Shoulder Prehabilitation (prehab) involves the process of implementing a physical, psychological, nutritional intervention before an individual goes into surgery. The goal behind prehab programs is to maximize an individual’s physical and psychological fitness/health before surgery in order to reduce pain, increase physical function and allow you to return to your normal activities sooner following surgery.
Although there is limited evidence regarding shoulder prehab programs, there is promising and growing evidence that suggests prehab programs for hip, knee, and spinal surgery may improve pain, function and reduce the total cost of healthcare spending in the post-operative period.
Also Read, Physiotherapy Clinics in Etobicoke

Types of Surgeries for Shoulder
- Reverse arthroplasty
- Total shoulder arthroplasty/replacement
- Rotator cuff repair
- SLAP repair
- Bicep tendon repair
- Tenotomy
What Prehab Programs look like:
Most prehab programs can be anywhere from 2-8 weeks leading up to surgery and could potentially involve:
1) Exercise training (2-3x/week)
- Strengthening and stabilization exercises for the rotator cuff and muscles supporting your shoulder blade
- Home exercise program tailored to your needs
- Exercise training 1 on 1 with a physical therapist
2) Education: information delivered regarding
- Shoulder anatomy and mechanics
- Pain science education
- The process of your operative procedure
- Patient-therapist expectations
- Post-operative protocol
- Detailed exercise program and technique
Also read, Best Physiotherapist near Mississauga
3) Nutritional support
- Consultation with a registered dietician
- Detailed nutrition programs to optimize physical and mental health
- Nutritional supplements as indicated
4) Psychological support
- Consultation with psychologist/ psychotherapist
- Anxiety and stress reduction
- Cognitive-behavioral therapy
- Relaxation techniques
- Coping strategies for surgery
Shoulder Prehab is a set of exercises and movements designed to strengthen and condition the shoulder joint and surrounding muscles, helping to prevent injury or improve recovery from a previous injury. Prehabilitation may include:
- Shoulder rotator cuff strengthening exercises such as internal and external rotation with light weights.
- Scapular stability exercises to improve posture and reduce stress on the shoulder joint.
- Stretching to improve flexibility and range of motion.
- Plyometric exercises to improve power and explosiveness.
- Core stability exercises to improve overall body control and stability.
Prehabilitation should be performed regularly, especially if you have a history of shoulder injuries or plan to participate in overhead activities such as weightlifting or throwing. By taking care of your shoulder before it becomes a problem, you can help prevent injury and improve your performance.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Shoulder prehabilitation is essential for preventing injuries and optimizing recovery, especially for those undergoing surgery or managing shoulder pain. If you’re looking for professional physiotherapy services for shoulder prehabilitation, there are several clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care to help you strengthen your shoulders and maintain overall joint health.
One of the most common runners’ complaints is Shin splints (also known as Medial Tibial Stress Syndrome (MTSS)). The word shin splints describes pain/discomfort that gets worse during running or exercise around the front of the lower shin. Shin splints are usually developed by overuse, and a registered physiotherapist will do a detailed assessment to diagnose shin splints and develop a treatment plan to resolve them.
Shin splints are painful and uncomfortable but here are a few tips to effectively manage them.

Woman suffering from an ankle injury while exercising. Running sport injury concept.
Rest
Shin splints are considered an overuse injury. In the short term, rest will help the pain, and it is advised to rest for a period of time before beginning to run again. Start with shorter, slower distances instead of jumping right back into long distances when you start running again. Start running once a week and work up to twice a week if you usually run 3 days a week.
Also read, Best physsiotherapy clinic in Oakville
Ice
Place ice packs on your shins for a few minutes at a time. Icing will not treat your shin splints but will help effectively manage your pain after running.
Change up your workout routine
Adding resistance training to your workout routine can help reduce your pain by helping your muscles & tendons increase their capacity. Incorporating other types of aerobic exercise into your routine, like cycling, rowing, or the elliptical in place of running, can also help. Shin splints commonly come from the impact from running on hard or uneven surfaces. Replacing running with a different type of exercise once a week can help.
Stretching, warm-ups and cool-downs
Stretch your calves and shins before running to increase the flexibility in your legs. Warm-up before your workout to prepare your muscles and cool down at the end of it to help your muscles recover.
