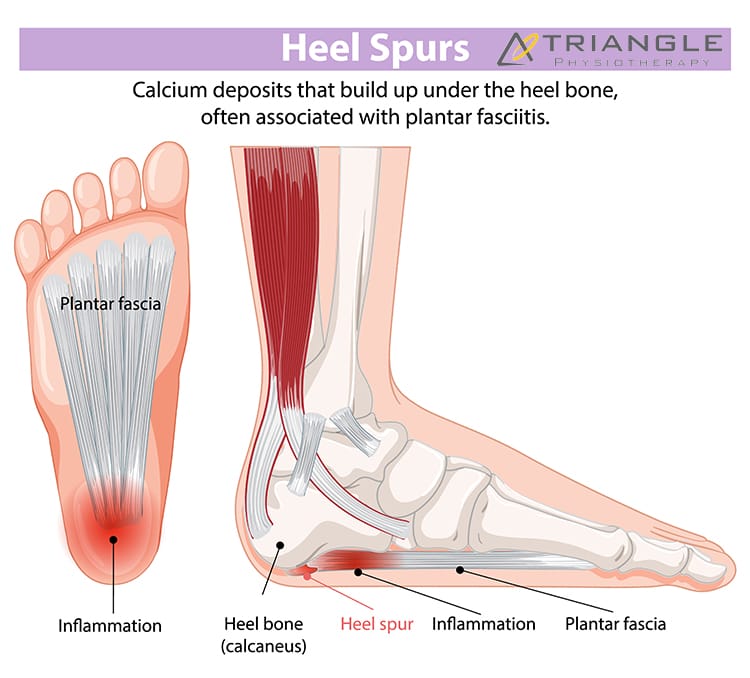
A heel spur is a bony protrusion that forms where the plantar fascia (a thick band of tissue running along the bottom of the foot) attaches to the heel bone. Heel spurs develop gradually over time due to repeated stress on the foot, which causes calcium deposits to accumulate in the affected area. Although many people with heel spurs don’t experience pain, others may feel sharp or aching pain, particularly when standing or walking.

If you have a heel spur, our physiotherapists at Triangle Physiotherapy can help!
What Causes Heel Spurs?
The primary cause of heel spurs is chronic strain and stress on the plantar fascia. Several factors can contribute to this, including:
- Overuse or excessive pressure on the foot: High-impact activities like running, jumping, or prolonged standing can increase the strain on the heel.
- Poor footwear: Wearing shoes that lack proper arch support or cushioning can put added stress on the heel and plantar fascia.
- Obesity: Carrying excess weight can strain the feet, leading to inflammation and potential heel spur formation.
- Flat feet or high arches: Both conditions can alter the mechanics of the foot and contribute to heel pain and spur development.
- Age: As we age, the fat pad that cushions the heel tends to thin, increasing pressure on the heel bone.
Common Symptoms of Heel Spurs
Heel spurs don’t always cause pain, but when they do, the symptoms can include:
- Sharp, stabbing pain: Most often felt in the morning with the first few steps, as the foot moves after resting overnight.
- A dull ache: This pain can persist throughout the day, especially after prolonged standing or walking.
- Tenderness: The bottom of the heel may feel tender to the touch, especially around the spur’s location.
- Swelling and inflammation: In some cases, the area around the spur may become swollen and inflamed.
Treatment for Heel Spurs
Thankfully, there are several treatment options available to alleviate the pain associated with heel spurs and help with recovery.
- Rest and Ice: Giving your foot time to rest and applying ice to the affected area can help reduce inflammation and relieve pain.
- Stretching Exercises: Stretching the calf muscles, Achilles tendon, and plantar fascia can help relieve tension and reduce heel pain. A physical therapist can recommend specific stretches.
- Shockwave Therapy: ESWT is a non-invasive treatment option for heel spurs, where high-energy sound waves are directed at the affected area to stimulate healing and alleviate pain associated with the heel spur.
- Orthotic Inserts: Custom or over-the-counter arch supports can help redistribute pressure on the foot and reduce strain on the heel.
- Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), like ibuprofen, can help reduce pain and swelling.
- Corticosteroid Injections: For more persistent pain, a doctor may recommend an injection to reduce inflammation and relieve discomfort.
- Surgery: In rare cases, when conservative treatments do not provide relief, surgery may be necessary to remove the spur or release tension on the plantar fascia.

Preventing Heel Spurs
Preventing heel spurs involves addressing the underlying causes. To avoid developing heel spurs:
- Wear supportive shoes with cushioning.
- Avoid overuse or excessive pressure on the feet.
