Yes, physiotherapy can help with knee pain.
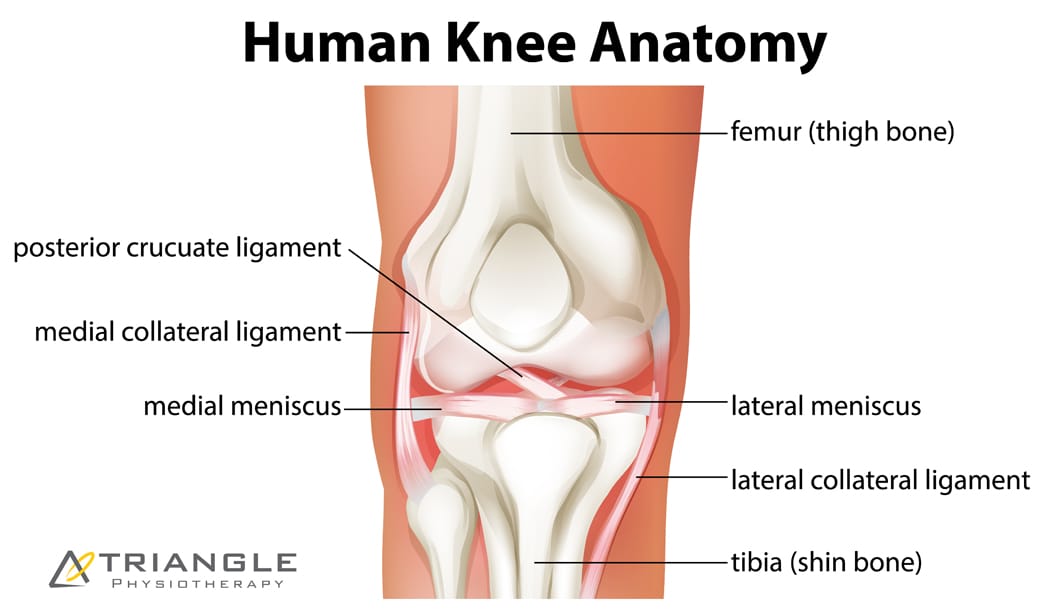
Knee pain is a very common complaint, and is something that can originate from many different structures in and around the knee. The knee joint is made up of the interaction between the femur (thigh), the tibia (shin), and the patella (kneecap). All the tissues around these areas can be contributing to your knee pain.
How does physiotherapy help with knee pain?
Here are some ways in which physiotherapy can help with knee pain:
- Pain management: Physiotherapists can utilize various modalities such as manual therapy, heat or cold therapy, and electrical stimulation to help alleviate pain and reduce inflammation in the knee joint.
- Exercise prescription: Specific exercises can be prescribed to strengthen the muscles around the knee joint, improve flexibility, and enhance joint stability. These exercises help restore normal movement patterns, reduce stress on the knee joint, and promote healing.
- Manual therapy: Physiotherapists may use hands-on techniques like joint mobilization or soft tissue massage to improve joint mobility, reduce muscle tension, and enhance circulation in the knee area.
- Education and self-management: Physiotherapists provide education about proper body mechanics, posture, and ergonomics to prevent further knee pain or injury. They may also offer guidance on activity modification and self-management strategies to promote long-term knee health.
- Assistive devices and bracing: If necessary, physiotherapists can recommend and provide appropriate assistive devices such as knee braces or orthotics to support the knee joint and reduce pain during movement.
What are the causes of knee pain?
Knee pain can have various causes, ranging from acute injuries to chronic conditions. Here are some common causes of knee pain:
- Acute injuries: Knee pain can result from sudden injuries, such as sprains, strains, ligament tears (such as anterior cruciate ligament or ACL tears), meniscus tears, or fractures. These injuries often occur during sports activities, accidents, or falls.
- Overuse or repetitive strain: Repetitive activities or excessive stress on the knee joint can lead to overuse injuries. Examples include patellofemoral pain syndrome (pain around the front of the knee), iliotibial band syndrome (inflammation of the band of tissue on the outside of the knee), or tendinitis (inflammation of a tendon, such as patellar tendinitis or jumper’s knee).
- Osteoarthritis: This is a degenerative joint disease characterized by the breakdown of cartilage in the knee joint. It is more common in older individuals and can cause knee pain, stiffness, and swelling.
- Rheumatoid arthritis: Unlike osteoarthritis, rheumatoid arthritis is an autoimmune condition that causes inflammation and damage to the joints, including the knee. It can lead to chronic pain, joint deformity, and functional limitations.
- Bursitis: Bursae are small fluid-filled sacs that cushion and reduce friction between tendons, ligaments, and bones. When the bursae become inflamed (bursitis), it can cause knee pain, swelling, and limited mobility.
- Patellar dislocation or instability: This occurs when the kneecap (patella) slips out of its normal position, often due to a sudden change in direction or a direct blow to the knee. It can cause severe pain, swelling, and instability.
- Gout: Gout is a type of arthritis caused by the buildup of uric acid crystals in the joints. It can affect the knee joint, leading to sudden and intense pain, redness, and swelling.
- Tumors: Although rare, tumors can develop in the bones or soft tissues around the knee joint, leading to knee pain and swelling.
What are some of the conditions associated with knee pain?
Some of the conditions associated with knee pain are:
- Patellar Tendonitis
- Patellofemoral Syndrome
- Osgood Schlatter Syndrome
- Knee Bursitis
- Knee osteoarthritis
- Baker’s Cyst
- Knee Ligament Injuries
How to treat knee pain at home
You can treat knee pain at home by doing some of the following:
- Rest: Avoid activities that aggravate the pain and give your knee sufficient rest. This can help reduce inflammation and promote healing.
- Ice therapy: Apply ice packs wrapped in a thin cloth to the affected knee for about 15-20 minutes at a time, several times a day. This can help reduce pain and swelling. Be sure to allow your knee to warm up between icing sessions.
- Compression: Use a compression bandage or knee brace to provide support and reduce swelling. However, make sure it’s not too tight to restrict circulation.
- Elevation: Elevate your leg and place a pillow under your knee to help reduce swelling.
- Over-the-counter pain relievers: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, can help relieve pain and reduce inflammation. Follow the instructions on the package and consult with a pharmacist if you have any concerns.
- Gentle exercises: Once the acute pain and swelling have subsided, gentle range-of-motion exercises and stretching can help improve mobility and reduce stiffness. However, avoid any exercises that cause pain or discomfort. Consult with a physiotherapist for appropriate exercises.
If you’re experiencing knee pain, it’s recommended to consult with a healthcare professional, such as a physician or physiotherapist, for an accurate diagnosis and appropriate treatment.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Physiotherapy is a highly effective approach for managing and alleviating knee pain, whether due to injury or chronic conditions. Triangle Physiotherapy provides expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can develop a personalized treatment plan to help you reduce pain, improve mobility, and enhance your quality of life.”
Physiotherapy is an evidence-based regulated healthcare profession that aims to maintain, restore and improve your function after disease or injury, so you can get back to doing what you love and enjoy an injury-free lifestyle that doesn’t hold you back.
Physiotherapists are primary healthcare professionals with a significant role in health promotion and treatment of injury and disease.
They combine their in-depth knowledge of the body and how it works with specialized hands-on clinical skills to assess, diagnose and treat symptoms of illness, injury, or disability.