Also read, Best Physiotherapy Clinic in Missisuaga
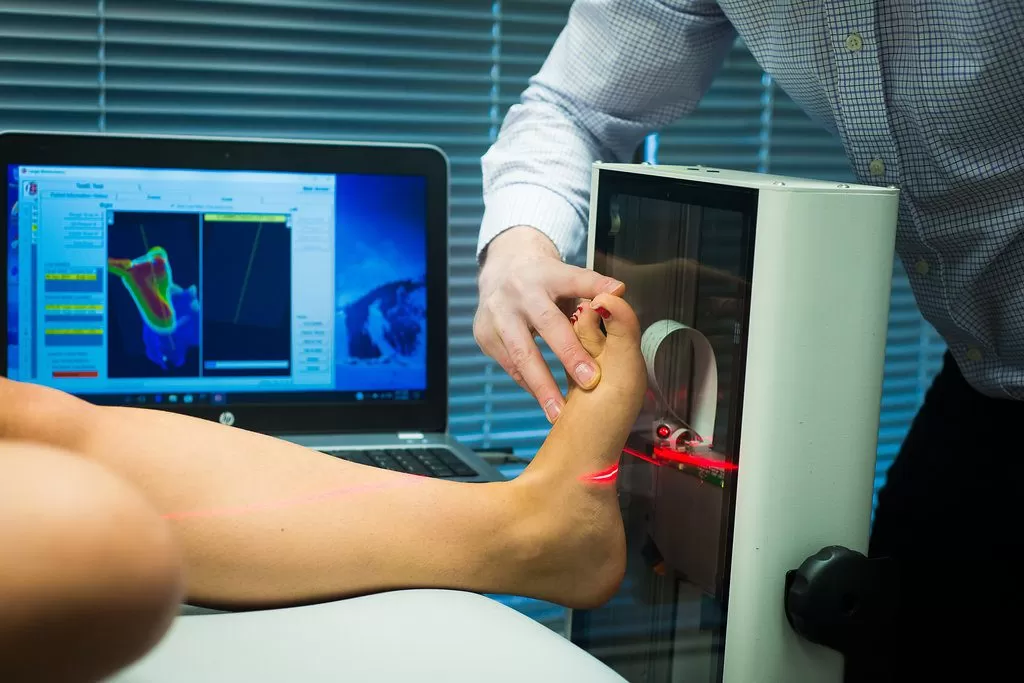
Footwear & Orthotics
Think about how long you have had your running shoes. Good shoes are important as they act as shock absorbers every time your foot hits the ground. If the sole of the shoe is worn, shoes lose their shock absorption. Try a new pair of shoes with more cushioning and see how you get on.
Also, consider seeing a chiropodist for a pair of orthotics. Custom orthotics can help align and stabilize your foot and ankle, taking stress off of your lower leg. They can also be beneficial if you have flat feet.
Our physiotherapists at Triangle Physiotherapy can help resolve your shin splints and get you back to running or any other sport that you may love! Call us to book your assessment or book online here.
If you’re suffering from shin splints, professional physiotherapy can help with pain management and recovery through targeted exercises and treatments. For those in need of physiotherapy services, there are reputable clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care to help you recover from shin splints and get back to your daily activities pain-free.
We’ve all heard how good running can be for you. Running helps to lose weight, prevent disease, lower stress, strengthen joints, manage blood pressure… the list goes on and on. But there’s a suprising problem you may be experiencing if you’re a long distance runner. It’s called leaky gut. I know, it sounds gross, but if you’re a runner then it’s something to keep in mind. How do you know if you have a leaky gut? Read on to find out common symptoms and how to treat it.
What is leaky gut, anyway?
Leaky gut, also known as intestinal permeability, is a dysfunction in the lining of our intestine. Our intestinal walls are only one cell layer thick. Their job is to absorb nutrients and prevent bacteria from getting into our bloodstream. When the cells of the gut lining start to separate and let bacteria enter the bloodstream, we get what we call leaky gut. This can lead to all kinds of health issues, including:
- allergies
- asthma
- autoimmune disease
- eczema
- psoriasis
- rheumatoid arthritis
- food sensitivities
- irritable bowel syndrome
- Crohn’s disease
- ulcerative colitis
- thyroid problems
- acne
- nutrient deficiencies
- depression and other mood disorders
Also read, Physiotherapy Treatment in Mississuaga
How does running lead to leaky gut?