- Maintain a healthy weight to reduce stress on the feet.
- Stretch before and after physical activity.
Conclusion
Heel spurs can be a painful and frustrating condition, but with the right treatment and preventive measures, most people can find relief and return to their normal activities. If you’re experiencing heel pain, it’s important to consult with a healthcare provider to determine the cause and develop an appropriate treatment plan. With the right care, heel spurs can be managed effectively, allowing you to walk and move comfortably again. Connect with us at Triangle Physiotherapy and we can get you started on your road to recovery from heel spurs!
What is Plantar Fasciitis?
Plantar fasciitis is an overuse injury. Accumulation of micro-damage leads to the degradation of the collagen fibers that make up the origin point of the plantar aponeurosis. This prevalent condition is the most common cause of heel pain. It is a common condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of your foot. Managing plantar fasciitis involves a combination of lifestyle changes, exercises, and medical interventions.
What are the risk factors for plantar fasciitis?
- Overpronation
- High-Arched Feet
- Leg-length Discrepancy
- Footwear
Here are five ways to manage plantar fasciitis:
- Stretching Exercises:
- Perform gentle stretching exercises for the Achilles tendon, calf muscles, and plantar fascia. Regular stretching can help alleviate tension and improve flexibility.
- Towel stretches, calf stretches, and wall stretches are beneficial for targeting the affected areas.
2. Night Splints:
- Wear night splints to keep the foot in a dorsiflexed position while sleeping. This helps stretch the plantar fascia and Achilles tendon, promoting healing and reducing morning pain.
3. Custom Orthotics
- For orthotics to successfully treat plantar fasciitis, they need to control overpronation and the motion of the first metatarsal head.
4. Supportive Footwear
- Choose shoes with proper arch support and cushioning to reduce strain on the plantar fascia. Avoid high heels and worn-out shoes.
- Consider orthotic inserts or custom-made insoles to provide additional support and stability.
5. Physiotherapy
- Consult with a physiotherapist who can guide you through exercises and techniques to strengthen the muscles around the foot and improve overall foot mechanics.
- Shockwave therapy has been known to show great results in the management of plantar fasciitis.
How do I book an appointment with a Physiotherapist near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
Managing plantar fasciitis effectively requires a combination of the right treatments and exercises. For professional support in addressing foot pain, consider physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, or Liberty Village. Experienced physiotherapists in these areas can provide personalized care plans to help you recover and stay active.
Shockwave therapy, also known as extracorporeal shock wave therapy (ESWT), is a non-invasive medical treatment that uses acoustic waves to stimulate healing in various musculoskeletal conditions, including plantar fasciitis. Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes.

Here’s how shockwave therapy is typically used for plantar fasciitis:
- Mechanism of Action:
- Shockwave therapy works by delivering high-energy shockwaves to the affected area. These shockwaves create microtrauma in the tissue, which triggers the body’s natural healing response.
- The treatment is thought to stimulate blood flow, promote tissue regeneration, and reduce inflammation.
- Procedure:
- During the procedure, a gel is applied to the skin of the affected foot to help transmit the shockwaves.
- A handheld device is then used to deliver controlled shockwaves to the targeted area, typically the heel or the sole of the foot.
- Number of Sessions:
- The number of shockwave therapy sessions required can vary.
- Some individuals may experience relief after just one session, while others may require additional treatments.
- Post-Treatment:
- After the procedure, patients may experience temporary soreness or discomfort, but this usually subsides within a few days.
- It’s important to follow any post-treatment instructions provided by the healthcare provider, which may include rest, ice, and avoiding certain activities.
- Effectiveness: The use of shockwave therapy is often considered when conservative treatments, such as rest, stretching exercises, orthotics, and anti-inflammatory medications, have not provided sufficient relief.
It’s crucial to note that while shockwave therapy may be beneficial for some individuals, it may not be suitable for everyone. Patients should consult with their healthcare provider to determine the most appropriate treatment approach based on their specific condition and medical history.
Who can provide Shockwave Therapy at Triangle Physiotherapy?
Shockwave Therapy can be provided at our clinics by a physiotherapist, a chiropractor or a massage therapist.
Will Shockwave Therapy be covered by my insurance?
Yes, shockwave therapy will be covered depending on the healthcare practitioner providing the service. For example, if you are seeing a physiotherapist for shockwave therapy, it will be covered under your physiotherapy coverage.
How do I book an appointment with a physiotherapist or chiropractor near me?
