Who is a Podiatrist? A podiatrist deals with the assessment, diagnosis and treatment of the lower limbs and feet. What is a Chiropodist? A chiropodist deals with the assessment, diagnosis and treatment of the lower limbs and feet. Sound familiar? That is because these two professions are one and the same!
While there may be differences in terms of scope of practice in other areas of the world, in Canada, both podiatrists and chiropodists are qualified to treat patients with arthritis, diabetes, lower limb sports injuries, and various other ailments of the feet. They have received specialized training which allows them to work with patients of all ages and to help the elderly stay mobile and independent. The only practical difference between the two professions, in terms of their scope of practice in Canada, is simply their title.
Also read, Physiotherapy Treatment Etobicoke
Chiropodists can advise patients on how to look after their feet and what type of shoes or orthotics to wear. They can also treat, alleviate and benefit day-to-day foot conditions, such as:
- Thickened, fungal, or ingrown toenails
- Varicose veins
- Athlete’s foot
- Smelly feet
- Dry and cracked heels
- Flat feet
- Bunions
- Heel pain
- Ageing feet
- Blisters
- Gout
- Sports Injuries
Also read, Oakville Physiotherapy Rehab Clinic

Seek help from a Chiropodist for advice or treatment if you have:
- Painful heels or arches
- Thickened or discoloured toenails
- Cracks, cuts, or hardened skin on your feet
- Growths, such as warts
- Scaling or peeling on the soles
- Any other foot condition
Don’t bury your head in the sand and ignore small foot problems! These small “problems” can quickly transform into major issues that can affect the quality of your life. As they say, “Prevention is the best cure“. Patients who make regular check-up appointments can avoid many potential foot problems as Chiropodists are specialists at recognizing problems before they have occurred.
Don’t let your feet problems keep you from stepping into our clinic! Seek the help of our foot specialists at any of our locations in Etobicoke, Oakville, North York, Mississauga & Toronto, and say goodbye to your foot dilemmas!
Addressing foot problems effectively often requires a comprehensive approach that includes professional physiotherapy. If you need expert care for foot-related issues, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide specialized physiotherapy services and personalized treatment plans to help you get back on your feet and improve your overall mobility.
Are your worries all perched on a pillow? And we don’t mean figuratively, but literally, are your worries all about THE PILLOW? Well, you are not in as uncommon a dilemma as you may think. Physiotherapists frequently get queries about pillow-related problems.
Sleeping on the wrong pillow, or one that is too worn out, not only leads to headaches, backaches, and neck cramps but also prevents you from getting a good night’s sleep. Lack of proper sleep can lead to many serious health issues, like obesity, heart disease, diabetes, etc.
It is imperative that you choose the right pillow for yourself but the kind of pillow you should pick will depend on your own unique needs as well. A physiotherapist is the best person to tell you exactly what you need. However, here are a few things that you can keep in mind while making a choice –
- Your usual sleeping position
- The shape and size of your head, neck and back
- Desired softness/firmness of the pillow
- Any neck pain, or backache you may have
- And your budget

Also read, Physiotherapy Clinic in Mississauga
There are a plethora of pillows in the market – cotton, polyester, feather, down, memory foam etc. However, these don’t cater to specific support or pain needs. If you have been injured, or have a particular condition, you will need a pillow that caters best to not just your problem, but also the stage that you are in. There are three main stages –
- Accommodation
- Correction
- Maintenance
For each of these three stages, you will need a specific kind of pillow.
Accommodation Stage:
Specialty pillows that are designed for the ‘Accommodation’ stage, are pillows that bring in comfort and ease by providing support and stabilizing the existing ailment or disorder. Such pillows are often called Displacement pillows and are often recommended by physiotherapists for short-term pain relief after an injury.
Correction Stage:
The next stage of an issue or injury is ‘Correction’. At this stage, a doctor or physiotherapist attempts to find a remedy for the cause of the problem, and thereby correct it. Pillows recommended in this stage are often designed to provide support, and sometimes to even change the sleeping position of the injured or ailing person. There are various ‘Supportive’ pillows to meet different support levels, firmness and neck lobe size needs of different patients. There are also specialized ‘Corrective’ pillows, which can reduce headaches, neck pain, joint pain, and whiplash discomfort and can even improve nerve function. A physiotherapist can tell you what is the ideal Supportive or Corrective pillow you need, based on your health and body needs.