It’s actually not just running that can lead to leaky gut. Powerlifters and people who do cross-fit are at risk, too. Same goes for anyone who does vigorous strength training or heavy exercise. The gut lining becomes more permeable due to the amount of stress put on your body by these types of activity. High physical stress leads to higher metabolic demands. Endurance sports do appear to have the most profound effect on leaky gut though, which is why you might be more concerned if you’re a marathon runner, cyclist, or triathlete.
When you exercise, plant-derived carbohydrates are digested and fermented by the gut. This can create some harmful byproducts that play a role in creating leaks in your gut. Once you have a leaky gut, toxins are more easily able to cross from your intestines into your bloodstream.
Also read, Physiotherapy Treatment in Oakville
Endurance exercise can also increase our secretion of pro-inflammatory cytokines. This means that more inflammation is happening in the gut, which can throw off the balance of good bacteria versus bad bacteria in the intestines.
If you know me, you know I don’t like talking about health issues without some scientific studies to back up what I’m saying. So let’s take a look at one. Researchers looked at LPS (lipopolysaccharide) levels in athletes. They chose to look at LPS because it is a toxin found in bacteria. They measured LPS from blood samples of 29 athletes before, immediately after, one hour after, two hours after, and 16 hours after a triathlon. What they found was that LPS in the blood increased immediately after the race. But guess what? LPS was even higher than that one hour later. This demonstrated that there was an increase in leaky gut both during and after intense exercise.
I think I might have a leaky gut… now what?
Don’t hang up your running shoes just yet, folks. There might be a solution to those leaks in your gut. Remember how I mentioned that the balance between good and bacteria in the gut can get thrown off? Well, one way to help restore that balance is by taking probiotics. Probiotics are known as the good, healthy bacteria that we want and need in our gut. There are many different strains of probiotics. The two that have been shown to be most helpful with leaky gut is called Lactobacillus and Bifidobacterium. These strains help cells of the intestinal wall to tighten up the gaps between them.
A study demonstrated that probiotic supplements reduced LPS levels in the blood. This led to less leaky gut as well as an increase in the amount of time it took to reach fatigue while exercising in hot temperatures. This means that probiotics could actually help to improve athlete performance, too!
If you are a runner and suspect you may have a leaky gut, don’t wait until deteriorating health issues come along. Act now by calling the clinic to book your appointment with Dr. Corina Kibsey, ND today.
Runners often face various issues that can benefit from targeted physiotherapy to prevent injuries and improve performance. If you need professional physiotherapy care, consider visiting clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer specialized services tailored to the needs of runners, helping them stay healthy and achieve their fitness goals.
Winter is on its way out and spring is almost upon us. With the warmer change in weather, we shake off our desire to hibernate and become more active, doing activities we haven’t done in months! However, we sometimes rush into things too quickly and can put too much pressure on our feet, leading to the development of various foot problems. Orthotics might be the answer for you as they can help change the way your foot makes contact with the ground and can take pressure off high-pressure areas in the foot.
What are Orthotics?
Orthotics are insoles that you use inside your shoes that help rectify biomechanical problems of the foot. They are usually made of a combination of rubber, metal, plastic, leather, or any other synthetic material. Our feet have so many muscles, bones, and joints that abnormal biomechanics of how they’re moving can result in numerous foot problems along with pain in your knee, lower back, hip or leg.
Also read, Physiotherapy Clinics in Mississuaga
How can Orthotics correct foot conditions?
- Orthotics help balance pressure placed on the feet by redistributing the weight appropriately
- They help stabilize the heel
- Support the arch of the feet
- Provides cushioning to delicate and inflamed areas of the feet that arise from too much walking, jogging, running, etc.
There are generally two options when it comes to selecting orthotics: over-the-counter orthotics and custom-made orthotics. Over-the-counter orthotics are available at your local pharmacy and big box store and they can be used with your regular shoes to correct trivial problems. However, because they are prefab, generalized products, there is a possibility that they might make your foot pain worse due to it not being the right kind of support that you need. Custom made orthotics work best because they are tailor-made to correct the problems specific to your feet. Check out our earlier blog on the most popular kinds of Orthotics for further detail.