Click HERE to book an appointment with a physiotherapist or chiropractor at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Shockwave therapy is an effective treatment for plantar fasciitis, helping to reduce pain and promote healing. Triangle Physiotherapy provides expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our skilled physiotherapists are here to help you find relief from plantar fasciitis and get back on your feet.”
Yes, a physiotherapist can definitely help with plantar fasciitis. They can provide specialized exercises, stretching techniques, and other treatments to alleviate pain, improve mobility, and promote healing of the plantar fascia.

What is plantar fasciitis and what causes it?
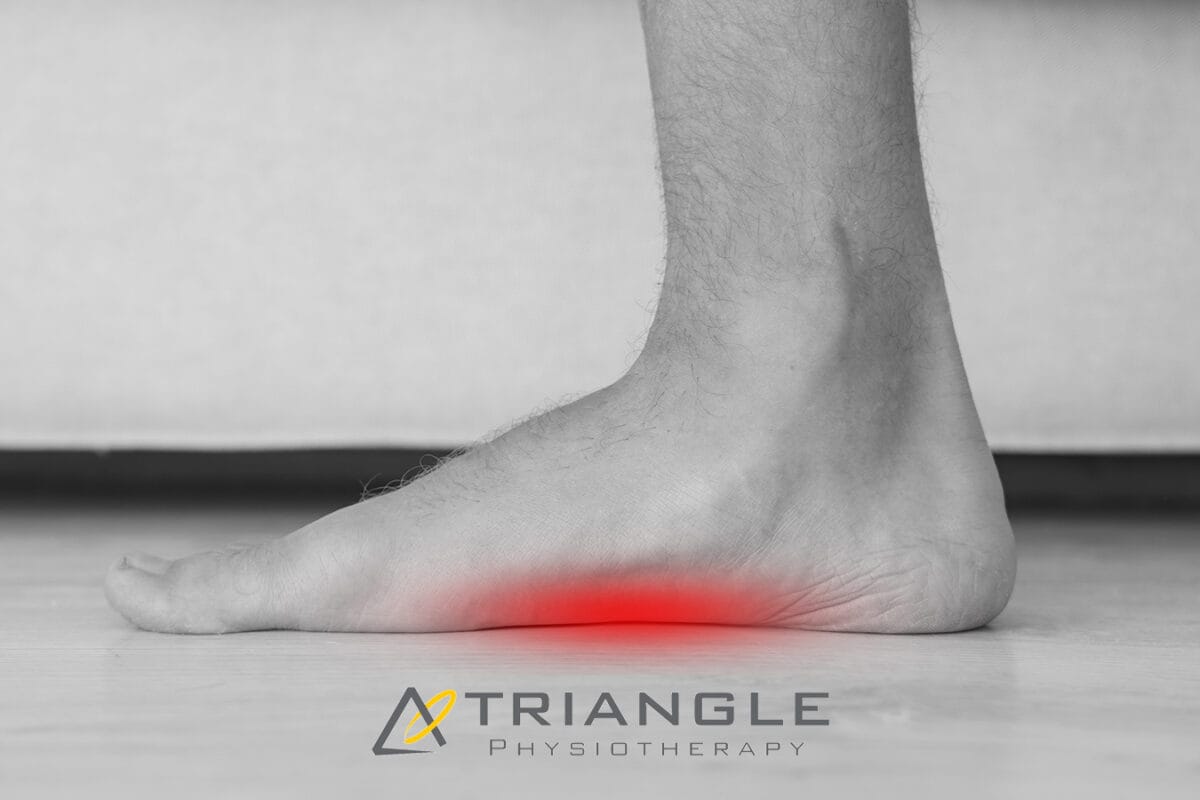
Plantar Fasciitis is a painful condition resulting from inflammation of a band of connective tissue located on the bottom side of the foot known as the Plantar Fascia. This band of connective tissue runs from the heel of the foot, all the way to the base of each toe, and it functions to support the arch of the foot, especially during weight-bearing.
What are the symptoms of plantar fasciitis?
The pain associated with Plantar Fasciitis is located on the bottom of the foot, with it often manifesting around the heel and along the inside of the foot. It is common for this pain to be at its worst first thing in the morning, and it is usually accompanied by other symptoms, such as stiffness, weakness, swelling, and decreased proprioception.
How is it diagnosed by a physiotherapist?
A Physiotherapist will run a thorough examination of the problem to ensure a proper diagnosis is obtained. This will include getting a detailed history, observing the area and how you function, and running through a series of specific tests. From there, an individualized treatment plan will be made for you to help you achieve your goals and assist you on your road to recovery.
Who is the most at risk to develop this condition?