Also read, Physiotherapy Clinic Oakville
Maintenance Stage:
Pillows for the last stage, ‘Maintenance’, help to promote good health by returning and keeping the body in its natural alignment. At this stage maintaining the normal curvature of the neck and spine is of utmost importance. While the normal curvature of one person’s neck and spine may differ from another, there are some general guidelines that a physiotherapist can jot down to help you understand your needs better. Comfort and support are the most important of these.
There are also Aqua pillows, which perform all the 3 functions of a pillow:
- Accommodation: Since water is fluid, a person gets customized accommodation that happens in real time, as the individual changes their position on the pillow.
- Correction: The volume of water determines the firmness and density of the pillow, which means different amounts of water can be utilized to help correct the neck position of different people in different stages of healing.
- Maintenance: Since the volume of water remains constant until changed manually, it helps maintain the neck posture at all times while sleeping.
A lot of people buy a pillow, try it for a few nights, and then feel it isn’t right for them. Sometimes the pillows can be returned, but more often, people end up having a collection of pillows that they have hardly ever used. An Aqua pillow is a huge savior in this aspect, as it can be customized for each individual! The water levels can be modified to best suit the clinical condition, neck shape, and size, and preferred sleeping position of the buyer.
There are also specially designed Orthopaedic pillows for specific conditions like arthritis, fractures, and slip discs. A physiotherapist can enlighten you more about these.
Seek the help of our professionals at any of our locations in Etobicoke, Oakville, North York, Mississauga & Downtown Toronto, and say goodbye to your pillow problems!
Proper posture and support are essential for preventing discomfort and maintaining spinal health. For those seeking professional physiotherapy services to address posture-related issues, consider visiting clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and tailored treatment plans to help you improve your posture and overall well-being.
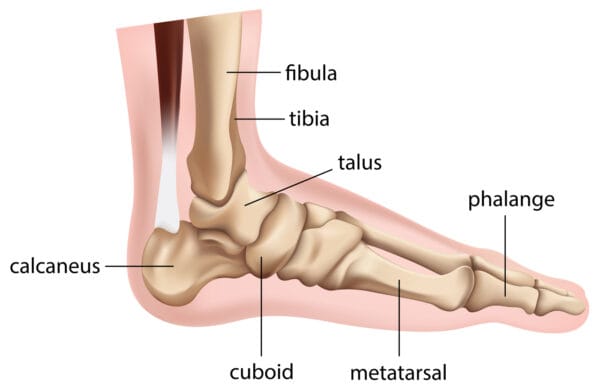
What are orthotics?
Orthotics are custom-made inserts that are worn inside your shoe to control abnormal foot function.
Orthotics solve a number of biomechanically related problems, for example, ankle and knee pain, pelvis, hip, and spinal pain. This is achieved by preventing misalignment of the foot, which significantly alters the way in which the bones move within their joints.
Also read, Physiotherapy Rehab Clinic in Mississauga
How are custom orthotics made?
The process starts with the chiropodist, chiropractor, or physiotherapist conducting a Biomechanical Gait analysis on a tablet that records your gait pattern & explaining the results to you. The chiropodist, chiropractor, or physiotherapist may also take a 3D cast of your feet in a foam box.
The orthotics are then custom-manufactured in the lab based on your foot impressions & scan.
Once the orthotics are made & delivered to the clinic, the chiropodist, chiropractor or physiotherapist will have you come in for a fitting & explain to you the wear & care of the orthotics.
Also read, Physiotherapy Clinic in Etobicoke
Why choose Triangle Physiotherapy for your custom orthotics?
- State-of-the-art technology
- Experienced chiropodists, chiropractors or physiotherapists trained in Biomechanical Assessments & Orthotic Prescription
- Lifetime warranty on the orthotics*
- Assistance with sending your claims to your insurance.
Click HERE to book an appointment with a chiropodist at one of our eight locations.