Also read, Physiotherapy Clinic in Oakville
Here’s a tip
Orthotics can still benefit you even if you don’t suffer from any foot issues but are an active participant in sports. If your foot is dealing with stress and impact, or if you have recently gained weight, orthotics will help you walk better!
Put your best foot forward and in the right direction!
We at Triangle Physiotherapy will quite literally help you get back on your feet! Our Chiropodist can advise you on how to look after your feet and what type of shoes or orthotics to opt for. Book an appointment with our Chiropodist today at any of our 6 clinics located across the GTA: Etobicoke, Oakville, Mississauga, North York, Toronto (King Street West) and Yonge Street. If you have any questions regarding any kind of foot conditions, please call or email us and we will be happy to help you!
Orthotics can be highly effective in managing various foot-related conditions, providing support and alignment to improve comfort and mobility. If you are looking for physiotherapy services to complement your orthotic treatment, there are clinics available in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and customized treatment plans to address your foot health needs.
Our feet are likely the most used body parts of all of our limbs. Be it sitting or standing, we are always using our legs in one way or the other. In fact, the use of our feet and legs usually begins the moment we wake up. So it is safe to say that our feet play a vital role in our day-to-day life and as such, it is important to take good care of them. Our feet carry the entire weight of our body throughout the day. They undergo tremendous pressure with every step we take as they get compressed and endure repeated movement against our footwear. Over a period of time, pressure on certain parts of the foot can increase and the body compensates by adding extra layers of scar tissue and skin on parts of feet that undergo high pressure, such as the ball and heel & toes of the foot. This can cause there to be painful areas of pressure on the foot or the formation of callouses on areas of higher pressure on the foot.

Also read, Best Physiotherapy Clinic in Etobicoke
Why schedule an appointment with a Chiropodist?
Walking, running, sitting – everything involves your legs. A minor injury or pain can cause huge discomfort in your everyday life and can escalate to become a serious issue. For example, an ingrown toenail or an infection can be very painful and uncomfortable. Seeing a Chiropodist at an earlier stage will help immensely in preventing and managing these kinds of foot-related problems.
An appointment with a Chiropodist will involve a thorough assessment of your foot-related problem and treatment that will help alleviate the problem. Even without a significant ongoing foot issue, a visit to the Chiropodist can help you in preventing one from developing by gaining more insight into your walking pattern or providing education on correct foot care. They are trained to diagnose and treat a wide variety of foot-related conditions and are able to understand their patient’s needs in order to prevent and treat both acute and chronic conditions that involve the foot and lower limb functions.
Also read, Best Physiotherapy Clinic in Oakville
What do we treat at Triangle Physiotherapy?
Our Chiropodist is a highly skilled professional that is an expert in their field. At Triangle Physiotherapy, our registered Chiropodists diagnose, assess, and treat a wide range of foot-related health issues and abnormalities including but not limited to:
- Alignment and support to prevent or correct abnormalities in the lower limbs
- Abnormal gait patterns
- Foot pain
- Sports injuries
- Diabetic foot care
Also read, Best Physiotherapy Treatment in Mississauga
How to Contact Triangle Physiotherapy?
We have 8 clinics located across the GTA: Etobicoke, Oakville, Mississauga, North York, and Toronto (King Street West, Queens Quay, and Yonge Street. If you have any questions regarding what type of chiropody treatment may be appropriate for you, please call or email us and we will be happy to answer your questions. You can also Book an Appointment with a Chiropodist now.
Chiropodists play a vital role in managing foot and lower limb conditions, often collaborating with physiotherapists to provide comprehensive care. If you’re looking for professional physiotherapy services to complement chiropody care, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and personalized treatment plans to help you achieve optimal foot health.
Who is a Podiatrist? A podiatrist deals with the assessment, diagnosis and treatment of the lower limbs and feet. What is a Chiropodist? A chiropodist deals with the assessment, diagnosis and treatment of the lower limbs and feet. Sound familiar? That is because these two professions are one and the same!
While there may be differences in terms of scope of practice in other areas of the world, in Canada, both podiatrists and chiropodists are qualified to treat patients with arthritis, diabetes, lower limb sports injuries, and various other ailments of the feet. They have received specialized training which allows them to work with patients of all ages and to help the elderly stay mobile and independent. The only practical difference between the two professions, in terms of their scope of practice in Canada, is simply their title.