Plantar Fasciitis is more common in people who can relate to the following:
- Have flat feet or high arches
- Have tight calf muscles
- Wear improper footwear
- Engage in repetitive physical activity (overtraining)
- Suddenly changed activity levels (increased frequency, duration, or intensity)
- Suddenly changed activity or training environment
- Work in an environment that requires prolonged standing
What is the best treatment for plantar fasciitis?
Physiotherapy is considered to be very effective in treating plantar fasciitis. The treatment starts with managing the initial pain and symptoms after which the soft tissue is gradually loaded to promote strengthening so that the condition does not reoccur.
What does plantar fasciitis treatment look like?
Plantar Fasciitis treatment can include one or more of the following:
- Rest: Avoid activities that worsen the pain and give your feet time to heal.
- Ice: Applying ice to the affected area can help reduce inflammation and pain.
- Stretching: Regularly perform calf and foot stretches to help improve flexibility and reduce tension on the plantar fascia.
- Footwear: Choose supportive and cushioned shoes that provide proper arch support.
- Orthotics: Custom or over-the-counter shoe inserts can help distribute pressure evenly on the foot.
- Night splints: These devices keep the foot in a stretched position overnight to alleviate morning pain.
- Physiotherapy: A physiotherapist can guide you through exercises and treatments to aid recovery.
- Extracorporeal Shock Wave Therapy (ESWT): In some cases, this treatment may be used to stimulate healing.
Click HERE to book an appointment with a physiotherapist at one of our eight locations.
- Physiotherapy Etobicoke – Triangle Physiotherapy Etobicoke
- Oakville Physiotherapy Clinic – Triangle Physiotherapy Oakville
- Physiotherapy North York – Triangle Physiotherapy North York
- Mississauga Physiotherapy Clinics – Triangle Physiotherapy Mississauga
- Downtown Physiotherapy Clinics – Triangle Physiotherapy King West
- Uptown Physiotherapy Clinics – Triangle Physiotherapy Lawrence Park
- Physiotherapy Clinic Downtown Toronto – Triangle Physiotherapy Queens Quay
- Physiotherapy Clinics Mississauga – Triangle Physiotherapy Erin Mills
“Plantar fasciitis can be effectively managed with the help of a skilled physiotherapist. Triangle Physiotherapy offers expert care across the GTA, including Physiotherapy in Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. Our experienced team can develop a personalized treatment plan to alleviate your symptoms and help you get back on your feet.”
Re: Kevin Durant’s mid-game calf strain
Kevin Durant, Durantula, easymoneysniper, whatever you want to call him is a superstar basketball player and is regarded by many as the second-best basketball player in the world. Unless you have been living under a rock in Toronto, you should know his name and the impact of his eventual return to the NBA Finals. Moreover, if you’re a therapist like me, you may feel disgusted about the mismanagement of his return to the court on Monday.
Here are the facts:
- Kevin Durant was diagnosed with a right calf strain on May 8th, 2019, which many suspected was an Achilles strain to begin with. Grade 1 Calf Strain can take anywhere from 7-10 days to resolve. Durant was out for a whole month!
- Kevin Durant was cleared for practice on June 9th and he did so with his teammates (unsure of the extent of this practice as it was closed off to the media)
- After his practice, Kevin Durant is noted leaving practice with a slight limp and ice on his right Achilles (to help with possible pain/inflammation?)
- A few hours before tip off he is upgraded to questionable to play in game 5 of the NBA finals, and 90 minutes before tip off it is known that he is cleared to play and will start in game 5, with no minutes restriction. WHAT?
- Kevin Durant does indeed start game 5, and starts off hot connecting on his first 3 attempts beyond the arc and scoring 11 points in the first quarter.
- At 9:46 of the second quarter, Durant came up the court and tried to accelerate past Ibaka with his right foot planted, and that was enough. Durant fell to the ground holding his right Achilles.
- Teammates and opposing players help him back to the locker room, and post game Durant is seen leaving the Scotiabank Arena in a walking boot and crutches
- Durant is expected to fly to New York to have an MRI done, which many believe will confirm a right ruptured Achilles.
Also read, Physiotherapy Rehab Clinic in Mississuaga
What is an Achilles Tear/Rupture and what does it mean for Durant?
The Achilles tendon is the largest tendon in the body. It connects your calf muscles to your heel bone and is used when you walk, run, and jump.
Achilles tendon ruptures can occur spontaneously in individuals and one symptom many people display is the pop or gunshot sound of their Achilles tendon rupturing. If you look in the video above, you can notice the pop of the Achilles and the subsequent vibration of the calf muscles accordingly.