- Orthotics Etobicoke – Triangle Physiotherapy Etobicoke
- Orthotics Oakville – Triangle Physiotherapy Oakville
- Orthotics North York – Triangle Physiotherapy North York
- Orthotics Mississauga – Triangle Physiotherapy Mississauga
- Orthotics Downtown Toronto – Triangle Physiotherapy King West
- Orthotics Yonge and Eglinton – Triangle Physiotherapy Lawrence Park
- Orthotics Toronto – Triangle Physiotherapy Queens Quay
- Orthotics Mississauga – Triangle Physiotherapy Erin Mills
Orthotics are essential for providing support, alignment, and pain relief for various foot and lower limb conditions. If you are looking for professional physiotherapy services to complement your orthotic treatment, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer specialized care and personalized treatment plans to help you achieve optimal foot health and mobility.
Pacifying the Pain – All about Patella Tendon Tears
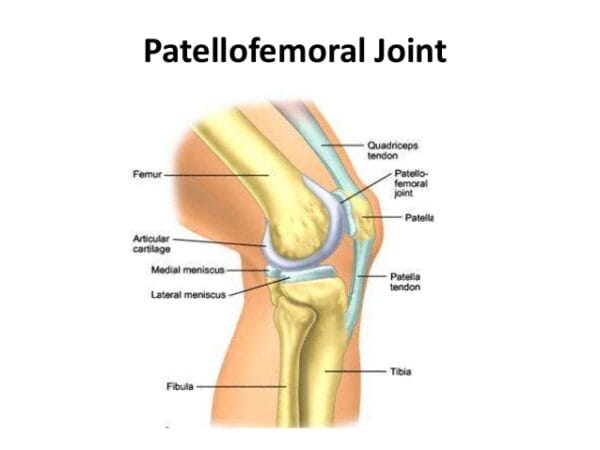
Despite it being named a “Tendon”, the patella tendon is both a ligament and a tendon. It connects to two different bones, the patella and the tibia. The patella tendon works in unison with the quadricep muscles and quadriceps tendons allowing them to straighten the knee. The tear within the patella tendon is either partial or complete and can be a disabling injury:
- Partial tear- More frayed and not complete, (think of a rope that is not completely torn)
- Complete Tear- The tissue is torn into two complete pieces
There are numerous causes that can contribute to the tear of a patella tendon:
- Falls
- Jumping
- Patellar tendonitis- inflammation of the patellar tendon thus weakening the tendon, causing small tears.
- Chronic disease – Chronic renal failure, rheumatoid arthritis, Diabetes mellitus & metabolic disease, etc.
- Infection
- Surgery
Also read, Best Physiotherapy Clinic Mississauga
Most patients have stated that they had felt a popping or tearing sensation when the patella tendon has torn. Additional symptoms recorded were:
- Indentation at the spot where the patella tendon is located
- Bruising
- Tenderness
- Cramping
- Shift of the kneecap to thigh, due to un-attachment
- Difficulty walking due to weakness in the knee
Also read, Physiotherapy Oakville
Once the initial pain and swelling has subsided, physiotherapy treatments can be started. Physiotherapy can restore strength and range of motion. Depending on the intensity of the injury, a brace may need to be worn. While the brace is worn, straight leg exercises are often prescribed to strengthen the quadriceps muscles. As the patellar tendon heals, eventually the brace may be removed, allowing the patient to move freely with a greater range of motion, with more exercises being put into use as healing progresses.
Recovery from patellar tendon tears is possible, and most individuals are able to return to work and regular activities. Even though patients may feel stiffness in the region after recovery, most regain nearly equal motion compared to the uninjured leg. At Triangle Physiotherapy, we are able to dispense custom-fit braces to aid in the recovery of patellar tendon tears. For more information visit our custom braces page at: https://www.trianglephysiotherapy.com/services/custom-bracing
Recovering from a patella tendon tear requires a comprehensive approach, including effective physiotherapy to restore strength and mobility. If you’re seeking professional physiotherapy services for tendon injuries, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and customized treatment plans to help you recover fully and get back to your active lifestyle.