Also read, Physiotherapy Treatment Etobicoke
Chiropodists can advise patients on how to look after their feet and what type of shoes or orthotics to wear. They can also treat, alleviate and benefit day-to-day foot conditions, such as:
- Thickened, fungal, or ingrown toenails
- Varicose veins
- Athlete’s foot
- Smelly feet
- Dry and cracked heels
- Flat feet
- Bunions
- Heel pain
- Ageing feet
- Blisters
- Gout
- Sports Injuries
Also read, Oakville Physiotherapy Rehab Clinic

Seek help from a Chiropodist for advice or treatment if you have:
- Painful heels or arches
- Thickened or discoloured toenails
- Cracks, cuts, or hardened skin on your feet
- Growths, such as warts
- Scaling or peeling on the soles
- Any other foot condition
Don’t bury your head in the sand and ignore small foot problems! These small “problems” can quickly transform into major issues that can affect the quality of your life. As they say, “Prevention is the best cure“. Patients who make regular check-up appointments can avoid many potential foot problems as Chiropodists are specialists at recognizing problems before they have occurred.
Don’t let your feet problems keep you from stepping into our clinic! Seek the help of our foot specialists at any of our locations in Etobicoke, Oakville, North York, Mississauga & Toronto, and say goodbye to your foot dilemmas!
Addressing foot problems effectively often requires a comprehensive approach that includes professional physiotherapy. If you need expert care for foot-related issues, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide specialized physiotherapy services and personalized treatment plans to help you get back on your feet and improve your overall mobility.
What exactly are shin splints? Are they treatable?
Shin splints are a condition characterized by damage and inflammation of the connective tissue joining muscles to the inner shin bone (tibia). Shin splints are known by many different names such as: Medial Tibial Tenoperiostitus, MTSS, Medial Tibial Stress Syndrome, Tenoperiostitus of the Shin, Inflammatory Shin Pain, Traction Periostitis, and Posterior Shin Splint Syndrome.
Several muscles lie at the back of the lower leg, and are collectively known as the calf muscles. The tibialis posterior, flexor digitorum longus, flexor hallicus, and soleus are muscles that lie deep within the calf and attach to the inner border of the tibia. Connective tissues are responsible for attaching these muscles to the tibia known as the tenoperiosteum. Every time the calf contracts, it pulls on the tenoperiosteum. When the tension becomes forced too much or is repeated frequently, the damage is caused to the tenoperiosteum. The results are inflammation and pain. Shin splints can also occur in combination with other pathologies that cause shin pain such as compartment syndrome and tibial stress fractures.
Patients who suffer from shin splints experience pain along the inner border of the shin. In other cases, the patient may experience an ache or stiffness along the inner aspect of the shin that increases with rest (typically and night or first thing in the morning). Areas of muscle tightness, thickening, or lumps may also be felt in the same area of pain.

There are several factors that predispose patients to shin splints:
• Excessive training or exercise
• Poor foot posture (especially in patients with flat feet)
• Inappropriate footwear
• Inadequate warm-up• Training on hard or inappropriate surfaces
• Muscle weakness (especially in calve muscles)
• Tightness in specific joints (such as ankle)
• Tightness in specific muscles (calves especially)
• Poor lower limb biomechanics
• Poor training techniques or methods
• Leg length differences
• Poor balance
• Being overweight
• Deconditioning
• Poor core stability
Also read, Physiotherapy Clinic in Oakville
Physiotherapy treatment for patients with shin splints is vital to speed up the healing process. Physiotherapy will ensure the most optimal outcome and reduce the likelihood of recurrence. Treatment may comprise of the following:
- Deep tissue massage
- Joint mobilization
- Dry needling
- Electrotherapy
- PNF stretches
- Arch support taping
- The use of orthotics or shock-absorbing insoles
- Crutches
- Biomechanical correction
- Ice or heat treatment
- Exercises to improve flexibility, balance, strength, and core stability
- Activity modification advice
- Anti-inflammatory advice
- Footwear advice
- Weight loss advice where appropriate
Also read, Physiotherapy Clinic in Mississauga
If you happen to suffer from shin splints and you are looking for a way to relieve pain, stress, and improve overall health, try adding physical therapy to a routine wellness plan. Our physiotherapists at Triangle Physiotherapy can be a powerful ally when combating daily stress, muscle pain, and general health issues when it comes to shin splints. Not only does physical therapy relieve pain, increase energy levels, and improve overall physical and mental performance, it prevents further injuries.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy can play a crucial role in treating and preventing shin splints by addressing muscle imbalances and improving biomechanics. If you’re looking for professional physiotherapy services to help manage shin splints, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and tailored treatment plans to support your recovery and enhance your running or athletic performance.