What is the average cost of physiotherapy near me?
The cost of physiotherapy depends on the appointment type and setting.
An initial assessment at a private practice typically costs between $120 to $150 in the Greater Toronto Area. Follow-ups at a private practice may cost between $80 and $110 per session. The numbers will vary based on the location of the clinics and various other factors.
What are the contributing factors to the cost of physiotherapy near me?
The cost of physiotherapy services is driven by factors such as:
- Type of service provided
- Length of session
- Physiotherapist’s specialty (Pelvic Health, Vestibular, and Concussion Rehab)
- The geographical location of the clinic
- Insurance reimbursement rates
Does insurance cover Physiotherapy?
Insurance plans may cover physiotherapy but every insurance plan is different, so, it may be prudent to check the details of your plan. Some questions to ask your insurance provider are:
- What is the annual coverage limit for physiotherapy?
- Is there a per-visit maximum, if any?
- Are there any required co-payments?
- Is the fee covered 100%?
- Is there a deductible?
How much will my physiotherapy treatments cost in total?
The cost of physiotherapy depends on the type and complexity of your injury or condition that is being treated as well as the treatment plan that your physiotherapist designs for you while keeping in mind your goals for recovery.
Why do I need to be treated by a registered physiotherapist?
It is of utmost importance to ensure that you are being seen by a registered Physiotherapist because behind every registered Physiotherapist are years of academic and clinical training as well as extensive knowledge of all the systems of the human body. At our physiotherapy center, we guarantee that every single physiotherapist we have is registered with the College of Physiotherapists of Ontario and will take excellent care of you.
Who do I speak to about the cost of physiotherapy near me?
Contact our patient care coordinator team at any of our eight locations. They will help you with any insurance-related questions you may have as well as match you with a physiotherapist best suited for your injury or condition.
Is it worth it to see a physiotherapist?
Seeing a physiotherapist can be very beneficial in many situations. Physiotherapy is a healthcare profession that focuses on improving and restoring physical function and mobility. Whether it’s addressing a specific injury, managing chronic pain, or enhancing overall physical well-being, a physiotherapist can provide valuable guidance and treatment.
Joining Physiotherapy Oakville offers you access to a team of skilled professionals who utilize evidence-based practices to tailor treatments to your specific needs. Scientific studies have shown that physiotherapy can significantly improve recovery times and physical outcomes. By becoming a part of Physiotherapy Oakville, you benefit from personalized care plans that enhance your physical health, help manage pain effectively, and support your overall well-being, ensuring you achieve the best possible outcomes.
Seein a physiotherapist costs less than what you would pay in terms of compromising your quality of life and being in pain.
Seeing a physiotherapist can help you:
- Get back to your favourite activity or sport
- Recover from an injury or surgery
- Get educated on how to exercise safely, manage painful episodes, improve your posture and more.
- Return to work after an injury
- Rehabilitate after an automobile accident
- Recover after childbirth
- and more.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Understanding the cost of physiotherapy is important for planning your treatment. Triangle Physiotherapy offers high-quality care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our clinics provide transparent pricing and personalized treatment plans to ensure you receive the best care at a cost that works for you.”
Preparing for a marathon requires more than just physical training. It also involves strategic planning and making the right choices to ensure you reach the starting line in peak condition. While proper training and nutrition are crucial, the day before the marathon is equally important for maximizing your performance. In this article, we will explore 10 essential activities to help you make the most of your day before the marathon.
1. Relax and Rest
The day before a marathon, it’s crucial to prioritize rest and relaxation. Engage in activities that promote calmness and allow your body to recover from training. Take a gentle walk, read a book, or indulge in a soothing bath. Remember, a rested body is a prepared body.
2. Focus on Hydration
Hydration is key to maintaining optimal performance during a marathon. Begin increasing your fluid intake the day before the race, but avoid excessive consumption. Sip water, electrolyte-rich drinks, and herbal teas throughout the day. Adequate hydration will help prevent muscle cramps and fatigue.
3. Light Exercise and Stretching
Engage in light exercise and stretching routines to loosen your muscles and improve flexibility. However, avoid intense workouts that could potentially tire you out or cause muscle soreness. Gentle stretches and mobility exercises will help keep your body limber and prevent injuries.
4. Plan Your Nutrition
Proper nutrition plays a vital role in marathon success. Consume a well-balanced meal rich in carbohydrates, lean proteins, and healthy fats. Opt for easily digestible foods such as whole grains, fruits, vegetables, and lean proteins. Avoid experimenting with new foods or overeating, as it may lead to discomfort on race day.
5. Physiotherapy Session
Consider scheduling a physiotherapy session on the day before your marathon. Physiotherapists can assess your body’s condition, identify any muscular imbalances or areas of concern, and provide appropriate treatments. They may use techniques like massage, stretching, or taping to enhance your performance and reduce the risk of injury.
6. Organize Your Gear
Take time to organize all the essential items you’ll need for the race. Lay out your race attire, running shoes, socks, GPS watch, and any other accessories. Double-check that you have everything you’ll need, such as race bibs, safety pins, energy gels, and hydration packs. Being well-prepared will help alleviate stress on race day.
7. Visualize Success
Visualization is a powerful tool to mentally prepare for a marathon. Spend some time visualizing yourself crossing the finish line, feeling strong and accomplished. Envision overcoming challenges and maintaining a steady pace. This mental exercise can boost confidence, reduce anxiety, and enhance your overall performance.
8. Plan Your Race Day Logistics
Familiarize yourself with the race route, including the start and finish locations, aid stations, and potential landmarks. Plan your transportation to the race venue, parking, and any logistical considerations. Knowing the details in advance will help you feel more relaxed and focused on race day.
9. Get Quality Sleep
A good night’s sleep is essential to perform your best. Aim for seven to nine hours of uninterrupted sleep the night before the marathon. Create a sleep-friendly environment by keeping your bedroom cool, dark, and quiet. Establish a pre-sleep routine to signal your body that it’s time to wind down and rest.
10. Stay Positive and Trust Your Training
Finally, stay positive and have faith in your training. Remind yourself of the hard work, dedication, and sacrifices you’ve made to reach this point. Trust in your training program and believe in your abilities. Positive thoughts will help you stay focused, motivated, and perform at your best.
The day before a marathon is a critical time to fine-tune your physical and mental preparations. Prioritize relaxation, hydration, light exercise, and physiotherapy to ensure your body is ready for the race. Plan your nutrition, organize your gear, and visualize success to boost confidence. Adequate rest and quality sleep will leave you refreshed for the marathon day. Embrace positivity, trust your training, and enjoy the incredible journey of completing a marathon. Good luck!
Note: Physiotherapy plays a significant role in optimizing marathon performance by addressing any underlying physical issues, promoting muscle recovery, and enhancing overall well-being.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Preparing for a marathon involves more than just training; it requires careful planning and attention to your physical health. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you prepare for your marathon with personalized advice and injury prevention strategies.”
Our physiotherapy center in Mississauga is located at 4188 Living Arts Drive, Unit 3, Mississauga L5B0H7. The closest intersection is Living Arts Drive and Burnhamthorpe Road, in the Square One Mall area.