Detailed in an article by Physio Works it states:
Achilles Ruptures occur mostly in middle-aged men, most of whom play recreational sports Injury often occurs during recreational sports that require bursts of jumping, pivoting and running.
They can happen in these situations:
- You make a forceful push-off with your foot while your knee is straightened by the powerful thigh muscles. One example might be starting a foot race or jumping.
- You suddenly trip or stumble, and your foot is thrust in front to break a fall, forcefully overstretching the tendon.
- You fall from a significant height.
Also read, Physiotherapy Rehab Clinic in Etobicoke
The biggest risk factor for Achilles tendon rupture is tendon cell death which occurs as a result of poorly managed tendinopathy.
As noted in the bold statements, these are the exact scenarios which led to the possible tendon rupture for Kevin Durant, with strong emphasis on the second statement!
While we don’t know the extent of Kevin Durant’s Achilles tear, we can only speculate that it is a complete rupture and thus provide this comparative timeline on his return to that of another NBA player, Rudy Gay, who tore his Achilles in 2017 at the same age, and has the body frame similar to that of Durant.
If the MRI on Tuesday confirms a complete tear and Durant follows a similar timeline to that of Gay
- Durant will undergo surgery to repair the tendon
- He will be on crutches and in a boot for the next six weeks.
- He will start physical therapy in two weeks and formal rehabilitation at eight weeks post-surgery.
- >12 weeks post he can begin sport specific training
- Return to sport is anticipated in 6 months
Now if Kevin Durant is able to follow the same path as Rudy Gay, what are the implications to his career? He was a free agent this year hoping to be signed to a max contract with the team of his choosing as every team salivated at the idea of signing him (Brooklyn, Knicks to name a few). Will teams take that gamble anymore? It’s Kevin Durant, so I am sure they will. Yet, he may be forced to stay in Golden State another year as he returns to the court to prove that he isn’t damaged goods. Keep in mind, numerous athletes in the past were never the same after facing a similar injury. Kobe is one that comes to mind, and this ultimately led to his retirement. Currently we see the same with Durant’s teammate Demarcus Cousins who went from being an all-star to a bench caliber player. Moreover, Rudy gay was quoted as saying that it took him almost a full year and a half to feel 100% again. Which scenario will apply to Durant? How long, if ever, will it take for him to be truly 100% again, as he sits in the prime of his career? All valid questions probably going through Kevin Durant’s head as he awaits his MRI results on Tuesday.
Also read, Physiotherapy Rehab Clinic in Oakville
Moreover, as we await the results of the MRI, I also question the doctors, therapists, and ownership of the Golden State Warriors on making the decision for Kevin Durant to return to Game 5. I get that the athlete has the final say as to whether they want to play or not (Kawhi Leonard comes to mind here ironically), but considering the immense amount of pressure put on Durant to help the Warriors avoid upset, and amplify his legacy, one can only point the finger at the medical and management team for allowing him to go out there. He was clearly still nursing a calf strain (and/or possible grade 1 Achilles strain). He was clearly not pain-free, nor was he recovered from a metabolic and vascular standpoint in that calf to Achilles region. So, was the chance at a three-peat really worth risking the health and career of one of the best players in the league?
I guess now that we know the outcome of that decision, all members involved will have to carry that guilt. Just remember therapists, don’t lose your credibility as a health care practitioner with unrealistic outcomes for some championship trophy, financial gain, or anything to inflate your ego. Always do what you clinically know is right for your client, and PLEASE educate patients that no pain no gain is not a real motto.
Recovering from a calf strain or any sports injury requires proper physiotherapy to ensure safe and effective healing. If you’re looking for expert physiotherapy care, clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village offer specialized treatment plans to help athletes and individuals recover fully and prevent future injuries.
Our feet are likely the most used body parts of all of our limbs. Be it sitting or standing, we are always using our legs in one way or the other. In fact, the use of our feet and legs usually begins the moment we wake up. So it is safe to say that our feet play a vital role in our day-to-day life and as such, it is important to take good care of them. Our feet carry the entire weight of our body throughout the day. They undergo tremendous pressure with every step we take as they get compressed and endure repeated movement against our footwear. Over a period of time, pressure on certain parts of the foot can increase and the body compensates by adding extra layers of scar tissue and skin on parts of feet that undergo high pressure, such as the ball and heel & toes of the foot. This can cause there to be painful areas of pressure on the foot or the formation of callouses on areas of higher pressure on the foot.

Also read, Best Physiotherapy Clinic in Etobicoke
Why schedule an appointment with a Chiropodist?