Do your legs tingle, become numb, or feel weak? You may be experiencing Sciatica. The term Sciatica describes leg pain that originates from the lower back and travels through the buttock and down the large sciatic nerve in the back of each leg. Sciatica is not a medical diagnosis in and of itself –it is a symptom of an underlying medical condition. Common lower back problems such as: lumbar herniated disc, degenerative disc disease, and spondylolisthesis can cause sciatica symptoms.
Sciatica is often characterized by one or more of the following symptoms:
• Constant pain in only one side of the buttock or leg (rarely in both legs)
• Pain that becomes worse when sitting
• Leg pain that is described as burning, tingling, or searing
• Weakness, numbness, or difficulty moving the leg, foot, and/or toes
• A sharp pain that may make it difficult to stand up or walk
• Pain that radiates down the leg and possibly into the foot and toes
Physiotherapy exercises incorporating a combination of strengthening, stretching, and aerobic conditioning are a central component of almost any sciatica treatment plan.
• Strengthening exercises- Most of these back exercises focus not only on the lower back, but also the abdominal muscles, and the buttock and hip muscles.
• Stretching exercises- Stretches for sciatica are designed to target muscles that cause pain when they are tight and inflexible.
• Low-impact aerobic exercise- Some form of low-impact cardiovascular exercise such as: walking, swimming, or pool therapy is usually a component of recovery, as aerobic activity encourages the exchange of fluids and nutrients to help create a better healing environment.
Also read, Physiotherapy Clinic Etobicoke
When patients engage in a regular program of gentle exercises, they can recover more quickly from sciatica pain and are less likely to have future episodes of pain. As sciatica is due to pressure on the sciatic nerve, it stands to reason that treatment involves removing this pressure. Your physiotherapy treatment aims to achieve this by reducing nerve pressure caused by poorly moving spinal joints as well as easing muscular tension in the lower spine, buttock, and leg.
If you are suffering from sciatica please do not delay. You can achieve the best results when you address the symptoms early!
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Dealing with numbness can be challenging, but physiotherapy can help by improving circulation, reducing nerve compression, and enhancing mobility. For those seeking professional physiotherapy services to address numbness or related conditions, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and personalized treatment plans to help you regain sensation and improve your quality of life.
Patellar tendinopathy aka, Jumpers Knee, (also known as patellar tendonitis, and tendonitis) is an overuse injury affecting the knee. The patella tendon is a short but very wide tendon that runs from the patella (kneecap) to the top of the tibia. It works with the muscles at the front of the thigh to extend the knee so it can perform physical acts like kicking, running, and jumping. Due to these elements, the patellar tendon has to absorb a lot of this loading and as a result, is prone to injury in runners and jumpers. Unlike many running injuries, patellar tendonitis is somewhat more common in men than in women.
The stress on the patellar tendon results in small tears, which the body attempts to repair, but as the injury multiplies, it causes pain from inflammation and weakening of the tendon. When this tendon damage persists for more than a few weeks, it is called, “tendinopathy”.

Initial symptoms of patellar tendonitis can be:
- Anterior knee pain over the patella tendon
- Pain increased from jumping, landing or running activity, and on occasion prolonged sitting
- Onset of pain can be gradual and commonly relates to an increase in sports activities
- Localised tenderness over the patella tendon
- The tendon feeling stiff, mostly first thing in the morning
- The affected tendon may appear thickened in comparison to the unaffected side
Also read, Physiotherapy Clinic in Oakville
Typically, tendon injuries occur in three areas:
- Musculotendinous junction (where the tendon joins the muscle)
- Mid-tendon (non-insertional tendinopathy)
- Tendon insertion (eg. Into the bone)
If you try to work through your pain, ignoring your body’s warning signs, you could cause increasingly larger tears in the patellar tendon.
Knee pain and reduced function can persist if the problem is not addressed , which can progress to more serious patellar tendinopathy.
Treatment of Jumpers Knee
Treatment of this condition has two objectives: to reduce inflammation and to allow the tendon to heal. Rest is a must when the knee is painful and swollen. Avoid stair climbing and jumping sports. Keep your knee straight while sitting, and avoid squatting.
Icing the knee for twenty minutes two to three times a day is recommended, especially after any sporting activities. Exercises can also be used to stretch and balance the thigh muscles.
It is advisable, however, to contact a physical therapist & approach proper physical therapy before you attempt any of these remedies, to avoid any further damage.