Do your legs tingle, become numb, or feel weak? You may be experiencing Sciatica. The term Sciatica describes leg pain that originates from the lower back and travels through the buttock and down the large sciatic nerve in the back of each leg. Sciatica is not a medical diagnosis in and of itself –it is a symptom of an underlying medical condition. Common lower back problems such as: lumbar herniated disc, degenerative disc disease, and spondylolisthesis can cause sciatica symptoms.
Sciatica is often characterized by one or more of the following symptoms:
• Constant pain in only one side of the buttock or leg (rarely in both legs)
• Pain that becomes worse when sitting
• Leg pain that is described as burning, tingling, or searing
• Weakness, numbness, or difficulty moving the leg, foot, and/or toes
• A sharp pain that may make it difficult to stand up or walk
• Pain that radiates down the leg and possibly into the foot and toes
Physiotherapy exercises incorporating a combination of strengthening, stretching, and aerobic conditioning are a central component of almost any sciatica treatment plan.
• Strengthening exercises- Most of these back exercises focus not only on the lower back, but also the abdominal muscles, and the buttock and hip muscles.
• Stretching exercises- Stretches for sciatica are designed to target muscles that cause pain when they are tight and inflexible.
• Low-impact aerobic exercise- Some form of low-impact cardiovascular exercise such as: walking, swimming, or pool therapy is usually a component of recovery, as aerobic activity encourages the exchange of fluids and nutrients to help create a better healing environment.
Also read, Physiotherapy Clinic Etobicoke
When patients engage in a regular program of gentle exercises, they can recover more quickly from sciatica pain and are less likely to have future episodes of pain. As sciatica is due to pressure on the sciatic nerve, it stands to reason that treatment involves removing this pressure. Your physiotherapy treatment aims to achieve this by reducing nerve pressure caused by poorly moving spinal joints as well as easing muscular tension in the lower spine, buttock, and leg.
If you are suffering from sciatica please do not delay. You can achieve the best results when you address the symptoms early!
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Dealing with numbness can be challenging, but physiotherapy can help by improving circulation, reducing nerve compression, and enhancing mobility. For those seeking professional physiotherapy services to address numbness or related conditions, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and personalized treatment plans to help you regain sensation and improve your quality of life.
Patellar tendinopathy aka, Jumpers Knee, (also known as patellar tendonitis, and tendonitis) is an overuse injury affecting the knee. The patella tendon is a short but very wide tendon that runs from the patella (kneecap) to the top of the tibia. It works with the muscles at the front of the thigh to extend the knee so it can perform physical acts like kicking, running, and jumping. Due to these elements, the patellar tendon has to absorb a lot of this loading and as a result, is prone to injury in runners and jumpers. Unlike many running injuries, patellar tendonitis is somewhat more common in men than in women.
The stress on the patellar tendon results in small tears, which the body attempts to repair, but as the injury multiplies, it causes pain from inflammation and weakening of the tendon. When this tendon damage persists for more than a few weeks, it is called, “tendinopathy”.

Initial symptoms of patellar tendonitis can be:
- Anterior knee pain over the patella tendon
- Pain increased from jumping, landing or running activity, and on occasion prolonged sitting
- Onset of pain can be gradual and commonly relates to an increase in sports activities
- Localised tenderness over the patella tendon
- The tendon feeling stiff, mostly first thing in the morning
- The affected tendon may appear thickened in comparison to the unaffected side
Also read, Physiotherapy Clinic in Oakville
Typically, tendon injuries occur in three areas:
- Musculotendinous junction (where the tendon joins the muscle)
- Mid-tendon (non-insertional tendinopathy)
- Tendon insertion (eg. Into the bone)
If you try to work through your pain, ignoring your body’s warning signs, you could cause increasingly larger tears in the patellar tendon.