Walking, running, sitting – everything involves your legs. A minor injury or pain can cause huge discomfort in your everyday life and can escalate to become a serious issue. For example, an ingrown toenail or an infection can be very painful and uncomfortable. Seeing a Chiropodist at an earlier stage will help immensely in preventing and managing these kinds of foot-related problems.
An appointment with a Chiropodist will involve a thorough assessment of your foot-related problem and treatment that will help alleviate the problem. Even without a significant ongoing foot issue, a visit to the Chiropodist can help you in preventing one from developing by gaining more insight into your walking pattern or providing education on correct foot care. They are trained to diagnose and treat a wide variety of foot-related conditions and are able to understand their patient’s needs in order to prevent and treat both acute and chronic conditions that involve the foot and lower limb functions.
Also read, Best Physiotherapy Clinic in Oakville
What do we treat at Triangle Physiotherapy?
Our Chiropodist is a highly skilled professional that is an expert in their field. At Triangle Physiotherapy, our registered Chiropodists diagnose, assess, and treat a wide range of foot-related health issues and abnormalities including but not limited to:
- Alignment and support to prevent or correct abnormalities in the lower limbs
- Abnormal gait patterns
- Foot pain
- Sports injuries
- Diabetic foot care
Also read, Best Physiotherapy Treatment in Mississauga
How to Contact Triangle Physiotherapy?
We have 8 clinics located across the GTA: Etobicoke, Oakville, Mississauga, North York, and Toronto (King Street West, Queens Quay, and Yonge Street. If you have any questions regarding what type of chiropody treatment may be appropriate for you, please call or email us and we will be happy to answer your questions. You can also Book an Appointment with a Chiropodist now.
Chiropodists play a vital role in managing foot and lower limb conditions, often collaborating with physiotherapists to provide comprehensive care. If you’re looking for professional physiotherapy services to complement chiropody care, consider clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and personalized treatment plans to help you achieve optimal foot health.
Acupuncture is a healing technique used in TCM where practitioners stimulate specific points on the body, most often by inserting thin, sterile needles into the skin.
Acupuncture mainly focuses on correcting imbalances of energy in the body & improves the body’s function by promoting the natural, self-healing process. It is now widely practiced as a therapeutic intervention in North America, in addition to Asia.

What can acupuncture help with?
The most common method used to stimulate acupuncture points or acupoints is the insertion of fine, sterile needles into the skin. This technique can release blocked Qi in the body and stimulates the body’s natural healing response through various physiological systems. Studies suggest that acupuncture can ease various types of pain generated by conditions such as:
- Low-back pain
- Neck pain
- Knee pain
- Osteoarthritis
- Headaches
- Migraine
- Depression
- Rheumatoid arthritis
- Smoking addiction
- Chronic asthma
- Epilepsy
- Insomnia
Also Read, Physiotherapy Etobicoke
How many treatments will I need?
The frequency of treatments differs from person to person based on their health condition. Some people experience relief in the first treatment itself, whereas others with complex or long-standing chronic conditions may notice more of a significant benefit after multiple treatment sessions. Generally, fewer treatments are required for acute conditions and more treatments are required for chronic conditions. An individualized treatment plan that includes the expected number of treatments will be discussed during the first visit.
In recent years, acupuncture has gained much more traction in Western Medicine. The majority of research on the use of acupuncture in Western Medicine has focused on its use for pain management and inflammation reduction. Thus far, the majority of this research has yielded positive results, indicating that acupuncture is indeed a useful technique for pain management and inflammation reduction.
Our More Locations
Physiotherapy Etobicoke | Physiotherapy Oakville | Physiotherapy North York | Physiotherapy Toronto | Physiotherapy Lawrence Park | Physiotherapy Mississauga | Physiotherapy Queens Quay | Physiotherapy Mississauga Erin Mills | Physiotherapy Liberty Village
At Triangle Physiotherapy, our practitioners and therapists will thoroughly assess your past medical history and will answer any questions that you might have about your condition. This New Year, make sure that you focus on your health to ensure that you have a productive and healthy year!
Acupuncture can be an effective treatment for pain relief, stress management, and promoting overall wellness. If you are looking for physiotherapy services to complement acupuncture, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer comprehensive care with personalized treatment plans to help you achieve optimal health and recovery.
Are your worries all perched on a pillow? And we don’t mean figuratively, but literally, are your worries all about THE PILLOW? Well, you are not in as uncommon a dilemma as you may think. Physiotherapists frequently get queries about pillow-related problems.