Happy Healing!
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Jumper’s knee can be a persistent issue for athletes, but physiotherapy can help by strengthening the knee, improving flexibility, and reducing pain. If you’re looking for professional physiotherapy services to treat jumper’s knee, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations provide expert care and customized treatment plans to help you recover and return to your sport stronger than ever.
What is ALS?
Amyotrophic lateral sclerosis (ALS) is the most common type of adult-onset motor neuron disease. Neurological disorders are characterized primarily by progressive degeneration and loss of motor neurons. ALS involves upper and lower motor neurons and presents as an idiopathic, progressive degeneration of anterior horn cells and their associated neurons, resulting in progressive muscle weakness, atrophy, and fasciculations.
What are the symptoms of ALS?
ALS is a gradual-onset disease. The first initial symptoms of ALS vary from person to person. One person may have trouble with their grip, such as holding a cup or pen, while another person may experience a change in pitch in their voice while speaking. The rate at which ALS develops also varies from person to person, with the mean survival time ranging from three to five years.
Although there are cases in which people have lived five, and ten or more years. Onset symptoms can begin in the muscles that control speech and swallowing, or in the hands, arms, legs, or feet. Not all people who suffer from ALS experience the same symptoms as others or the same sequences or patterns of progression. Although, universally progressive muscle weakness and paralysis are experienced.
How is ALS diagnosed?
ALS is a somewhat difficult disease to diagnose. There is not one test or procedure to instantly establish the diagnosis of ALS. Through the use of clinical examination, and a series of diagnostic tests, often ruling out other diseases that mimic ALS, that a diagnosis can be established. A comprehensive diagnostic check-list includes most, if not all, of the following procedures:
- Electrodiagnostic tests- Electromyography (EMG) and Nerve conduction velocity (NCV)
- Blood & Urine studies
- Spinal tap
- X-rays including MRI
- Myleogram of cervical spine
- Muscle and/or nerve biopsy
- A thorough neurological examination
These tests are done at the discretion of the physician, usually based on the results of other diagnostic tests and the physical examination. There are several diseases that have some of the same symptoms as ALS, and most of these conditions are treatable.
What are the treatments for ALS?
Treatment of ALS can be done with physiotherapy, focusing on stretching and daily range of motion (ROM) exercises. Our physiotherapists at Triangle will focus on the emphasis of energy conservation and teach patients and caregivers methods for performing safe, efficient transfers. They can also provide instruction for strengthening exercise programs.
In one study, individualized, moderate-intensity, endurance-type exercises for the trunk and limbs performed 15 minutes twice daily were shown to significantly reduce spasticity as measured by the Ashworth scale. At Triangle, we may have to recommend wheelchairs to anticipate the patient’s future needs. Initially, a lightweight wheelchair should be rented, with future plans to purchase a heavier chair when the patient is no longer able to ambulate. Modifications will be recommended on the basis of the patient’s condition and tolerance for gadgets.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Physiotherapy is a crucial component in managing ALS, helping to maintain mobility, reduce discomfort, and improve quality of life. For those seeking specialized physiotherapy services to support ALS management, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans tailored to the needs of individuals living with ALS.
Are you feeling a bit of a pain in the neck lately? Does your neck feel stiff, painful, tender, or are you not able to turn it and move around as much as you used to? You may be a victim of whiplash.
What is Whiplash?
Whiplash is most associated with traumatic events involving sudden acceleration-deceleration forces mainly on the neck. It can affect a variety of issues pertaining to your muscles, joints, bones, ligaments, discs, and nerves. Whiplash is mostly associated with car accidents, but other causes may include roller-coasters, bungee jumping, or a sports-related condition.

What are the symptoms of Whiplash?
Symptoms and severity of whiplash can vary significantly between people. The most commonly reported symptom is neck pain or stiffness. This can occur anywhere from immediately after the injury to several days after.
Symptoms may include:
- Neck pain or stiffness
- Headache
- Shoulder pain, arm pain, or upper back pain
- Dizziness
- Altered sensation
- Weakness
- Visual disturbances
- Hearing difficulties
- Difficulty speaking or swallowing
- Difficulty swallowing
How can Whiplash be treated?