Knee pain and reduced function can persist if the problem is not addressed , which can progress to more serious patellar tendinopathy.
Treatment of Jumpers Knee
Treatment of this condition has two objectives: to reduce inflammation and to allow the tendon to heal. Rest is a must when the knee is painful and swollen. Avoid stair climbing and jumping sports. Keep your knee straight while sitting, and avoid squatting.
Icing the knee for twenty minutes two to three times a day is recommended, especially after any sporting activities. Exercises can also be used to stretch and balance the thigh muscles.
It is advisable, however, to contact a physical therapist & approach proper physical therapy before you attempt any of these remedies, to avoid any further damage.
Happy Healing!
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Jumper’s knee can be a persistent issue for athletes, but physiotherapy can help by strengthening the knee, improving flexibility, and reducing pain. If you’re looking for professional physiotherapy services to treat jumper’s knee, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and customized treatment plans to help you recover and return to your sport stronger than ever.
A knee sprain is an injury of the ligaments; tough bands of fibrous tissue that connect the bones of the upper and lower leg at the knee joint. One of the main forms of knee sprain is in the anterior cruciate ligament (ACL). The ACL and the posterior cruciate ligament (PCL) bridge the inside of the knee joint, forming an, “X” pattern that stabilizes the knee against front-to-back and back-to-front forces.
There are certain movements in the knee that cause a sprain in the ACL such as:
- a sudden stop;
- a twist,
- pivot, or change in direction at the joint;
- extreme over-straightening (hyperextension);
- or a direct impact to the outside of the knee or lower leg.
These injuries are quite common among athletes in sports such as football, basketball, soccer, rugby, wrestling, gymnastics, and skiing.

It is suggested that when one knee ligament suffers a sprain, there is a good chance that the other parts of the knee may also be injured, most commonly the ACL. Knee sprains are very common. ACL sprains tend to cause more significant symptoms compared to MCL injuries.
The most frequent signs of an ACL sprain are:
- A pop heard or felt inside your knee at the time of injury
- Significant knee swelling within a few hours after injury
- Severe knee pain that prevents you from continued participation in your sport
- Black-and-blue discoloration around the knee
- Knee instability- the feeling that your knee will buckle or give out
Treatment of an ACL Sprain
A physiotherapist will examine both knees, comparing the injured knee to the uninjured one. During this exam, the physiotherapist will check your injured knee for signs of swelling, deformity, tenderness, fluid inside the knee joint, and discoloration. If the patient does not have too much pain and swelling, a physiotherapist will then evaluate the knee’s range of motion and will pull against the ligaments to check their strength. During the exam, the patient will have to bend their knee and the physiotherapist will gently pull forward or push backward on their lower leg where it meets the knee.
Based on the results of the patient’s exam, diagnostic tests may need to be performed to further evaluate the condition of the patient’s knee. These tests may include standard X-rays to check for ligament separation from bone or fracture. Tests may also include an MRI scan or a camera–guided knee surgery (arthroscopy). The expected duration of recovery depends on the severity of the patient’s knee sprain, their rehabilitation program, and what type of sports the patients play. In general, milder sprains heal within 2-4 weeks, whereas other types may take 4-12 months.
There are many ways of preventing ACL knee sprain, to help sports related injuries you can:
- Warm up and stretch before participating in athletic activities
- Do exercises that strengthen the leg muscles around the knee, especially the quadriceps.
- Avoid sudden increases in the intensity of a training program. Do not push too hard or too fast. Gradually increase intensity.
- Wear comfortable, supportive shoes that fit your feet and fit your sport
About 90% of people with ACL injuries can expect a full recovery after proper treatment and a good physical therapy program. As a long-term complication, some patients who suffered from an ACL sprain eventually develop pain from osteoarthritis in the joint where the knee has been injured. This symptom may not become present until 15 to 20 years after the initial knee injury.
Call a professional when:
- Knee becomes very painful or swollen
- Cannot bear weight
- Feels as if it will buckle or give out.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Recovering from an ACL sprain involves targeted physiotherapy to restore knee stability, strength, and mobility. If you need professional physiotherapy services for ACL rehabilitation, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide expert care and customized treatment plans to help you recover fully and return to your active lifestyle.