My health is very important to me so I would like to choose the best physiotherapy clinic near me. I have heard great things about you. What makes you the best physiotherapy clinic in Mississauga?
Our patients have told us many times that we offer the best physiotherapy service in Mississauga because from the second they step inside our physio clinic in Mississauga until the end of every session, our physiotherapists at our Mississauga clinic provide them with a one-on-one quality service they deserve.
I went to a physiotherapy clinic near me which I was told was the best physiotherapy clinic in Mississauga but I found out the physiotherapist who was treating me was not registered. Are all the physiotherapists at your Mississauga clinic registered?
Yes, all the physiotherapists at our Mississauga clinic are registered. We go through a rigorous vetting process for applicants when we hire our professionals, as we want to provide the best expertise and service to our patients.
I recently moved to Mississauga and am in search of a physiotherapist near me who could provide me with excellent care like my previous physiotherapist. Which physiotherapist in Mississauga would you recommend I see?
Our physiotherapists in Mississauga are all registered, highly qualified and will provide you with quality care that will exceed your expectations. We have all their profiles on our website for your review. You may also call us and we can discuss your condition further so we may recommend the physiotherapist at our physiotherapy centre in Mississauga, who we feel would best fit your condition.
What kind of services do you offer at your physio clinic in Mississauga and what makes you different from all the other clinics that offer physiotherapy services near me?
Our physiotherapy center in Mississauga offers:
- Physiotherapy,
- Pelvic Health,
- Pediatric Pelvic Health,
- Vestibular Rehab,
- Massage therapy,
- Naturopathy,
- Acupuncture, Dry Needling
- Chiropractic services.
The physio clinic near me does not provide direct billing. I would only like to go to a clinic that can do direct billing for me. Does your physiotherapy center do direct billing or do I need to pay upfront for the physiotherapy services?
Yes, our physio clinic in Mississauga offers direct billing to most insurance companies to save you time and provide you with a stress free experience.
I have vertigo and am in search of a Vestibular physiotherapist near me. Do you have a Vestibular physiotherapist in your Mississauga location?
Yes, we have a Vestibular physiotherapist at our Mississauga location. Here at the physiotherapy clinic in Mississauga, our vestibular physiotherapist will conduct a thorough assessment to establish the root of your problem and design a customised program of balance exercises to help resolve your symptoms.
If you have Vertigo (BPPV) this can be treated with a simple head maneuver called the Epley’s maneuver.
Your treatment will include exercises and education about your condition.
Who would benefit from pelvic floor physiotherapy?
Pelvic health physiotherapy is the therapeutic treatment of all disorders affecting the pelvis and pelvic floor. From incontinence to prolapse, pelvic pain, or constipation, there is growing evidence that physiotherapy can alleviate, and in many cases cure these symptoms. Pelvic physiotherapists are experienced in treating men and women.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Finding the closest physiotherapy clinic in Mississauga is essential for convenient access to care. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy Etobicoke, Physiotherapy Oakville, Physiotherapy North York, Physiotherapy Toronto, Physiotherapy Lawrence Park, Physiotherapy Queens Quay, Physiotherapy Erin Mills, Physiotherapy Mississauga, and Liberty Village. Our clinics are strategically located to provide you with the highest quality physiotherapy services close to home.”
At Triangle Physiotherapy, we are committed to creating an inclusive and equitable environment for our employees, clients, and the communities we serve. We believe in upholding and promoting principles of Equality, Diversity, and Inclusion (EDI) as well as safeguarding human rights. This policy outlines our commitment to these values and serves as a guide for all stakeholders associated with our clinic.
1. Equality, Diversity, and Inclusion (EDI)