Sleeping on the wrong pillow, or one that is too worn out, not only leads to headaches, backaches, and neck cramps but also prevents you from getting a good night’s sleep. Lack of proper sleep can lead to many serious health issues, like obesity, heart disease, diabetes, etc.
It is imperative that you choose the right pillow for yourself but the kind of pillow you should pick will depend on your own unique needs as well. A physiotherapist is the best person to tell you exactly what you need. However, here are a few things that you can keep in mind while making a choice –
- Your usual sleeping position
- The shape and size of your head, neck and back
- Desired softness/firmness of the pillow
- Any neck pain, or backache you may have
- And your budget

Also read, Physiotherapy Clinic in Mississauga
There are a plethora of pillows in the market – cotton, polyester, feather, down, memory foam etc. However, these don’t cater to specific support or pain needs. If you have been injured, or have a particular condition, you will need a pillow that caters best to not just your problem, but also the stage that you are in. There are three main stages –
- Accommodation
- Correction
- Maintenance
For each of these three stages, you will need a specific kind of pillow.
Accommodation Stage:
Specialty pillows that are designed for the ‘Accommodation’ stage, are pillows that bring in comfort and ease by providing support and stabilizing the existing ailment or disorder. Such pillows are often called Displacement pillows and are often recommended by physiotherapists for short-term pain relief after an injury.
Correction Stage:
The next stage of an issue or injury is ‘Correction’. At this stage, a doctor or physiotherapist attempts to find a remedy for the cause of the problem, and thereby correct it. Pillows recommended in this stage are often designed to provide support, and sometimes to even change the sleeping position of the injured or ailing person. There are various ‘Supportive’ pillows to meet different support levels, firmness and neck lobe size needs of different patients. There are also specialized ‘Corrective’ pillows, which can reduce headaches, neck pain, joint pain, and whiplash discomfort and can even improve nerve function. A physiotherapist can tell you what is the ideal Supportive or Corrective pillow you need, based on your health and body needs.
Also read, Physiotherapy Clinic Oakville
Maintenance Stage:
Pillows for the last stage, ‘Maintenance’, help to promote good health by returning and keeping the body in its natural alignment. At this stage maintaining the normal curvature of the neck and spine is of utmost importance. While the normal curvature of one person’s neck and spine may differ from another, there are some general guidelines that a physiotherapist can jot down to help you understand your needs better. Comfort and support are the most important of these.
There are also Aqua pillows, which perform all the 3 functions of a pillow:
- Accommodation: Since water is fluid, a person gets customized accommodation that happens in real time, as the individual changes their position on the pillow.
- Correction: The volume of water determines the firmness and density of the pillow, which means different amounts of water can be utilized to help correct the neck position of different people in different stages of healing.
- Maintenance: Since the volume of water remains constant until changed manually, it helps maintain the neck posture at all times while sleeping.
A lot of people buy a pillow, try it for a few nights, and then feel it isn’t right for them. Sometimes the pillows can be returned, but more often, people end up having a collection of pillows that they have hardly ever used. An Aqua pillow is a huge savior in this aspect, as it can be customized for each individual! The water levels can be modified to best suit the clinical condition, neck shape, and size, and preferred sleeping position of the buyer.
There are also specially designed Orthopaedic pillows for specific conditions like arthritis, fractures, and slip discs. A physiotherapist can enlighten you more about these.
Seek the help of our professionals at any of our locations in Etobicoke, Oakville, North York, Mississauga & Downtown Toronto, and say goodbye to your pillow problems!
Proper posture and support are essential for preventing discomfort and maintaining spinal health. For those seeking professional physiotherapy services to address posture-related issues, consider visiting clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics offer expert care and tailored treatment plans to help you improve your posture and overall well-being.
Who doesn’t want to stay flexible, especially as they age? Well, stretching is one very good way to stay flexible! According to the American College of Sports Medicine, it’s good to stretch all the major muscle groups at least two times a week. Stretching is an integral part of physiotherapy, and a physiotherapist is the perfect person to guide you on how to stretch. Physiotherapists recommend stretching regularly, as it keeps one’s hips and hamstrings flexible later in life, which is very important for easy movement in old age.
Apart from this stretching has many other benefits:
- It increases muscle flexibility
- It improves posture
- It also improves performance in sports & other activities
- It provides relief from stress
- It helps prevent injuries
- It prevents Delayed Onset Muscle Soreness or DOMS, which is the soreness and pain one suffers a few hours to a few days after hectic exercise.
Also read, Physiotherapy Etobicoke

The first question that many wonder about, is what body parts should one stretch.
