of your condition, including a detailed medical history review and a physical examination. This step helps us understand your specific concerns and develop an appropriate treatment plan.
Step 2: Pain Management
Physiotherapy plays a significant role in pain management through various techniques and modalities tailored to each individual’s needs.
Pain management techniques that may be used in your rehabilitation are:
- Heat/Cold Therapy
- Manual Therapy
- Electrotherapy
- Education and self-management strategies
- Activity modification
Step 3: Range of Motion Exercises
Step 4: Strengthening Exercises
Step 5: Balance and Proprioception
Step 6: Education and Prevention
Click here to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Effective ankle rehabilitation requires expert physiotherapy care. Triangle Physiotherapy offers specialized services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team is here to help you recover strength, mobility, and confidence in your ankles.”