1.1. Equal Opportunities: We are committed to providing equal opportunities to all employees and clients, irrespective of their race, color, ethnicity, nationality, religion, gender, sexual orientation, age, disability, marital status, or any other protected characteristic.
1.2. Anti-Discrimination: Discrimination, harassment, or victimization of any kind will not be tolerated within our clinic. We actively promote a working environment that is free from any form of discrimination.
1.3. Accessibility: We strive to ensure that our clinic facilities, services, and information are accessible to all individuals, including those with disabilities. Reasonable accommodations will be provided to enable individuals to participate fully and equally in our programs and services.
1.4. Inclusive Culture: We foster an inclusive culture that values and respects individual differences. We encourage open dialogue, collaboration, and mutual respect among our employees, clients, and partners.
1.5. Training and Education: We will provide regular training and educational opportunities to our employees to enhance their understanding of diversity, inclusion, and unconscious bias. This will enable them to create an inclusive environment and deliver culturally competent care to our diverse client base.
2. Human Rights
2.1. Human Rights Compliance: We are committed to upholding and promoting human rights as defined by international conventions and local laws. We will not engage in any activities that violate human rights or support organizations or entities that do not align with our human rights principles.
2.2. Privacy and Confidentiality: We respect and protect the privacy and confidentiality of our clients’ personal information in accordance with applicable privacy laws and regulations.
2.3. Ethical Practices: We adhere to ethical business practices and will not engage in any form of exploitation, forced labor, child labor, or any activity that violates basic human rights.
2.4. Reporting Mechanisms: We encourage employees, clients, and other stakeholders to report any concerns related to equality, diversity, inclusion, or human rights violations. We will establish confidential reporting mechanisms and ensure that appropriate actions are taken to address reported issues.
2.5. Continuous Improvement: We are committed to continuously improving our policies, practices, and procedures to ensure that we remain aligned with evolving societal norms, best practices, and legal requirements related to EDI and human rights.
This policy applies to all employees, contractors, clients, visitors, and anyone associated with Triangle Physiotherapy. Violation of this policy may result in appropriate disciplinary action, up to and including termination of employment or termination of client relationship.
We believe that by actively promoting equality, diversity, inclusion, and human rights, we can create a positive and supportive environment that benefits everyone involved with our clinic.
Triangle Physiotherapy remains committed to reviewing and updating this policy periodically to ensure its relevance and effectiveness.
“At Triangle Physiotherapy, we are committed to Equity, Diversity, and Inclusion (EDI) and uphold human rights in all aspects of our services. We provide expert physiotherapy care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our clinics are dedicated to creating an inclusive environment where everyone is treated with respect and dignity.”
Stretching can be beneficial for relieving lower back pain and improving flexibility and mobility.
What are some of the best stretches for the lower back?