In physiotherapy, stretching the following body parts is considered essential –
- Neck
- Jaw
- Upper Back
- Shoulders
- Triceps
- Biceps
- Wrists
- Quadriceps
- Calves
- Hamstrings
- Hips
- Groin
The next thing to take into consideration is if there is the right amount of time to stretch. While there is no particular amount of time that physiotherapists suggest you stretch, recent studies show that 3 sets of 30-second stretches, 5 days per week for 4 weeks help to strengthen hamstring muscles greatly.
Also read, Physiotherapy Treatment Oakville
There are many kinds of Stretching that physiotherapists recommend.
Stretching a muscle to its full extent and holding it for 15 to 30 is known as the Static Stretch. You can exceed this time frame a bit but don’t stretch until it hurts, as you can end up doing more damage to your muscles than good by over stretching. However, don’t do Static Stretches before a run or sprint, as this can slow down your speed by tiring out the muscles.
Before warming up for a run or other sports, doing Dynamic Stretches is more suitable. Dynamic Stretches are stretches that you do, as you are moving, and hence are called dynamic.
Another effective way of stretching, often used in physiotherapy, is Proprioceptive Neuromuscular Facilitation (PNF) Stretching.
PNF stretching is an advanced type of stretching wherein the targeted muscle or muscle group, is stretched, contracted, and finally relaxed. This process is repeated at least 2 to 4 times before moving on to the next muscle group. PNF stretching helps to elongate one’s muscles and was first developed as a muscle therapy by athletes, but is now often used in physiotherapy as a means of increasing flexibility.
Stretching can be used as a preventative precaution, but also to help correct and recover from more serious issues. A physiotherapist can guide you more regarding the stretching exercises that will be best suited to your needs. So visit any of our locations in Etobicoke, Oakville, North York, Mississauga & Toronto, and find out how you can get the most out of stretching!
Stretching with physiotherapy can help improve flexibility, prevent injuries, and enhance overall physical performance. If you’re looking for professional physiotherapy services to guide you in safe and effective stretching techniques, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These clinics provide expert care and personalized treatment plans to help you achieve your mobility and wellness goals.
Summer is here, and with the sun on one’s face and a cool breeze, everyone feels like going out and enjoying some fresh air. Be it an early morning run or a quick swim, a game of tennis with your buddies or you just dribbling the ball all by yourself at the basketball court; this is the season when even the lazy ones find some energy to be active. Kids in particular love to go out and play in the summers. But with an active lifestyle, or an energetic kid, there is always the chance of sports-related injuries or foot fatigue.
Maybe you twisted your ankle while playing tennis? Or did your kid get hurt while playing football? Maybe too much running is affecting your feet? Or your friend is having pain in his or her legs post-cycling?
Also read, Physiotherapy Clinic in Etobicoke
Orthotics might just be the answer to your woes!

The type of Orthotics recommended to you will depend on not just your ailment or injury, but the shape of your feet as well. A physiotherapist can tell you what kind of orthotics you need, by evaluating your injury and the shape of your feet.
The most popular kind of Orthotics include:
- Casual Orthotics – These are inserts or pads that can be worn with regular shoes.
- Custom Orthotics – these are inserts that are specially designed, keeping the shape of your feet and your particular needs in mind.
- Sports Orthotics – these are inserts or pads that help to absorb shock while doing high-impact activities. Be it running, jogging, cycling, or playing a sport. There are even specialized Orthotics that slip easily into athletic shoes for professional athletes.
- Dress Orthotics – These are inserts that can be put into heels and other fashionable shoes, and are particularly made for women.
- Accommodative Footwear – this refers to special footwear, which can accommodate the Orthotics.
Also read, Physiotherapy Oakville
If you don’t have a sports injury but are just very active, orthotics can still come to your aid. But do seek your doctor’s advice before using any kind of orthotics.
At Triangle Physiotherapy our health professionals cater to your needs and specifications. With the help of our professionals, you can figure out what is the best solution for you, based on your activities and the needs of your feet. So visit any of our locations in Etobicoke, Oakville, North York, Mississauga & Downtown Toronto, to stay active with Orthotics!
Orthotics can be crucial for active individuals looking to prevent injuries and enhance performance. If you need professional physiotherapy services to complement your orthotic treatment, there are clinics in physiotherapy Etobicoke, Oakville, North York, Toronto, Lawrence Park, Queens Quay, Erin Mills, Mississauga, and Liberty Village. These locations offer expert care and personalized treatment plans to support your active lifestyle and overall foot health.