Fortunately, most people recover from the pain and stiffness associated with whiplash in a matter of weeks, but some cases require longer recovery time and treatment from a physiotherapist. Healing time varies with the level of tissue damage and promptness of treatment. Most whiplash patients will start to feel better within a few weeks of the injury from physiotherapy treatment. At Triangle Physiotherapy, our physiotherapists will aim to:
- Reduce neck pain, headaches, and inflammation
- Normalise joint range of motion
- Gain strength in your neck
- Strengthen your upper back muscles
- Improve neck posture
- Normalize your muscles lengths and rest muscle tension
- Resolve any deficit in neural tissue extensibility
- Improve neck proprioception, fine motor control, and balance
- Improve your ability to cope with everyday activities
- Minimize your chance of future neck pain or disability
Whiplash injuries can take from a few days to several months to rehabilitate. Just as the symptoms and severity of whiplash can vary from person to person, so can the recovery time. The large majority of whiplash sufferers do recover with actively guided treatment. Depression and trauma-related anxiety may impact the healing process of whiplash. Please consult with a qualified health professional to give yourself the best chance of recovery.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Recovering from whiplash requires a comprehensive physiotherapy approach to restore mobility, reduce pain, and improve strength. If you are looking for professional physiotherapy services to help manage whiplash recovery, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide expert care and tailored treatment plans to help you get back to your normal activities safely and effectively.
What is incontinence?
Incontinence can be a fairly sensitive or embarrassing subject to those who suffer from it. Incontinence is the involuntary loss of urine or feces from the bladder and bowel. But know this, incontinence is an ACCIDENT, it is something that is uncontrollable and can happen to any expecting mother.
Urinary incontinence affects around 10-13 million men and women, and it is twice as common in women as in men. Anthony Atala, MD, said, “I would say virtually all pregnant women experience some type of incontinence”. Incontinence should not rule your pregnancy or your life.

What does pregnancy have to do with incontinence?
Pregnancy can interfere with the normal way your urethra relaxes and contracts. You are able to urinate when the muscles around your urethra relax, allowing urine to pass through your bladder and out of your body. After urination, the muscles around your urethra contract, holding off urine flow until your body is ready to urinate again. Hormone changes during pregnancy and the additional pressure on the bladder from your uterus can cause stress incontinence. Mothers who are experiencing stress incontinence may urinate whilst sneezing, walking, coughing, laughing, running, and during exercise. Women who have a family history of incontinence, gain more weight than recommended during pregnancy, and are over the age of 35 are at higher risk of experiencing incontinence.
How do I avoid incontinence during pregnancy?
There are numerous ways to avoid pregnancy incontinence, along with visiting a pelvic health physiotherapist, to avoid leakage.
- Schedule your bathroom breaks. Try to make it to the toilet at least every two hours, as when pregnant, women urinate more frequently.
- If you think your bathroom visits are proper, try practicing kegel exercises. Kegels help strengthen the pelvic floor. Practicing a kegel is the same as stopping the flow of urine within your urethra. Contract your muscles to the count of ten and then release. Repeat exercises ten to twenty times in a row two to three times a day. The average time to see results is four to eight weeks of regular practice.
- Watching your weight while carrying has a significant effect on developing incontinence. Women who gain more weight during pregnancy are more likely to experience incontinence. Combining these factors with your pelvic physiotherapist will lower your risk of developing incontinence during your pregnancy, allowing your experience to be worry-free.
If you are still unsure or worried about the risk of incontinence during your pregnancy, contact a pelvic floor physiotherapist at Triangle Physiotherapy. Triangle Physiotherapy has eight convenient locations: Etobicoke, Oakville, Mississauga, North York, Toronto, and King West. At Triangle Physiotherapy, our team is compromised of professionals who love what they do. Triangle staff will ensure that you will have a safe and comfortable pregnancy while in their care, and will help get your pregnancy back on track and in your hands.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Incontinence during pregnancy can be challenging, but physiotherapy can help manage symptoms and improve pelvic floor strength. If you’re looking for specialized physiotherapy services to support incontinence management, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and personalized treatment plans to help you stay comfortable and healthy throughout your pregnancy journey.