Cat-Cow is one of the best stretches for the low back which gentle flow between two poses that warms the body and brings flexibility to the spine. It stretches the back torso and neck, and softly stimulates and strengthens the abdominal organs.

Knee-to-Chest Stretch: Lie on your back with your knees bent. Slowly bring one knee toward your chest, grasping it with your hands and gently pulling it closer. Hold for 20-30 seconds, then repeat with the other leg.

Child’s Pose is one of the best stretches for the low back and provides a gentle stretch for the back, hips, thighs, and ankles. It can help relieve back pain. Start on your hands and knees, then sit back on your heels while extending your arms forward and lowering your forehead to the ground. This stretch gently stretches the lower back.

Piriformis Stretch: Lie on your back with your knees bent. Cross one ankle over the opposite knee, then gently pull the uncrossed leg towards your chest until you feel a stretch in your buttocks. Hold for 20-30 seconds and switch sides.

Figure 4 Stretch: Lie on the ground or treatment table with your legs extended in front of you. Cross one ankle over the opposite knee, then gently lean forward, keeping your back straight, until you feel a stretch in your buttocks and outer hip. Hold for 20-30 seconds and switch sides.

Pelvic Tilt: Lie on your back with your knees bent and feet flat on the ground. Gently flatten your lower back against the floor by tilting your pelvis upward. Hold for a few seconds, then release. Repeat 10-15 times.

Sphinx Pose: Lie on your stomach and prop yourself up on your forearms, keeping your elbows directly beneath your shoulders. Press your forearms into the ground to lift your upper body, arching your back gently. Hold for 20-30 seconds.

Lie on your back with your knees bent, feet flat on the floor. Lift your hips off the ground, forming a straight line from knees to shoulders.

Bird Dog: While in a crawling position, tighten/brace at your abdominal muscles and then slowly lift a leg and opposite arm upwards. Your hip will move into a hip extension on the way up. Lower leg and arm down and then repeat with the opposite side.

Standing Quadriceps Stretch: Stand tall and hold onto a stable object for balance. Bend one knee, bringing your heel toward your buttocks, then grasp your foot with your hand. Hold for 20-30 seconds and switch legs.
Should I stretch my lower back if it hurts?
Doing regular stretching exercises can help with lower back pain by maintaining your posture, strengthening your back and abdominal muscles, and improving flexibility.
What is the best position to sit in with lower back pain?
The best position to sit in with lower back pain is with a back support such as a rolled-up towel or lumbar roll, at the curve of your back. Keep your hips and knees at a right angle. Use a foot stool if necessary. Your legs must not be crossed and your feet should lie flat on the floor. It is also advisable to stretch and move around as much as possible.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Stretching is a key component in managing lower back pain effectively. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you develop a personalized stretching routine to alleviate pain and improve your mobility.”
Introduction to Cancer Rehab
Cancer rehabilitation physiotherapy is a form of physiotherapy for people who have been diagnosed with cancer or for those who are undergoing cancer treatment. The goal of cancer rehab physiotherapy is to help manage and treat the side effects of cancer treatment.
Our cancer rehab physiotherapist will conduct a thorough assessment of your physical condition and medical history.
What are some conditions that cancer rehab can help with?
Common cancer rehab conditions our registered physiotherapists can help with are:
- Balance problems
- Pain
- Breathing difficulties
- Neuropathy
- Muscle weakness
- Fatigue
- Lymphedema
- Range of motion and mobility issues
- Pelvic health issues
What are some tips to prepare for my cancer rehab appointment?
Some tips for preparing for your cancer rehab physiotherapy appointment are:
- We recommend you drink plenty of water and have a light meal before your appointment.
- Complete the necessary forms before your appointment.
- Remember to bring your doctor’s note to your appointment if your insurance requires one for billing.
- Wear comfortable clothing that allows easy movement.
- Gather any relevant medical information and documentation and bring it to your appointment.
- Make a list of any medications you’re taking.
- Try to get enough rest before the appointment.
How to find a cancer rehab physiotherapy service in Oakville?
Triangle Physiotherapy Oakville is located at 2501 Prince Michael Drive, unit 2 and it’s in the same plaza as Shoppers Drug Mart and Starbucks. The main intersection is Trafalgar and Dundas. There is free parking available
How to find a cancer rehab physiotherapy service in Mississauga?
Triangle Physiotherapy Erin Mills is located at 2520 Eglinton Ave W, Unit 205 across from the Credit Valley Hospital. The main intersection is Eglinton and Erin Mills. Parking is available in the building at $1.00 for 30 minutes.
FAQ
Who can benefit from cancer rehab physiotherapy?
Individuals who have undergone or are currently undergoing cancer treatment can benefit from cancer rehab physiotherapy.
Would cancer rehab physiotherapy help during all stages of cancer treatment?
Cancer rehab physiotherapy can be helpful during all stages of cancer treatment, including before, during, and after treatment.
What kind of treatment is included in a cancer rehab physiotherapy session?
It may include some exercises, modalities, and manual therapy. Your physiotherapist will assess you and create a personalized treatment plan for you.
Is cancer rehab physiotherapy safe?
Yes, cancer rehab physiotherapy is designed to be safe, effective, and beneficial to cancer patients. It has been known to significantly improve the quality of life of Cancer Survivors.
What are the 4 stages of Cancer Rehab?
According to the Dietz Classification of Cancer Rehabilitation, there are 4 Stages in Cancer Rehabilitation.
- Preventative Rehabilitation: Early intervention and exercise to identify potential impairments and prevent or delay complications related to cancer or therapies.
- Restorative Rehabilitation: For cancer patients with the potential to attain full functional recovery, restorative rehabilitation offers comprehensive therapy to regain function to return to work or school.
- Supportive Rehabilitation: For patients with temporary or permanent deficits from cancer and/or treatments, and patients with slowly progressive or chronic cancer, supportive rehabilitation can give the opportunity to re-establish and maintain functional independence.
- Palliative Rehabilitation: For patients with treatment-refractory cancer or advanced disease, less intense palliative rehabilitation may play a role in assisting the patient and their family by maximizing patient comfort and reducing caregiver burden,
Click HERE to book an appointment with a cancer rehab physiotherapist near you.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
The article discusses rehabilitation programs for cancer patients, focusing on improving quality of life during and after treatment. These programs are tailored to address the physical and emotional challenges faced by cancer patients, including pain management, mobility improvement, and emotional support. Triangle Physiotherapy offers specialized services to help patients regain strength and functionality across various locations in the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village.
When choosing a physiotherapy clinic, it’s essential to find a clinic that has physiotherapists that meet your specific needs and can provide high-quality care.
Which is the closest Physiotherapy clinic near me in the Erin Mills area of Mississauga?
Our physiotherapy center at Erin Mills in Mississauga is located in the Arc Condominiums at 2520 Eglinton Avenue, W, on the SECOND Floor. The closest intersection is Erin Mills Parkway & Eglinton Ave W across from Erin Mills Town Center and Credit Valley Hospital.
Is there a highly qualified physiotherapist at your physio clinic in Mississauga who you would recommend I see?
Our physiotherapy center in Mississauga has highly qualified professional physiotherapists with many years of experience. We have physiotherapists with FCAMPT designation, which is the highest certification in manual therapy. Our physiotherapists are also trained in specialties like dry needling, pelvic health and cancer rehab.
We also have a team of highly skilled professionals including physiotherapists, massage therapists, acupuncturists, chiropractic doctors as well as naturopathic doctors. You are welcome to read their profiles on our website or call us for more information.
Do all your physiotherapy centers offer physiotherapy services, massage services, and chiropractic services?
Yes, all of our clinics offer the following services:
- Physiotherapy
- Pelvic Floor Physiotherapy
- Acupuncture and Dry Needling
- Vestibular Rehab Therapy
- Chiropractic
- Massage therapy
- Naturopathic Medicine
Are the fees for all physiotherapy services, massage services and chiropractic services the same in all your physiotherapy centers?
Yes, our fees at all eight locations are the same for all physiotherapy services.
I have tried a physio clinic near me but I wasn’t satisfied with the service they have provided me and I would like to try another physio clinic near me. How many clinics do you have in Mississauga?
We have two locations in Mississauga, Triangle Physiotherapy by Erin Mills Mall and Triangle Physiotherapy by the Square One Shopping Centre.
I have been searching for physiotherapy clinics near me that offer Shockwave physiotherapy service, does your clinic offer this?
Yes, our physiotherapy clinic in Erin Mills has shockwave therapy as well as other Physiotherapy modalities available to provide the best treatment possible for our patients.
I recently found out that the physiotherapy clinic near me has registered physiotherapists at their physiotherapy clinic. I would like to move to a physio clinic near me, are all your physiotherapists in Erin Mills registered?
Yes, all our physiotherapists at the Erin Mills clinic are registered physiotherapists and highly qualified.
I have seen many physiotherapists in Erin Mills but I have yet to see improvement in my condition. Are all your physiotherapists in your Physiotherapy clinic in Mississauga registered and am I able to choose which registered physiotherapist I would like to book with?
All our physiotherapists will take excellent care of you, but you’re more than welcome to choose which physiotherapist you would like to book with. You may check their profiles on our website and inform us who you would like to book with when you request an appointment.
Many Physiotherapy centers claim to be the best physiotherapy clinic in Mississauga but I have personally heard from a friend who I trust that you are indeed the best physiotherapy clinic in Mississauga. How do I book an appointment?
You may call, email, or send us a message on the chat feature on our website, and we will gladly help you book an appointment at a time that is most convenient for you. You may also submit a booking request by clicking here.
What is physiotherapy?

Orthopaedic Physiotherapy is the assessment and treatment of all musculoskeletal conditions (including back and neck pain, fractures, and sprains) caused by repetitive “wear and tear,” sports injuries, falls, car accidents, or surgeries. The problem can be acute or chronic. Manual therapy, education, active exercise therapy, soft tissue release, and joint mobilizations are the focus of treatments at Triangle Physiotherapy in Erin Mills, to allow you to regain strength, flexibility, balance, and full movement and function.
Our physio clinic Erin Mills, Mississauga has qualified and expert physiotherapists to help you with any musculoskeletal, vestibular, or pelvic health issues.
How is physiotherapy beneficial and what conditions can it treat?
Physiotherapists apply their extensive scientific knowledge of anatomy and physiology to:
- Assess, diagnose, and treat injuries & conditions that affect people of all ages and social groups
- Assist a patient to prevent injury in the workplace or on the sports field
- Promote healthier lifestyles for all
By choosing Triangle Physiotherapy in Mississauga you can rest assured that your physiotherapist is a registered professional with the highest qualifications. This means that they have undergone rigorous scientific training and that they continue to stay up to date with current practices.
Physiotherapy can help a wide variety of conditions including the following:
- Sports injuries
- Posture & movement correction
- Low back pain
- Neck pain & Whiplash
- Headaches
- Shoulder pain
- Ankle sprains
- Knee pain
- Shin splints
- Groin & hip injuries
- Muscular corks/contusions/tears
- Osteoarthritic/degenerative joint pain and more.
What are the different types of physiotherapy?
There are different types of specializations in physiotherapy, some of which are listed below:
- Orthopedic Physiotherapy
- Pelvic Floor Physiotherapy
- Vestibular Physiotherapy
- Cancer Rehab Physiotherapy
- Neurological Physiotherapy
- Sports Physiotherapy
- Pediatric Physiotherapy
Who would benefit from pelvic floor physiotherapy?
Pelvic Floor Physiotherapists are specifically trained in diagnosing and treating conditions associated with the pelvic floor muscles. This usually refers to muscles involved in reproductive and digestive processes in the body. While these muscles are in close proximity to muscles commonly involved in lower back problems, and sometimes even overlap, physiotherapy treatment for the lower back involves significantly different techniques.
Men, women, and children with pelvic floor dysfunction can benefit from pelvic floor physiotherapy.
What can I expect from my pelvic floor physiotherapy appointment?
When attending an appointment at our Mississauga Pelvic Health clinic for the first time, you will be asked to fill in a new patient information form prior to your initial visit. We highly recommend filling out your forms at home through our user-friendly patient portal, the link for which will be sent to you as soon as you book your session.
We will endeavor to make your first visit to our clinic a comfortable experience.
At your initial consultation, your physiotherapist will:
- Conduct a thorough examination including history taking and a physical assessment, which may include an internal examination of your pelvic area;
- Give you a working diagnosis of your condition;
- Education
- Treatment Plan
The initial visit will be an hour long and follow-up visits can range from 30 minutes to an hour depending on the amount of time your physiotherapist needs with you.
Who performs acupuncture at your physiotherapy clinic in Mississauga, Erin Mills location?
At Triangle Physiotherapy Erin Mills, acupuncture treatment is carried out by our physiotherapists, who have undergone specialized training. They use acupuncture or dry needling as part of their physiotherapy treatment to reduce pain and stimulate the healing process.
In addition to our physiotherapists, our acupuncturist also has specialized training in needling and can help with conditions such as:
- Pain
- Stress & anxiety
- Sleep & insomnia
- Allergies
- Respiratory issues
- Women’s health
- Dizziness & Vertigo
- Asthma
- Weakness & Fatigue
What conditions can vestibular physiotherapy be beneficial for?
Vestibular rehabilitation is a specialized form of therapy primarily aimed at reducing symptoms of vertigo, dizziness, visual disturbance, and/or imbalance. Research suggests that it is beneficial, safe & effective.
Vestibular rehabilitation can benefit patients of any age and can be effective for long-standing symptoms, although it is advisable to start as soon as possible.
Treatment plans for vestibular conditions depend on the presenting symptoms, medical history, diagnostic test results, and physical examination. Treatment will be goal focused and progressive and you will be provided with exercises to complete independently on a regular basis.
How do I find a pelvic health physiotherapist near me?
We have 8 locations with pelvic health physiotherapists to help you. Book an Appointment today!
- Pelvic Health Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Pelvic Health – Triangle Physiotherapy Oakville
- Pelvic Health Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Pelvic Health – Triangle Physiotherapy Mississauga
- Downtown Pelvic Health – Triangle Physiotherapy King West
- Uptown Toronto Pelvic Health – Triangle Physiotherapy Lawrence Park
- Pelvic Physiotherapy Downtown Toronto – Triangle Physiotherapy Queens Quay
- Mississauga Pelvic Health – Triangle Physiotherapy Erin Mills
“Finding the closest physiotherapy clinic is important for convenient and effective care. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our clinics are easily accessible, providing high-quality physiotherapy to help you achieve your health goals.”
How do I choose the Best Physiotherapist Near Me?

When choosing a physiotherapist, it’s essential to find someone who meets your specific needs and can provide high-quality care. Here are some steps you can take to help you pick the best physiotherapist:
- Ask for recommendations: Ask your friends, family, or colleagues for recommendations. Personal referrals can be valuable as they come from people you trust.
- Research their experience and specialization: Look for a physiotherapist with experience and expertise in treating your specific condition or injury. Physiotherapy covers a broad range of areas, such as sports injuries, post-surgery rehabilitation, back pain, or neurological disorders. Choosing someone who specializes in your area of concern can increase the chances of effective treatment.
- Check credentials and qualifications: Ensure that the physiotherapist you’re considering is licensed and registered to practice in Ontario. You can usually verify their credentials through the College of Physiotherapists of Ontario.
- Read reviews and testimonials: Search online for reviews or testimonials from previous patients. Although individual experiences may vary, reading about others’ experiences can give you an idea of the physiotherapist’s reputation and patient satisfaction.
- Assess communication and rapport: A good physiotherapist should listen and communicate well. They should be able to understand your concerns, explain your condition or treatment plan clearly, and answer any questions you may have. It’s important to feel comfortable and have a good rapport with your physiotherapist to ensure a positive therapeutic relationship.
- Consider practical factors: Take into account the location of the physiotherapy clinic or practice. It’s generally more convenient to choose a clinic that is easily accessible to you, whether it’s close to your home or workplace. Additionally, check their availability and scheduling options to see if they can accommodate your needs.
- Insurance coverage: If you have health insurance, check if the clinic provides direct billing to your insurance. This way you only have to pay a copayment or deductible if required by your plan.
- Initial Assessment: Schedule an initial assessment with the physiotherapist to discuss your condition, treatment options, and their approach. This can give you a sense of their knowledge, professionalism, and whether their treatment philosophy aligns with your goals.
What are the types of specializations that physiotherapists can have?

Physiotherapists have training in assessing, diagnosing, and treating a wide range of physical conditions and injuries. Physiotherapists can specialize in various areas of practice based on their interests, expertise, and advanced training. Some common specializations that our physiotherapists in Toronto have include:
- FCAMPT – The highest level of training in orthopedic manual therapy
- McKenzie Certification
- Cancer Rehab
- Pelvic Health – Assessing and treating pelvic floor conditions in men and women
- Vestibular Rehab & Concussion Therapy
- Running Assessments
- Sports Physiotherapy
These are just a few examples of the specializations within physiotherapy. It’s worth noting that some physiotherapists may have expertise in multiple areas or choose to focus on specific sub-specialties within these broader categories.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Choosing the best physiotherapist near you is crucial for effective treatment and recovery. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team is dedicated to providing personalized care tailored to your needs, helping you achieve your health goals.”
Q: Why do I experience back pain while working from home?
A: Back pain during work from home can be caused by various factors. Some common reasons include:
- Poor posture,
- Inadequate ergonomics,
- Prolonged sitting,
- Lack of physical activity, and
- Stress
Working from home often means using suboptimal workstations, such as sitting on a couch or using a kitchen table as a desk, which can contribute to poor posture and strain on the back muscles.
Q: How can I improve my posture while working from home?
A: Improving your posture can help reduce back pain. Here are some tips:
- Use a comfortable chair with good lumbar support.
- Sit up straight and align your head, neck, and spine.
- Keep your feet flat on the floor or use a footrest if needed.
- Position your computer monitor at eye level to avoid straining your neck.
- Take breaks and stretch regularly to prevent prolonged sitting.
Q: What are some ergonomic recommendations for a home office setup?
A: Consider the following ergonomic recommendations for a home office setup:
- Invest in an adjustable chair with proper lumbar support.
- Use a desk or workstation at an appropriate height to maintain proper alignment.
- Position your keyboard and mouse at a comfortable distance and height.
- Ensure your computer monitor is at eye level and about an arm’s length away.
- Use a document holder if you frequently refer to papers or documents.
- Consider using an ergonomic keyboard and mouse to minimize strain on your hands and wrists.
Q: How can I incorporate physical activity into my work-from-home routine?
A: Adding physical activity to your work-from-home routine can help alleviate back pain. Here are some suggestions:
- Take short breaks every hour to stretch and move around.
- Incorporate exercises such as walking, jogging, or cycling into your daily routine.
- Consider using a standing desk or an adjustable desk converter that allows you to alternate between sitting and standing.
- Engage in exercises specifically targeting core strength and back muscles, like yoga or Pilates.
- Schedule regular exercise breaks or participate in online workout classes during your breaks.
Q: Are there any specific exercises that can help relieve back pain while working from home?
A: Yes, certain exercises can help relieve back pain. Here are a few examples:
- Cat and Camel

Get on your hands and knees, arch your back upward like a cat, then lower it down like a camel.
2. Back Extensions

Lie face down, place your hands under your shoulders, and slowly lift your upper body off the ground while keeping your pelvis on the floor.
3. Bridge Pose

Lie on your back with your knees bent, feet flat on the floor. Lift your hips off the ground, forming a straight line from knees to shoulders.
4. Child’s Pose

Kneel on the floor, then sit back on your heels while lowering your upper body forward, reaching your arms out in front of you.
Remember to consult with a physiotherapist for personalized advice on exercises and stretches for your specific condition.
Q: How can I manage stress-related back pain while working from home?
A: Stress can contribute to back pain. Here are some strategies to manage stress:
- Practice relaxation techniques such as deep breathing exercises, meditation, or mindfulness.
- Maintain a healthy work-life balance by setting clear boundaries between work and personal time.
- Engage in stress-reducing activities outside of work, such as hobbies, exercise, or spending time
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Working from home can lead to back pain, but with the right strategies and physiotherapy, you can find relief. Triangle Physiotherapy offers expert services across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced physiotherapists can help you develop a personalized plan to manage and prevent back pain while working from home.”










